Case Report - Interventional Cardiology (2017) Volume 9, Issue 3
Early lotus transcatheter aortic valve thrombosis
- Corresponding Author:
- Gökhan Ertas
Department of Cardiology, Dr. Siyami Ersek Thorcic and Cardiovascular SurgeryTraining and Research Hospital, Istanbul, Turkey
Tel: 02164189610
Fax: 02163379719
E-mail: drgokhanertas@yahoo.com.tr
Submitted: 05 April 2017; Accepted: 16 May 2017; Published online: 22 May 2017
Abstract
Valve thrombosis is an important problem of surgical valves and also newer generation transcatheter valves. Valve thrombosis has been reported in different transcatheter valves, such as Edwards and Corevalve valves. Valve thrombosis after Lotus valve implantation has not been reported. To the best of our knowledge, this is the first report in the literature of a Lotus valve thrombosis. The patient discharged home on aspirin and clopidogrel after procedure, however she became symptomatic soon and the diagnosis of prosthetic valve malfunction due to thrombosis was made. Patient treated with anticoagulant therapy.
Keywords
Aortic valve thrombosis
Case Report
A 86 years old female patient was referred to our hospital due to severe aortic stenosis. Patient was suffering from dyspnea and chest pain. Transthoracic echocardiography (TTE) revealed a concentric hypertrophic left ventricle with preserved left ventricular ejection fraction (EF 55%) and a severely calcified aortic valve with a maximum pressure gradient (PG) of 77 mmHg and a mean PG of 47 mm Hg. Aortic valve area (AVA) indexed by body surface area was 0.6 cm2/m2. Preprocedural coronary angiography revealed nonstenotic coronary atherosclerotic plaque. The EuroSCORE II was 2.15% and the STS score for mortality was 1.11%. The heart team decided to perform transcatheter aortic valve implantation (TAVI) despite of low STS and EuroSCORE because patient was very fragile.
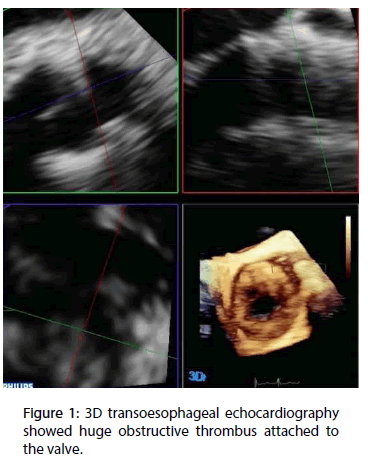
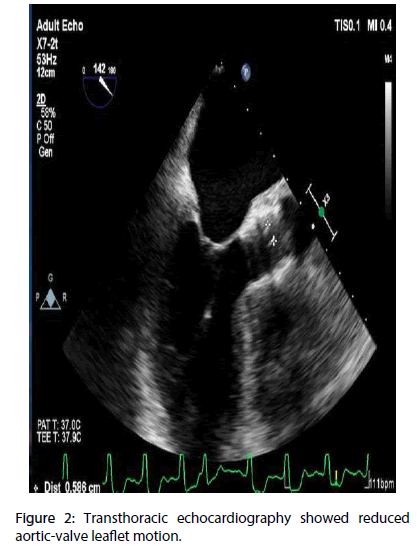
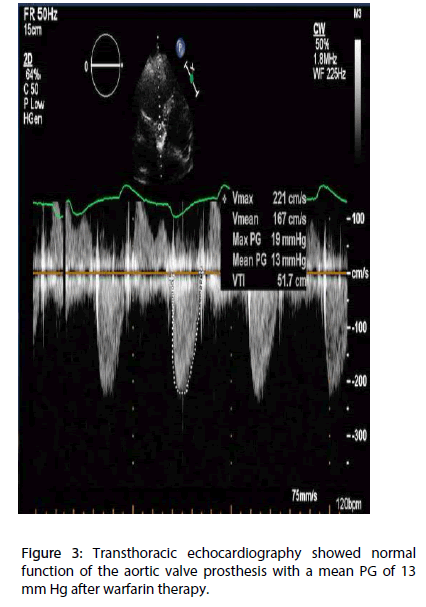
We decided to implant a self-expandable stent which we have experienced most, so patient had successful implantation of a 23 mm Lotus valve bioprosthesis (Boston Scientific, Natick, Massachusetts). After an uneventful postoperative period, the patient was discharged on day 3 on 100 mg aspirin and 75 mg clopidogrel and advised to stop the clopidogrel after 3 months. Discharge TTE showed normal function of the aortic valve prosthesis with a mean PG of 15 mm Hg and no paravalvular regurgitation. Two months after TAVI the patient suddenly became symptomatic, with dyspnoea (New York Heart Association [NYHA] functional class III). TTE revealed reduced aortic-valve leaflet motion, a mean PG of 56 mmHg, and an AVA (2D planimetry) of 0.7 cm2 these findings were confirmed by a transoesophageal echocardiography (TEE). 3D TEE revealed huge obstructive thrombus attached to the valve (Figures 1 and 2). Warfarin therapy was started to achieve a target INR of 2.0 to 3.0. After 40 days, patient was totally asymptomatic and control TTE revealed normal function of the aortic valve prosthesis with a mean PG of 13 mmHg (Figure 3).
Figure 2: Transthoracic echocardiography showed reduced aortic-valve leaflet motion.
Figure 3: Transthoracic echocardiography showed normal function of the aortic valve prosthesis with a mean PG of 13 mm Hg after warfarin therapy.
Discussion
Dual antiplatelet therapy (DAPT) is currently recommended after TAVI, oral anticoagulation has been advised only in special conditions. Valve thrombosis occurs more often in mechanical prostheses, bioprosthetic surgical aortic valve thrombosis has been reported with a incidence of 0.18% [1].
Retrospective multicentre study reported valve thrombosis after transcatheter aortic valve implantation with a incidence of 0.61% [2]. Latib et al. has reported that most of valve thrombosis occcured in the first year after implantation [2].
The optimal duration of anticoagulant therapy after valve thrombosis is unknown. Direct visualization of thrombus is a highly specific finding but it is not seen all cases. Valve thrombosis should be suspected if elevated transvalvular gradients are obtained. Also, computed tomography imaging and transesophageal echocardiography may be useful to support the diagnosis of thrombosis, however if direct visualization of thrombus could not be seen, reduced bioprosthetic aortic valve leaflet motion may be a sign of thrombus.
In summary, consider valve thrombosis in case of clinical symptoms and high Doppler gradient, even if thrombus could not be seen. A trial of a warfarin therapy should be considered before a valve-in-valve procedure.