Case Report - Imaging in Medicine (2017) Volume 9, Issue 1
Embolization of left gastric artery pseudoaneurysm after blunt trauma
Lavi Nissim*, Conrad Diven & Aaron Braun
Abrazo West Campus, Arizona, USA
- *Corresponding Author:
- Lavi Nissim
Abrazo West Campus, Arizona, USA
E-mail: lavinissim@gmail.com
cfdiven1@abrazohealth.com
Abstract
Traumatic pseudoaneurysms of the visceral arteries are a rare but described entity. Typically, these are associated with penetrating trauma to the torso. They may present as a diagnostic challenge, as detection on conventional CT angiography is limited in the absence of surrounding hematoma or evidence for soft tissue or visceral organ injury. Clinically, this form of injury may present in both acute and delayed fashions. Post-traumatic pseudoaneurym of the left gastric artery is a seldom-described entity, particularly when encountered after blunt trauma. Here we present a young patient who sustained extensive injury after motor vehicle accident, with hemorrhagic shock on ER admission. Pseudoaneurysm with active bleeding from the left gastric artery was promptly detected on CT and immediately treated by angiographic embolization. A discussion of the available literature follows the case report.
Keywords
left gastric artery, pseudoaneurysm, blunt trauma, embolization
Case Report
An otherwise healthy 25 years old male presented as a restrained driver in a head-on motor vehicle collision. Upon arrival to the ER, he reported 10/10 abdominal and chest pain. His initial Glasgow Coma Scale score was 15. He was noted to be tachycardic in the 110 s-120 s with a mean arterial blood pressure of 67. On physical examination, he had a positive “seatbelt sign” and epigastric tenderness.
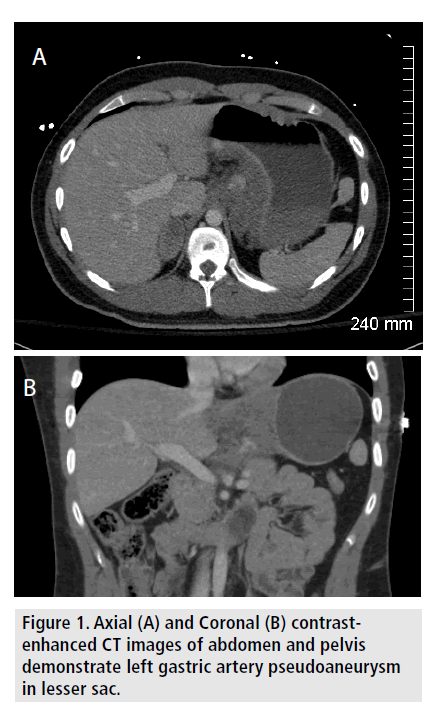
Initial radiographic imaging demonstrated extremity fractures, with no free intra-peritoneal air. A CT scan of the torso was performed, showing a large hematoma measuring 4.8*2.9*5.8 cm in the lesser sac of the abdomen, with an active blush arising from the left gastric artery (FIGURE 1). There was no evident injury to the stomach, duodenum, or pancreas. Within 2 hr of initial presentation, the patient was noted to be in hemorrhagic shock, with estimated mean arterial pressure dropping from 98 to 46 and Interventional Radiology was consulted for emergent angiogram with embolization; his hematocrit was 38.6 at this time. The procedure was started approximately 45 min after the CT examination.
