Review Article - Imaging in Medicine (2009) Volume 1, Issue 2
ECG-gated multidetector-row computed tomography in the assessment of left ventricular function
Marco Rengo†, Paola Lucchesi, Carlo Nicola de Cecco, Pasquale Paolantonio, Riccardo Ferrari & Andrea LaghiDepartment of Radiological Sciences, Sapienza University of Rome, Polo Pontino, I.C.O.T., Via Franco Faggiana 34, 04100 Latina, Italy
- Corresponding Author:
- Marco Rengo
Department of Radiological Sciences
Sapienza University of Rome, Polo Pontino
I.C.O.T., Via Franco Faggiana 34, 04100 Latina, Italy
Tel: +39 077 365 1307
Fax: +39 077 348 9403
E-mail: marco.rengo@gmail.com
Abstract
Keywords
DS CT ▪ image reconstruction ▪ left ventricular function ▪ MDCT ▪ MDCT technique ▪ MRI ▪ multidetector-row computed tomography
The evaluation of cardiac function can provide important diagnostic and prognostic information in many diseases that have an impact on the performance of the pump activity of the heart. The assessment of cardiac function, in an accurate and reproducible way, is crucial in determining the severity of cardiac impairment and the efficacy of treatment [1]. For several years, investigators have explored different strategies to quantify global and regional cardiac performance using a variety of techniques. With the availability of noninvasive cardiac imaging modalities such as echocardiography and cardiac scintigraphy, assessment of cardiac function became part of routine clinical examination [2]. In particular, for the clinical work-up of patients, echocardiography is still the most used technique to determine left ventricular (LV) volumes [3]. However, its measurements rely on geometric assumptions about ventricular structure. Cardiac MRI provides excellent temporal and spatial resolution, allows image acquisition in any desired plane, and has a high degree of accuracy and reproducibility concerning quantitative measurements. In addition, MRI can be used to measure LV volume, without assumptions regarding LV cavity geometry. Thus, MRI is currently considered a reference standard in assessment of cardiac function [4]. The advent of multidetector computed tomography (MDCT) has provided a new opportunity for cardiac imaging; with submillimetric collimation and a faster gantry rotation it allows the acquisition of the entire heart volume in a single breath-hold with excellent temporal and spatial resolution. Moreover, data acquisition in spiral MDCT, using a retrospective ECG gating, is continuous and provides information for any phase of the cardiac cycle. Thus, end-systolic and end-diastolic images can be produced to assess ventricular volumes and function. Consequently, MDCT is becoming an attractive option for the assessment of ventricular function, and not only for the evaluation of coronary artery obstruction [5]. This ability to provide both anatomical and functional information may significantly alter future practice within cardiology.
In this article, we aim to discuss the role of MDCT for the evaluation of cardiac function and evaluate its current clinical applications.
Global ventricular volumes & function
Assessment of global ventricular function means measuring the adequacy of the ventricles to eject blood into the vessels. Since the ventricles exhibit a repetitive process of ejection and filling, the filling process must be considered part of the global ventricular performance. In clinical routine, only the ventricular volumes at maximal filling (end diastole) and maximal emptying (end systole) are usually quantified. From these two volumetric parameters, end-diastolic volume (EDV) and end-systolic volume (ESV), all other global functional parameters can be deduced. Subtracting the ESV from the EDV provides the stroke volume (SV). The SV divided by the EDV multiplied by 100 gives the ejection fraction (EF) in percent. The EF describes the relative change of EDV to ESV and reflects the global ventricular function: the normal left ventricle ejects 50–70% of the EDV during systolic contraction. The SV multiplied by the heart rate gives the cardiac output. It is evident that the reliability of the deduced global ventricular parameters is only as good as the accuracy by which the EDV and ESV are determined [6]. Another important parameter of global ventricular performance, and an independent predictor of morbidity and mortality from coronary heart disease, is the ventricular or myocardial mass. Myocardial mass can be derived by multiplying the myocardial volume with the myocardial density. The myocardial density is variable, but a value of 1.05 g/cm³ is often used.
Two different approaches are used to obtain the ventricular volumes, function and mass: geometric assumptions and volumetric ventricular quantification.
