Research Paper - Imaging in Medicine (2017) Volume 9, Issue 4
Evaluating patients with pulmonary thromboembolism: a retrospective study on the utilization of serum D-dimer assay and CT angiography
Amar Richard Tobias*, Anjali Agrawal & Arjun KalyanpurTeleradiology Solutions Private Limited Bangalore, India
- Corresponding Author:
- Amar Richard Tobias
Teleradiology Solutions Private Limited Bangalore, India
E-mail: drtobias.ra@gmail.com
Abstract
Background and objective: Serum D-dimer assay is an inexpensive laboratory test with a high negative predictive value, obviating the need for computed tomographic pulmonary angiography (CTPA) in patients with low clinical probability of thromboembolic disease. It has been recommended that CTPA may be performed only in patients with positive D-dimer assays and clinical suspicion of PTE (pulmonary thromboembolism), to curb unnecessary imaging and health care costs. We wanted to reassess the validity of this recommendation by looking into the D-dimer results in patients with positive PTE on CTPA.
Methods: All patient records with positive PTE diagnosis on CTPA and having relevant laboratory data during one calendar year (January 01 to December 31, 2009) were selected. Serum D-dimer values of >500 ng/ml was considered abnormal. The D-dimer results among the patients who had the test performed were tabulated based on age and sex along with those without D-dimer assay in the same groups and correlated with their percentage distribution.
Results: Out of a total of 98 positive PTE cases on CTPA, only 26 patients (26.5%) had a serum D-dimer assay done prior to CTPA. Of these, 20 (76.9%) had elevated values and 6 cases (23.1%) had a negative test. Negative D-dimer results varied with patient age, being highest in the 21-40 years age group.
Conclusion: Overall, there seems to be more preferred use of CTPA and underutilization of serum D-dimer assay in clinical practice for suspected PTE. Secondly, negative D-dimer assay should not be used to triage patients with a high clinical index of suspicion for PTE.
Keywords
Pulmonary thromboembolism (PTE) • D-dimer assay • computed tomographic pulmonary angiography (CTPA)
Introduction
Pulmonary thromboembolism (PTE) is an obstruction by a thromboembolus in any part of the pulmonary arterial circulation usually manifesting clinically as dyspnea, chest pain or collapse. PTE is the third most common acute cardiovascular disease after cardiac ischemic syndromes and stroke [1]. Deep vein thrombosis (DVT) and PTE are both part of a spectrum of one clinical entity, having an annual incidence of 1.0 and 0.5 per 1000 in the Western world, respectively [2]. Based on autopsy data, the incidence of PTE is even greater [3].
The various tests used to evaluate for PTE include D-dimer assay, computed tomographic pulmonary angiography (CTPA), lower limb ultrasonography, conventional angiography, magnetic resonance angiography (MRA) and ventilation-perfusion scintigraphy. In the recent years CTPA has become the standard of care at many institutions across the world for the initial evaluation of patients with suspected pulmonary thromboembolism [4]. CTPA has demonstrated sensitivities of 53%-100% and specificities of 83%-100%. Such wide ranges of accuracies may in part be due to the wide variety of CT scanners in clinical use [4,5].
D-dimer is an inexpensive, and easily performed laboratory test which a direct biomarker of fibrinolysis and an indirect marker of coagulation. Though increased levels of D-dimer occur in various conditions where the coagulation system is activated; its usefulness lies in its ability to safely exclude the presence of venous thromboembolism due to its high negative predictive value. A sensitivity of 96% and specificity of 52% was reported by Kelly et al. [6]. The enzyme linked immunosorbent assay (ELISA) D-dimer method is considered to be the ‘gold standard’ and most widely used. According to a recent study, the use of a screening D-dimer measurement of 1.0 μg/ml or less precludes CTPA in patients with suspected acute PTE [7].
There have been recommendations to triage patients suspected of PTE using D-dimer assay and that only those with positive D-dimer assays in the right clinical setting ought to have CTPA [8]. Given the current health care environment with emphasis on evidence based medical practice (EBMP), we considered re-assessing the validity of the recommendations of relying solely on D-dimer assay, and denying patients the benefit of CTPA. This would be critical before it becomes an accepted standard for EBMP.