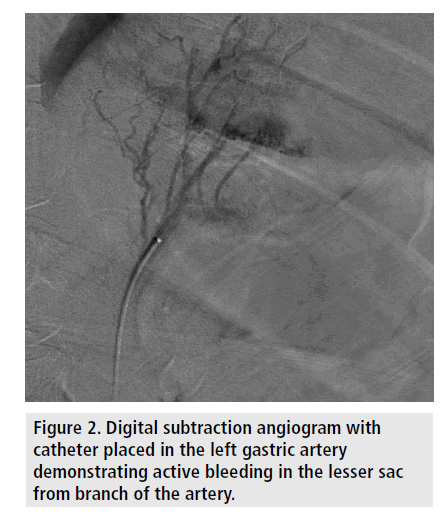
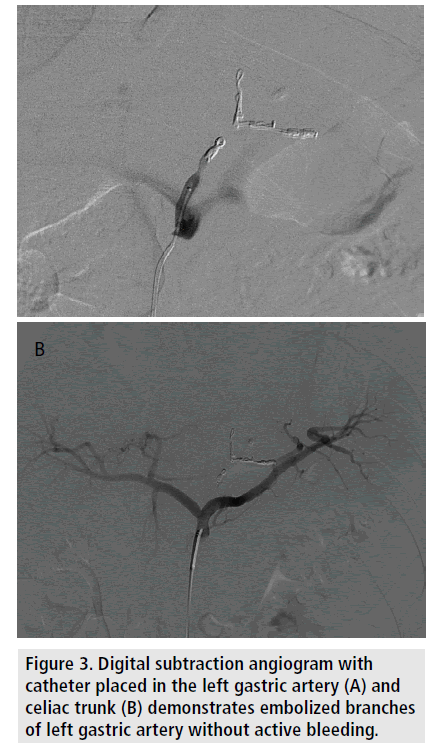
Access was achieved in the right common femoral artery using standard Seldinger technique. Using a Cobra 2 catheter (Angiodynamics, Latham, NY) placed in the celiac artery, digital subtraction angiogram was performed; this identified blush of extravasated contrast in the epigastric region. Utilizing a 0.027” Renegade Hi-Flo catheter (Boston Scientific, Marlborough, MA), the left gastric artery was selected and angiogram performed, confirming the presence of a pseudoaneurysm with active extravasation arising from a prominent branch vessel (FIGURE 2). The branch vessel was then selected and embolized using a detachable 2 mm*40 mm Ruby coil (Penumbra Inc, Alameda, CA) and a detachable 3 mm*150 mm Ruby coil. The proximal left gastric artery was then embolized using a 3*50 mm Ruby coil and a 3 mm*3.3 mm VortX Diamond 18 coil (Boston Scientific) to stasis (FIGURE 3). The procedure was performed within 1 hour utilizing 125 ml of iodinated contrast and 17 min of fluoroscopy for a radiation dose length product of 18335 mGy.
The patient was administered intravenous analgesia with 50 μg Fentanyl for the procedure.
Figure 2. Digital subtraction angiogram with catheter placed in the left gastric artery demonstrating active bleeding in the lesser sac from branch of the artery.
Figure 3. Digital subtraction angiogram with catheter placed in the left gastric artery (A) and celiac trunk (B) demonstrates embolized branches of left gastric artery without active bleeding.
The patient was hemodynamically stable immediately following the procedure, and his pain was well-controlled. On post-procedural day 1, the patient was noted to have a mean arterial pressure of approximately 87. On post-procedural day 3, he was noted to have a gradual decrease in hematocrit to 19.2; this was corrected with 1 unit of packed red blood cells to 22.8. He reported significant improvement in pain control and was discharged 6 days after his initial imaging. A follow-up CT examination performed prior to discharge showed stable hematoma posterior to the stomach with no further active bleeding. The patient was evaluated in the office one month after his trauma and there was no evidence for recurrent bleeding.
Discussion
True aneurysms of the visceral arteries are rare anomalies that are often asymptomatic and found incidentally after spontaneous rupture. Risk factors for true visceral artery aneurysm rupture include size, pregnancy and hypertension. Typically, these involve the splenic or renal arteries, with solitary gastric artery aneurysms quite rare. Even more uncommon are the incidence of false aneurysms, also known as pseudoaneurysms, of the visceral arteries; these can present in the settings of chronic intra-abdominal inflammation such as from pancreatitis, after prior intra-abdominal surgery, or after trauma. Often times visceral pseudoaneurysms may be a diagnostic challenge and they may not be detected for days or even months after the incendiary event [1-3].