Geometric assumptions compare the ventricular cavity with a geometrical model. Geometric assumptions are used in planar imaging techniques, such as echocardiography, scintigraphy and contrast ventriculography. They have the advantage of rapidly obtaining ventricular volumes and LV mass, but they are only reliable as long as the geometrical model corresponds to the true ventricular cavity or myocardial wall, which might not be the case in focally diseased ventricles.
Volumetric quantif ication is based on Simpson’s rule. The volume of a complex structure, such as a ventricle, can be quantified by dividing this structure into several smaller, less complex subvolumes. By delineation of the endocardial contours, multiplication of the area by the thickness of the imaging plane and the interslice distance, an addition of these subvolume slices yields the total ventricular volume. Volumetric quantification has the advantage of more reliably quantifying the ventricular volumes and being more easy to reproduce than the geometric assumptions techniques.
LV function
Data acquisition & image reconstruction
Cardiac computed tomography (CT) can be performed using both a retrospective ECG-gating or a prospective triggering technique. When retrospective gating is used, the ECG signal is recorded simultaneously during a spiral CT acquisition. Thus, image reconstruction can be obtained at any desired point throughout the cardiac cycle and the ESV and EDV can be reconstructed to assess ventricular function [6,7]. This acquisition technique is less likely to trigger cardiac arrhythmia. Prospective triggering has historically been used for unenhanced calcium scoring and has recently been proposed for contrast-enhanced coronary imaging owing to the significant dose reduction. This acquisition technique consists of a transverse scan in which x-rays are only turned on during a desired phase of the cardiac cycle. A fundamental requirement for this technique is an accurate prediction of the patient’s cardiac cycle and precise synchronization with the x-rays. This technique makes the patient vulnerable to arrhythmia and heart rate variability, and can be performed only in patients with a stable heart rate below 65 beats per min. Furthermore, to evaluate functional parameters, a double trigger needs to be set at end-diastolic and end-systolic phases, which are usually centered at 0 and 30–50% of the cardiac cycle, respectively. To date, this double acquisition can only be performed on a few scanners. Depending on the scanner used, scan time may differ, but the state of the art for coronary assessment requires a submillimeter spatial resolution along the z-axis, and possibly the isotropic voxel; this allows a real 3D reconstruction of images and enables measurements to be made in any desired plane [8]. The most important technical parameter is the temporal resolution (TR); in fact, imaging of the moving heart requires a high TR to achieve a artifact-free display of myocardial contraction over the cardiac cycle. This is possible using new-generation scanners. With four- and 16-slice MDCT systems, the TR achievable was not optimal (250 and 210 ms, respectively) and multisegment reconstruction algorithms were needed [9,10]. Multisegment reconstruction is achieved using small segments of data acquired during two or more cardiac cycles. Multiple segments of data are combined to make the final image at end systole. The resulting TR equals the gantry rotation time divided by 2N, where N is the number of cycles. However, the z-axis spatial resolution can decrease if there are gaps in the acquired data. The maximum number of cycles typically used is two or three, beyond which image quality falls.