In this study we correlated the results of D-dimer in patients who were diagnosed with PTE based on CTPA and attempted to establish the role of D-dimer assays in diagnostic algorithm for the work-up of suspected PTE.
Materials and Methods
This retrospective, multi-institutional study was approved by our institutional review board and conducted over a calendar year (January 01 to December 31, 2009). All patient reports with a diagnosis of PTE (on CTPA) along with their laboratory data on D-dimer assay during this period were retrieved from our radiology information system (RIS) data base. Few of the studies which did not have relevant laboratory information (confirmation whether serum D-dimer assay was performed or its results) were not included.
The CTPAs were performed on MDCT scanners, all following the minimum recommended ACR protocol for CTPA imaging of PTE [9]. The ACR protocol included slice thickness ≤ 3 mm, slice spacing ≤ slice thickness, to include the entire thorax, using an appropriate scan delay from initiation of intravenous contrast injection. The contrast delivered varied from 80 to 150 ml of at least 300 mg% lowosmolar or iso-osmolar iodinated contrast agent injected at the rate of 3 to 5 cc/s. The images were reconstructed using soft tissue algorithm with a field of view (FOV) that included the entire thorax at the greatest width; images were viewed for detection of thromboemboli, using unlimited gray scale. Lung windows were also available for evaluation of accompanied airway and parenchymal disease, or to detect unsuspected pneumothorax.
A total of 98 cases which were positive for thromboembolism on CTPA were included in this study. The images were interpreted on a picture archiving and communications system
(PACS) (eRAD–eRAD Inc. Corporate Headquarters: South Carolina 29607) workstation by at least two American Board certified radiologists experienced in emergency radiology. The radiology reports of our study group generally included details of the pulmonary thromboemboli such as location(s), partial or total vessel obstruction, associated parenchymal changes and other incidental findings (these details are however not included in this article since the reports with positive PTE was only used to define the study group and further to analyze the D-Dimer usage in that group).
We then retrospectively reviewed laboratory data among these patients with positive CTPA to see if serum D-dimer was performed on them and if so their results. We considered values of >500 ng/ml by ELISA method as abnormal/ raised levels [6]. The data with number of patients who had D-dimer assay performed (segregated into positive and negative results) and those who did not have the test in various age groups were tabulated and analyzed for their percentage distributions.
Results
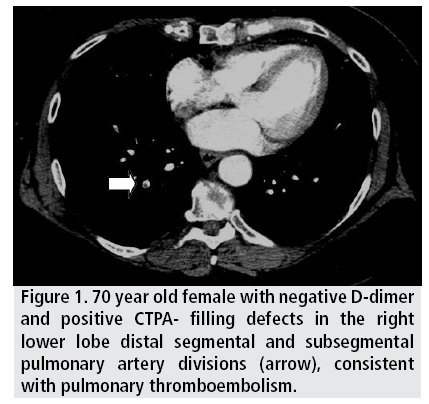
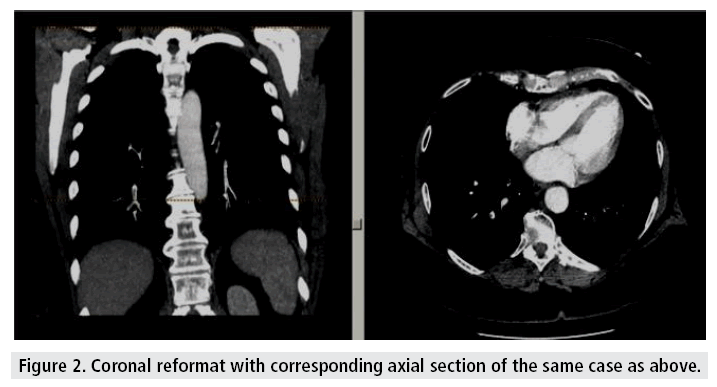
The results are summarized in TABLES 1 and 2. The 98 positive PE cases in this study comprised of 46 (46.9%) men and 52 (53.1%) women. The age of patients in this study group ranged from 17 years to 98 years (mean age of 58.5 years) with a significant number of patients (44.9%) over 60 years of age. A majority of the patients in our study group (73.4%) went directly for CTPA without D dimer assay. Of the 26 patients who were offered a D dimer assay, 20 (76.9%) had elevated values (ranging from 700 to 10540 ng/ml). In patients with high clinical suspicion for PTE (n=90), CTPA was performed without a D-dimer assay; some (n=72) in fact never had a D- dimer assay. In 6 cases (23.1%) though the D-dimer test was negative, CTPA was positive for PTE. The D-dimer positivity varied according to patient age. In the 21 to 40 years age group, 3 patients of 5 (60%) had false negative d dimer results; in the >60 years it was 2 of 12 (16.7%); and in the 41 to 60 years age group 1 of 8 (12.5%). There were no false negatives in the <20 years age group. One of the patients with negative d Dimer results and a positive CTPA is illustrated as example (FIGURES 1 and 2).