In the case of visceral artery pseudoaneurysm secondary to trauma, the etiology is more frequently penetrating rather than blunt trauma [4]. This may be due to the protective nature of the overlying visceral organs during blunt injury to the abdomen. Nevertheless, this entity should be suspected in the setting of expanding intra-abdominal hematoma, even with no active bleeding detected on routine imaging studies. In the few cases reported in the literature, delay in detection appears to be prevalent, from days to even months after the injury [1,5]. In a case series of 9 visceral pseudoaneurysms due to penetrating trauma, the mean presentation was 12.3 weeks after injury; these were detected only after erosion in to visceral organs of the GI tract, respiratory tract, or urinary tract [3].
Treatment recommendations for posttraumatic pseudoaneurysms of the visceral arteries vary in the literature and should be individualized depending on the clinical scenario. Since they are not always detected on CT or be associated with other injuries, they are sometimes initially diagnosed and henceforth treated at the same time as exploratory laparotomy, with vessel over-sew or primary repair [1,6]. Minimally invasive angiogram with coil embolization of the feeding vessel or aneurysm sac itself can be attempted, though not always successful [2,4,6]. Stent-graft placement to preserve patency of native vessel has also been described [1].
Given its proximity to the pancreas, rupture of left gastric artery pseudoaneurysm should be suspected clinically when there is expanding hematoma in the lesser sac or in the setting of pancreatic inflammation or injury [5,7]. This entity is rarely reported after blunt trauma to the abdomen [5,8,9]. In addition to lesser sac hematoma with associated symptom of epigastric pain, rupture into the mediastinum or chest cavity is plausible, and should be considered [10]. This case report illustrates the use of contrastenhanced arterial-phase computed tomography in rapid detection of the entity in a patient with hemorrhagic shock after motor vehicle blunt trauma. The ability to diagnose with CT and treat with endovascular approach resulted in expedient stabilization of the patient without the need for exploratory laparotomy of the lesser sac and associated complications. In a patient with blunt trauma to the epigastric region, consideration should be made to diagnostic angiography in the setting of expanding lesser sac hematoma for early detection and treatment of occult injury to the left gastric artery.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Ceppa EP, Evans DC, Upton EC et al. Endovascular treatment of a traumatic visceral aneurysm. J. Trauma. 65, 929-932 (2008).
- Adam S, Bruce JL, Laing GL et al. Successful selective angiographic embolisation of a gastroduodenal pseudoaneurysm following penetrating abdominal trauma. S. Afr. J. Surg. 52, 79-81 (2014).
- Hassantash SA, Mock C, Maier RV. Traumatic visceral artery aneurysm: Presentation as massive hemorrhage from perforation into an adjacent hollow viscus. J. Trauma. 38, 357-360. (1995)
- Olsen AB, Ralhan T, Harris JH Jr. et al. Superior mesenteric artery pseudoaneurysm after blunt abdominal trauma. Ann. Vasc. Surg. 27, 674-678. (2013)
- Mathew AJ, Raju RS, Vyas FL et al. Left gastric artery pseudoaneurysm following traumatic pancreatic transection. Trop. Gastroenterol. 28, 133-134 (2007).
- Park CY, Ju JK, Kim JC. Damage control surgery in patient with delayed rupture of pseudoaneurysm after blunt abdominal trauma. J. Korean. Surg. Soc. 83, 119-122 (2012).
- Smith RE, Fontanez-Garcia D, Plavsic BM. Gastrointestinal case of the day. Pseudoaneurysm of the left gastric artery as a complication of acute pancreatitis. Radiographics. 19, 1390-1392 (1999).
- Varela JE, Salzman SL, Owens C et al. Angiographic embolization of a left gastric artery pseudoaneurysm after blunt abdominal trauma. J. Trauma. 60, 1350-1352 (2006).
- Allorto NL, Royston D, Hadley GP. Traumatic false aneurysm of the left gastric artery. Pediatr. Surg. Int. 25, 455-457. (2009)
- Lee MK, Vrazas JI. Ruptured left gastric artery aneurysm: unique presentation with hemothorax and hemomediastinum. Cardiovasc. Intervent. Radiol. 29, 438-442 (2006).