Data analysis
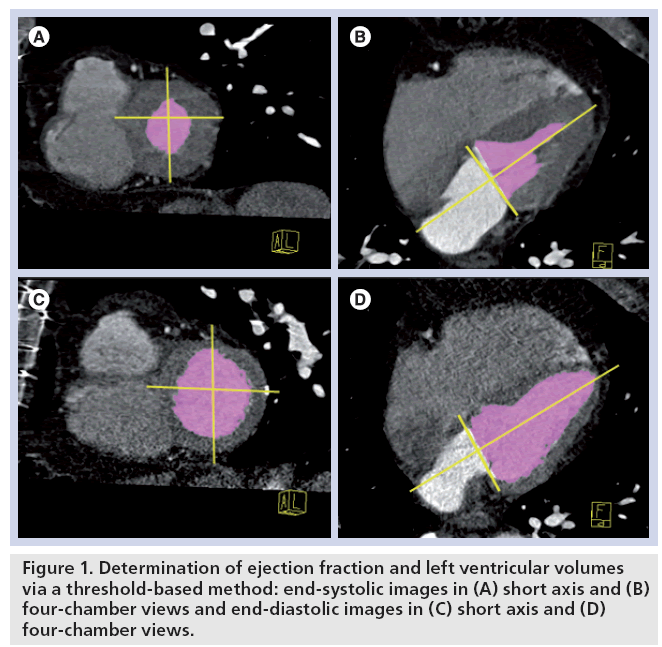
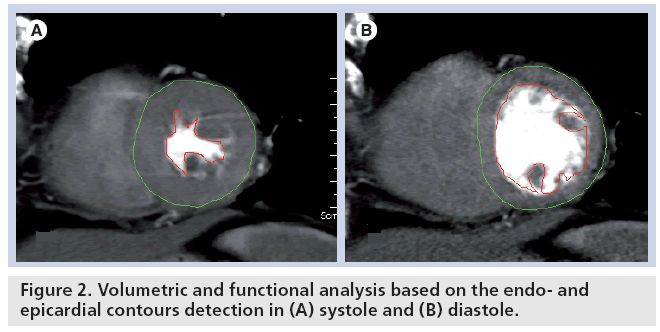
To assess EF, a diastolic phase (usually found at 95–0% of RR interval) and a systolic phase (usually found at 30–50% of RR interval) are necessary, and can be performed by visual analysis of the short-axis images that are reconstructed every 5–10% of the RR interval at a representative mid-ventricular level. LV volumes can then be measured by use of the area–length method (used primarily in echocardiography based on a vertical or horizontal long-axis view), the Simpson method (primarily used in cardiac MRI) or a threshold-based volumetric method (developed in MDCT to take advantage of the high contrastto- noise ratio between the LV cavity and the myocardium) [11]. Generally, the Simpson method and the threshold-based volumetric method are considered more reliable as they do not rely on geometric assumptions for determination of global LV parameters such as LV volumes or EF. The threshold-based method calculates the EDV and ESV on a pixel-by-pixel basis after appropriate definition of the mitral valve plane and left ventricle, excluding the LV outflow tract (Figures 1 & 2). Owing to the complex shape of the heart, the myocardium wall is tilted toward the apex and is not orthogonal to a predetermined study axis; thus, only multiplanar reconstruction images along cardiac axis, long axis, horizontal and vertical axis, and short axis can completely compensate this deviation, providing a precise wallthickness measurement as well as an evaluation of global and regional function. Most of the recently released software automatically generates these cardiac orientations, shortening the evaluation time, whereas in some cases the manual reformation is needed from the primary axial images [12]. If the planes are not perpendicular to the wall or the cavity, subsequent partial volume effects and obliqueness can introduce a large overestimation of the true dimensions. Once long- and short-axis views are generated, end-diastolic and end-systolic phases can be either automatically or manually individuated, depending on the software in use. Finally, diastolic and systolic LV volumes can be calculated using standard CT software with different approaches. To determine measurements for both global and regional functions, only the end-diastolic and end-systolic phases are used [13]. For the volume analysis, only endocardial LV borders need to be drawn. If LV mass is also needed in order to perform regional quantitative analysis, epicardial borders have to be drawn too. To correctly identify the epicardial border, the opacification of right ventricle cavity is mandatory to obtain a different attenuation compared with the septal myocardium. Thus, a dedicated contrast-medium injection protocol must be applied, such as a dual-flow rate approach or the injection of a mixture of contrast and saline (20% contrast and 80% saline) after the contrast bolus. Endocardial and epicardial contours are either automatically detected by the analysis software or have to be manually traced on systolic and diastolic short-axis image reformations. Software packages for CT that semiautomatically perform ventricular volume and wall-thickness measurements are widely available and help to speed up analysis and reporting, as well as improve reproducibility of results. An accurate definition of the basal slice is desired, because it contains the largest area of the CT image reformations stack; a potential error in LV volumetry might be caused from inadequate slice selection. For the volume calculation, papillary muscles should be excluded from the cavity [14].
For regional function assessment of the left ventricle, there is a need for standardization of imaging modalities to assure that accurate intraand cross-modality comparisons can be made for patient management and research (cardiac ultrasound, MRI and CT). Measurements of regional LV function are based on the assessment of systolic thickening by use of the 17-segment model proposed by the American Heart Association [15].