| AGE (YEARS)⇨ SEX⇩ | <20 | 21-40 | 41-60 | >60 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| D-dimer done | No D-dimer | D-dimer done | No D-dimer | D-dimer done | No D-dimer | D-dimer done | No D-dimer | |||||
| + | - | + | - | + | - | + | - | |||||
| MALES | 1 | 2 | 1 | 2 | 4 | 1 | 18 | 4 | 1 | 12 | ||
| FEMALES | 1 | 2 | 8 | 3 | 11 | 6 | 1 | 20 | ||||
| TOTAL | 2 | 15 | 37 | 44 | ||||||||
+: Positive D-dimer result
-: Negative D-dimer result
Table 1: Summary of findings.
| D-dimer performed | 26 (26.5%) | POSITIVE RESULTS: 20 (76.9%) |
| NEGATIVE RESULTS: 6 (23.1%) | ||
| D-dimer not performed | 72 (73.4%) | |
| Total | 98 | |
Table 2: D-dimer usage.
Discussion
CTPA has become established as the primary noninvasive imaging test in clinical practice due to its wide availability, safety, cost-effectiveness and high negative predictive value for the diagnosis of clinically relevant PTE [10]. Our study substantiates this, with almost three fourths of the patients (73%) in the study group having CTPA as the initial or the only diagnostic test for suspected PTE. Besides the direct visualization of intraluminal thrombus, the depiction of cardiac and pulmonary function along with the extent of pulmonary arterial obstruction helps to grade the severity of PTE for further risk stratification and subsequent follow-up to assess the success of thrombolytic therapy because PTE and deep venous thrombosis are two different aspects of the same disease, there is an added advantage of CTPA. CT venography can be performed in conjunction with CTPA, utilizing the same contract injection. Several studies have reported that a quantitative D-dimer assay was effective in obviating the need for CTPA, and that it had high negative predictive value of about 99.6% [6,8,11]. In spite of this proven fact however, D-dimer screening is not used according to established diagnostic algorithms to determine the need for MDCT in diagnosing acute pulmonary thromboembolism in the emergent setting [12].
Limitations
Our study design has a few limitations. A major limitation is a selection bias for the study’s subjects as the clinical index of suspicion was not looked for patients who went directly for CTPA versus D-dimer assay. The cases selected were from different institutions. Thus differences in the CT equipment, the scan protocols (though all confirmed to the minimum ACR-2005 recommendations), and viewing algorithms could potentially create some degree of variability of image quality. However, these differences are to be expected in a multi- institutional study which has the advantage of analyzing the clinical practices and protocols from multiple institutions. A prospective study with matching protocol among all the institutions included in the study would be useful to overcome the limitations mentioned. And a larger study group with more robust statistical analysis of the data would help in forming a better consensus/ recommendation.
Our study somewhat points to a relative preference of CTPA over serum D-dimer assay. Furthermore, it is important to note that in our study we found a 23.1% false negative rate for Ddimer assay. Had the CTPAs not been obtained in these patients, appropriate and much needed care would have been denied. This false negative D-dimer results were highest in the 21 to 40 years age group (60%) than in the extremes of age (i.e., <20 and >60 years). Of note, in this age group 2 women underwent D-dimer assay and both were false negative (100%) as shown on subsequent CTPA studies. This may be partly explained by the smaller sample size and differences in laboratory standards; but none the less is an important observation. Thus when clinical suspicion for PTE is high or uncertain, and when other chest pathology is also a clinical possibility, CTPA is a better test than D-dimer as the sole decision making diagnostic tool.