Assessment of LV function using MDCT
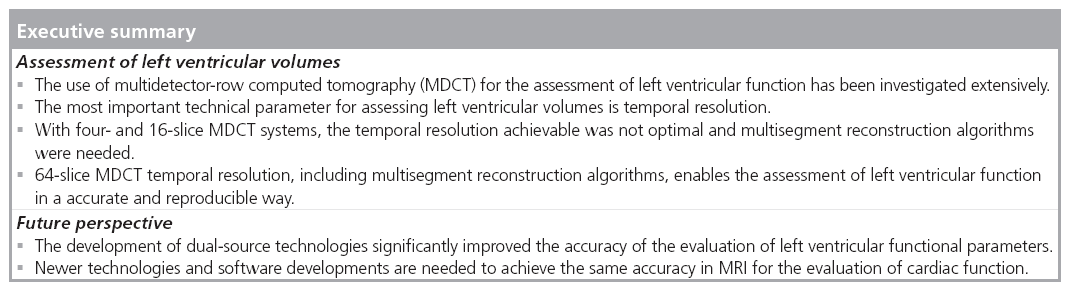
Since the introduction of CT in the early 1970s, it has remained an ongoing challenge to obtain better spatial resolution and TR in order to acquire more detailed images in less time. Early CT scanners could not attain the acquisition times and the spatial resolution required to generate functional images of the heart. However, the introduction of MDCT in the early 1990s lowered acquisition times and spatial resolution to the range where functional imaging of the heart is feasible [16]. The use of MDCT for the assessment of LV functions has been investigated extensively. Studies using older generation CT showed that function assessment could be performed, but the TR of the four-slice (250 ms) and 16-slice (210 ms) MDCT systems hampered the sensitivity for detection and accurate classification of regional LV wall motion abnormalities. Owing to the limited TR, systolic images, especially those obtained in patients with a higher heart rate, were shown to be of lower quality. Additionally, ESV was overestimated, while EDV was not significantly different. As a result, underestimation of EF was noted in several studies (Table 1). More recently, assessments performed on 64-slice MDCT scanners, capable of achieving better TR, demonstrated a significant improvement in the accuracy of MDCT in the evaluation of LV function [17]. Butler et al. concluded that 64-slice MDCT could be an alternative for suboptimal echocardiography results [18], and Salem et al. found that 64-slice MDCT enabled LV function analysis in patients with regular sinus rhythm [19]. Mahnken et al. showed that reliable assessment of LV volumes was also possible at increased heart rates with the introduction of multisegmental image reconstruction algorithms that use data from multiple RR intervals, which allowed the TR of cardiac CT to be improved [20].
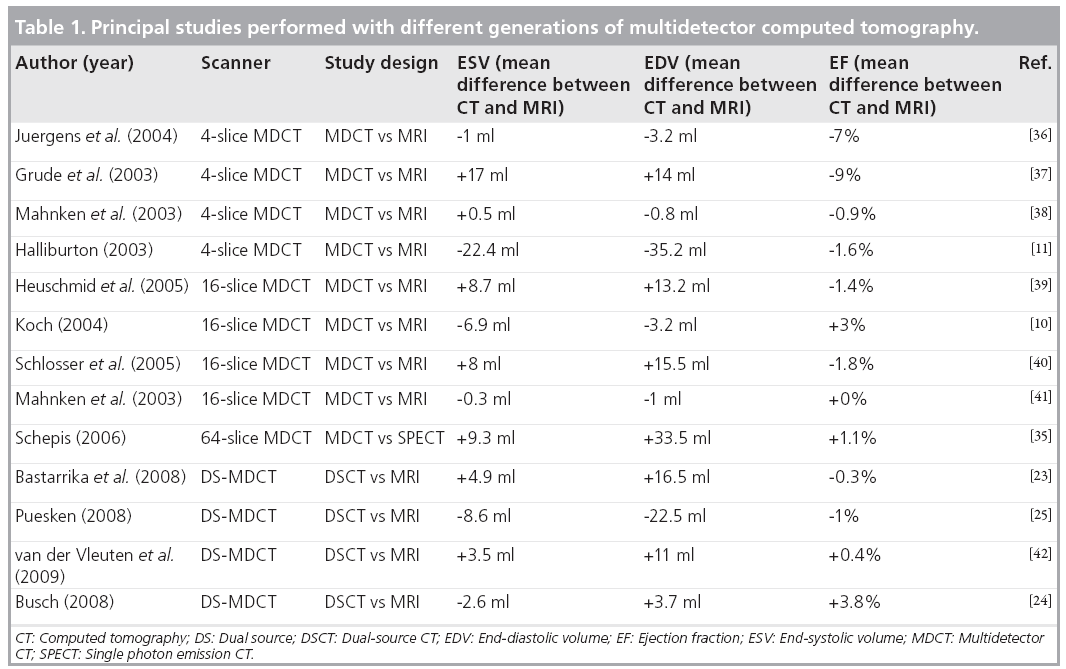
Recently, a new CT system equipped with two tubes and corresponding detectors in a 90° geometry has been designed and provides a heart-rate-independent TR of 83 ms. The latter may be further improved by use of a multisegment reconstruction algorithm and could be as low as 42 ms. There are several data on the diagnostic accuracy of this technique (Table 1). In fact, the study by Mahnken et al. [21], which used a moving heart phantom, demonstrated a good correlation between dual-source CT (DSCT) and MRI, with no significant differences, which is in accordance to the in vivo study by Van der Vleuten et al. [22]. The study by Bastarrika et al. on transplant patients demonstrated the reliability of LV function quantification in individuals with high heart rates [23]. According to Busch et al. [24], the observed nonsignificant differences between functional parameters acquired in DSCT and MRI may be caused by physiological effects due to rapid contrast material injection and the absence of b-blocker medication in CT. In further studies, β-blockers were used to lower the heart rate, which has been postulated to be responsible for reduced EF values in CT examinations. Second, the trend of higher injection rates in CT may cause a stronger inotropic and chronotropic effect and may explain higher values for EF and SV in CT studies compared with values acquired in MRI. An explanation for these differences is the visualization of endocardial borders and the exclusion or inclusion of trabeculae into the LV blood pool. This may explain why there is an underestimation of the systolic volume, while there is an overestimation in diastole, because trabeculae can cause an actual underestimation of EDVs in MRI as they reduce the diameter of the endocardial contour, while the region-growing algorithm counts bright pixels between the trabeculae as blood pool in CT. In systole, the effect should be smaller because the trabeculae lie closely adjacent to each other so that there is only a very small volume between trabeculae. Of course, the depiction of the trabeculae will depend on a high contrast opacification of the ventricular blood pool. Puesken et al. suggested that the systematic underestimation of LV volumes by the 3D-segmentation algorithm is explained by a different handling of the papillary muscles: soft-tissue density structures such as the papillary muscles are excluded from the LV volume by attenuation-based segmentation, whereas standard short-axis-based LV function analysis from CT and MRI data sets usually accounts for them as part of the LV cavity [25]. However, Sievers et al. demonstrated that systematic subtraction of papillary muscles and trabeculations from LV volume has no significant impact on the reliability of LV EF evaluation [26]. A recent study by Groen et al. [27], which compares MRI, 64-slice MDCT and DSCT in assessing functional cardiac parameters of a moving heart phantom, demonstrated that a clinically implemented MRI protocol structurally underestimates functional parameters, EF and cardiac output of a moving heart phantom. A clinical implemented protocol using a 64-slice MDCT underestimates or overestimates these functional parameters depending on the heart rate, and a clinical protocol using DSCT deviates the least from these functional parameters compared with MRI and 64-slice MDCT. De Cecco et al. [28] demonstrated in vivo an accurate evaluation of functional parameters by DSCT, which was in agreement with data obtained from MRI. However, in this study, the authors underline a tendency to underestimate the EF even if the difference was not statistically significant.
Although the TR can be improved with multisegment reconstruction, leading to better reproducibility in a phantom study [21], it was shown that this technique did not improve results for studies in human subjects. In fact, in a study by Juergens et al. [29], the multisegment image reconstruction achieved a significant increase of TR at the expense of spatial resolution causing a deterioration of the slice profile and consecutive blurring of endocardial borders. Thus, it can be assumed that improved TR without a reduction in spatial volume may allow for a more reliable assessment of global ventricular function.