CTPA is now the recommended initial imaging modality for non-massive PTE and patients with a good quality negative CTPA do not require further investigation or treatment for PTE [13].
Nilson et al. in their study also concluded that CTPA has a higher sensitivity and specificity than latex agglutination D-dimer [14]. A recent article by Youssf also states that D-dimer alone cannot exclude or confirm the presence of PE and that a combination of other tests including CTPA is recommended for patients with suspected PE [15].
Conclusion
Our study indicates that there seems to be underutilization of serum D-dimer assay in clinical practice for suspected PTE in spite of the recommendations and guidelines based on previously published reports. The negative D-dimer assay is a significant problem, and should not be used to triage patients with a high clinical index of suspicion for PTE. Furthermore, CTPA also has the added advantage of rapidly diagnosing or excluding other conditions which may clinically mimic PE, many of which are life threatening emergencies.
References
- Giuntini C, Di Ricco G, Marini C et al. Pulmonary embolism: Epidemiology. Chest. 107, 3S-9S (1995).
- Torbicki A, van Beek EJR, Charbonnier B et al. Task force report: Guidelines on diagnosis and management of acute pulmonary embolism. Eur. Heart. J. 21, 1301-1336 (2000)
- Richard HW. The epidemiology of venous thromboembolism. Circulation. 107, I-4 (2003).
- Conrad W, Michael MM, Albert JY et al. CT Angiography of pulmonary embolism: Diagnostic criteria and causes of misdiagnosis. Radiographics. 24, 1219-1238 (2004)
- Rathbun SW, Raskob GE, Whitsett TL. Sensitivity and specificity of helical computed tomography in the diagnosis of pulmonary embolism: A systematic review. Ann. Intern. Med. 132, 227-232 (2000).
- Dunn KL, Wolf JP, Drofman DM et al. Normal D-dimer levels in emergency department patients suspected of acute pulmonary embolism. J. Am. Coll. Cardiol. 40, 1475-1478 (2002).
- Hirai LK, Takahashi JM, Yoon HC. A prospective evaluation of a quantitative D-dimer assay in the evaluation of acute pulmonary embolism. J. Vasc. Interv. Radiol. 18, 970-974 (2007).
- Abcarian PW, Sweet JD, Watabe JT et al. Role of a quantitative D-dimer assay in determining the need for CT angiography of acute pulmonary embolism. AJR. Am. J. Roentgenol.182, 1377-1381 (2004).
- Klein J, Berland LL, Brink JA et al. ACR practice guideline for the performance and interpretation of computed tomography (CT) for the detection of pulmonary embolism in adults Revised 2005 (2005).
- Wildberger JE, Mahnken AH, Das M et al. CT imaging in acute pulmonary embolism: diagnostic strategies. Eur. Radiol. 15, 919-929 (2005).
- Gupta RT, Kakarla RK, Kirshenbaum KJ et al. D-Dimers and efficacy of clinical risk estimation algorithms: Sensitivity in evaluation of acute pulmonary embolism. AJR. Am. J. Roentgenol. 193, 425-430 (2009).
- Crowin MT, Donohoo JH, Partridge R et al. Do emergency physicians use serum D-dimer effectively to determine the need for CT when evaluating patients for pulmonary embolism? Review of 5,344 consecutive patients. AJR. Am. J. Roentgenol. 192, 1319-1323 (2009).
- Miller AC, Campbell IA, Fennerty A et al. British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax. 58, 470-484 (2003).
- Nilsson T, Soderberg M, Lundqvist G et al. A comparison of spiral computed tomography and latex agglutination D dimer assay in acute pulmonary embolism using pulmonary arteriography as gold standard, Scand. Cardiovasc. J 36, 373-377 (2002).
- Youssf ARI, Ismail MFM, ElGhamry R et al. Diagnostic accuracy of D-dimer assay in suspected pulmonary embolism patients. EJCT. 63, 411-417 (2014).