Conclusion
Since MRI was the first noninvasive technique to provide high-resolution 3D functional images of the heart, it is regarded by many as the current standard of reference for LV function. The main advantage of MRI is its excellent TR without exposing the patient to ionizing radiation. Furthermore, it does not rely on geometrical assumptions for LV function parameters. However, MRI cannot be performed in patients with a pacemaker or cerebral vascular clips for both safety and image-distortion reasons; furthermore, it is expensive and not always available [30]. As an alternative to MRI, MDCT can be used to assess functional parameters of the left ventricle [31]. However, DSCT has a TR more similar to the TR of MRI, and also has a relatively high spatial resolution [32]. A significant reduction in postprocessing time is achieved owing to advanced raw-data reconstruction algorithms, automatic generation of cardiac axis views, automatic determination of end-diastolic and end-systolic phases, and automatic LV myocardial segmentation for regional function assessment. New software for automatic anatomic tube current modulation is being developed and appears to significantly reduce radiation exposure [33].
In conclusion, over the years, CT has evolved to a point where contemporary multidetector-row systems combined with adequate reconstruction algorithms and postprocessing tools can perform global LV functional assessment. However, for 64-slice MDCT systems with further improved TR, head-to-head comparisons with MRI in vivo are not yet available, even if promising results have been published in some studies [26,34,35]. DSCT allows a quick, accurate and global evaluation of the heart, both for functional parameters and coronary artery disease, as demonstrated in several studies. The limitation of this system and MDCT is the tendency to overestimate LV volumes when compared with MRI. There are different explanations, but since the differences are not statistically significant, we can conclude that functional parameters obtained using MDCT are readily interchangeable with those obtained with MRI.
Future perspective
The application of conventional CT to cardiac imaging has long been limited by insufficient TR owing to slow gantry rotation and long total acquisition time, resulting from slow volume coverage with single-slice imaging. With the development of multidetector technology, cardiac CT is increasingly being used in the diagnosis of coronary artery disease and for cardiac morphology assessment. Furthermore, 64-slice MDCT scanners, capable of achieving better TR, demonstrated a significant improvement in the accuracy of evaluating LV function and is capable of achieving this at faster heart rates with the introduction of multisegmental image-reconstruction algorithms.
The improvement in TR achieved with the dual-source technology increased the accuracy of the evaluation of LV volumes. Newer scanners with even higher TR, owing to faster rotation time and the development of software solutions adapted from MRI or echocardiography, will overcome the current limitations regarding standardized LV function analysis.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
• of interest
- White HD, Norris RM, Brown MA, Brandt PW: Left ventricular endsystolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation 76, 44–51 (1987).
- Yamamuro M, Tadamura E, Kubo S: Cardiac functional analysis with multi-detector row CT and segmental reconstruction algorithm: comparison with echocardiography, SPECT, and MR imaging. Radiology 234, 381–390 (2005).
- Malm S, Frigstad S, Sagberg E, Larsson H, Skjaerpe T: Accurate and reproducible measurement of left ventricular volume and ejection fraction by contrast echocardiography: a comparison with magnetic resonance imaging. J. Am. Coll. Cardiol. 1(44), 1030–1035 (2004).
- Higgins CB, Sakuma H: Heart disease: functional evaluation with MR imaging. Radiology 199, 307–315 (1996).
- Mollet NR, Cademartiri F, Nieman K et al.: Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J. Am. Coll. Cardiol. 43, 2265–2270 (2004).
- Savino G, Zwerner P, Herzog et al.: CT of cardiac function. J. Thorac. Imaging 22(1), 86–100 (2007).
- Nieman K, Cademartiri F, Lemos PA et al.: Reliable non invasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106, 2051–2054 (2002).
- Juergens KU, Grude M, Fallenberg EM: Using ECG-gated multidetector CT to evaluate global left ventricular myocardial function in patients with coronary artery disease. Am. J. Roentgenol. 179, 1545–1550 (2002).
- Boehm TAH, Roffi M, Willmann JK: Time–effectiveness, observer-dependence, and accuracy of measurements of left ventricular ejection fraction using 4-channel MDCT. Rofo 176, 529–537 (2004).
- Koch KE, Oellig F, Kunz P: Assessment of global and regional left ventricular function with a 16-slice spiral-CT using two different software tools for quantitative functional analysis and qualitative evaluation of wall motion changes in comparison with magnetic resonance imaging. Rofo 176, 1786–1793 (2004).
- Halliburton SS, Petersilka M, Schvartzman PR: Evaluation of left ventricular dysfunction using multiphasic reconstructions of coronary multi-slice computed tomography data in patients with chronic ischemic heart disease: validation against cine magnetic resonance imaging. Int. J. Cardiovasc. Imaging 19(1), 73–83 (2003).
- Orakzai S, Orakzai R, Nasir K: Assessment of cardiac function using multidetector row computed tomography. J. Comput. Assist. Tomogr. 30, 555–563 (2006).
- Fischbach R, Juergens K, Ozgun M et al.: Assessment of regional left ventricular function with multidetector-row computed tomography versus magnetic resonance imaging. Eur. Radiol. 17, 1009–1017 (2007).
- Juergens KU, Fischbach R: Left ventricular function studied with MDCT. Eur. Radiol. 16, 342–357 (2006).
- Cerqueira MD, Weissman NJ, Dilsizian V et al.: American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4), 539–542 (2002).
- Boese JM, Bahner NL, Albers J, van Kaick G: Optimizing temporal resolution in CT with retrospective ECG gating. Radiology 40, 123–129 (2000).
- Halliburton SS, Boese JM, Flohr TG: Improved volumetric analysis of the left ventricle using cardiac multi-slice computed tomography (MSCT) with high temporal resolution image reconstruction. Radiology 252(P), 389 (2002).
- Butler J, Shapiro MD, Jassal DS et al.: Comparison of multidetector computed tomography and two-dimensional transthoracic echocardiography for left ventricular assessment in patients with heart failure. Am. J. Cardiol. 99(2), 247–249 (2007).
- Salem R, Remy-Jardin M, Delhaye D et al.: Integrated cardiothoracic imaging with ECG-gated 64-slice multidetectorrow CT: initial findings in 133 patients. Eur. Radiol. 17(4), 902–910 (2007).
- Mahnken AH, Hohl C, Suess C: Influence of heart rate and temporal resolution on left-ventricular volumes in cardiac multislice spiral computed tomography: a phantom study. Invest. Radiol. 41, 429–435 (2006).
- Mahnken AH, Bruder H, Suess C: Dual-source computed tomography for assessing cardiac function: a phantom study. Invest. Radiol. 42, 491–498 (2007).
- Van der Vleuten PA, Willems TP, Götte MJW et al.: Quantification of global left ventricular function: comparison of multidetector computed tomography and magnetic resonance imaging. A meta-analysis and review of the current literature. Acta Radiol. 47(10), 1049–1057 (2006).
- Bastarrika G, Arraiza M, De Cecco CN et al.: Quantification of left ventricular function and mass in heart transplant recipients using dual-source CT and MRI: initial clinical experience. Eur. Radiol. 18(9), 1784–1790 (2008).
- Busch S, Johnson TR, Wintersperger BJ: Quantitative assessment of left ventricular function with dualsource CT in comparison to cardiac magnetic resonance imaging: initial findings. Eur. Radiol. 18, 570–575 (2008).
- Puesken M, Fischbach R, Wenker M: Global left-ventricular function assessment using dual-source multidetector CT: effect of improved temporal resolution on ventricular volume measurement. Eur. Radiol. 18, 2087–2094 (2008).
- Sievers B, Kirchberg S, Bakan A et al.: Impact of papillary muscles in ventricular volume and ejection fraction assessment by cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 6(1), 9–16 (2004).
- Groen JM, Van der Vleuten PA, Greuter MJW: Comparison of MRI, 64-slice MDCT and DSCT in assessing functional cardiac parameters of a moving heart phantom. Eur. Radiol. 19(3), 577–583 (2009).
- De Cecco CN, Bastarrika G, Pueyo J et al.: Global cardiac evaluation without heart rate control: preliminary experience with dual source CT (DSCT). Minerva Cardioangiol. 56(6), 587–597 (2008).
- Juergens KU, Maintz D, Grude M, Boese JM: Multi-detector row computed tomography of the heart: does a multisegment reconstruction algorithm improve left ventricular volume measurements? Eur. Radiol. 15, 111–117 (2005).
- Steen H, Nasir K, Flynn E: Is magnetic resonance imaging the ‘reference standard’ for cardiac functional assessment? Factors influencing measurement of left ventricular mass and volumes. Clin. Res. Cardiol. 96, 743–751 (2007).
- Leschka S, Alkadhi H, Plass A: Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur. Heart J. 26, 1482–1487 (2005).
- Brodoefel H, Kramer U, Reimann A et al.: Dual-source CT with improved temporal resolution in assessment of left ventricular function: a pilot study. AJR Am. J. Roentgenol. 189, 1064–1070 (2007).
- Juergens KU, Seifarth H, Maintz D: MDCT determination of volume and function of the left ventricle: are short-axis image reformations necessary? AJR Am. J. Roentgenol. 186(6 Suppl. 2), S371–S378 (2006).
- Henneman MM, Schuijf JD, Jukema JW: Assessment of global and regional left ventricular function and volumes with 64-slice MSCT: a comparison with 2D echocardiography. J. Nucl. Cardiol. 13, 480–487 (2006).
- Schepis T, Gaemperli O, Koepfli P: Comparison of 64-slice CT with gated SPECT for evaluation of left ventricular function. J. Nucl. Med. 47, 1288–1294 (2006).
- Juergens KU, Grude M, Maintz et al.: Multi-detector row CT of left ventricular function with dedicated analysis software versus MR imaging: initial experience. Radiology 230(2), 403–410 (2004).
- Grude M, Juergens KU, Wichter T et al.: Evaluation of global left ventricular myocardial function with electrocardiogramgated multidetector computed tomography: comparison with magnetic resonance imaging. Invest. Radiol. 38(10), 653–661 (2003).
- Mahnken AH, Spüntrup E, Wildberger JE et al.: Quantification of cardiac function with multislice spiral CT using retrospective EKG-gating: comparison with MRI. Rofo 175(1), 83–88 (2003).
- Heuschmid M, Rothfuss J, Schröder S et al.: Left ventricular functional parameters: comparison of 16-slice spiral CT with MRI. Rofo 177(1), 60–66 (2005).
- Schlosser T, Pagonidis K, Herborn CU et al.: Assessment of left ventricular parameters using 16-MDCT and new software for endocardial and epicardial border delineation. AJR Am. J. Roentgenol. 184(3), 765–773 (2005).
- Mahnken AH, Spuentrup E, Niethammer M et al.: Quantitative and qualitative assessment of left ventricular volume with ECG-gated multislice spiral CT: value of different image reconstruction algorithms in comparison to MRI. Acta Radiol. 44(6), 604–611 (2003).
- van der Vleuten PA, de Jonge GJ, Lubbers DD et al.: Evaluation of global left ventricular function assessment by dualsource computed tomography compared with MRI. Eur. Radiol. 19(2), 271–277 (2009).
• Investigates the influence of heart rate and temporal resolution on the assessment of left ventricular function with 64-multislice spiral computed tomography. It demonstrates that reliable assessment of left ventricular volumes was also possible at increased heart rates with the introduction of multisegmental image reconstruction.
• Demonstrates that the markedly improved temporal resolution with dual-source computed tomography (DSCT) allowed ventricular function to be reliably assessed, even in patients with increased heart rates or under stress conditions.
• Data presented in this review indicate that the global left ventricular functional parameters measured by contemporary multidetector row systems combined with adequate reconstruction algorithms and postprocessing tools show a narrow diagnostic window and are interchangeable with those obtained by MRI.
• Demonstrates the reliability of left ventricular function quantification in individuals with high heart rates using DSCT compared with MRI.
• Compares, for the first time, MRI, 64-slice multidetector-row computed tomography and DSCT, and showed there are few differences between them.
• Recent in vivo study demonstrating that global left ventricular functional parameters, calculated from DSCT data sets have acceptable limits of agreement with global left ventricular parameters obtained using MRI.