Research Article - Clinical Practice (2020) Volume 17, Issue 6
Evaluation of an endocrinology tele-medicine service during COVID-19
- Corresponding Author:
- Mathara Diddhenipothage Shani Apsara Dilrukshi Department of Endocrinology, Oxford Centre for Diabetes, Endocrinology and Metabolism, Churchill Hospital, Oxford University Hospitals, NHS Foundation Hospitals, United Kingdom E-mail: shani.mathara@ouh.nhs.uk
Abstract
The COVID-19 pandemic has brought exceptional challenges to health care providers across the globe requiring urgent alternative models of care to minimise interruptions to routine service. In this context orthodox practice of clinical endocrinology based upon face to face consultation, was converted to telemedicine. A rapid evaluation of this service was conducted to assess future utility in the post-pandemic period. Outcomes showed the majority of patients and clinicians were satisfied with telemedicine appointments and there was a reduced non-attendance rate when compared to a comparable pre-COVID face to face appointment cohort. Telemedicine was deemed appropriate for a sizable proportion of follow up visits, particularly for pituitary and thyroid disease. These findings favour an important role for telemedicine in future models of endocrinology outpatient care.
Keywords
COVID-19, endocrine outpatient services, telemedicine, clinician satisfaction, patient satisfaction
Introduction
The COVID-19 has created unprecedented challenges to health care; requiring urgent mobilization of acute services whilst trying to keep some semblances of routine care functioning. The universal challenges met by all specialty services were to comply with social distancing guidelines whilst continuing to deliver services with reduced manpower due to staff redeployment, shielding and sickness. Many specialties adapted services rapidly, with continued review of urgent patients and modified routine appointments to prevent the inevitable backlog when ‘normal’ services resumed. A key adaptation of our and many other endocrinology departments was the conversion of all appointments to Telemedicine (TM) to reduce patient footfall to the hospital and enable clinicians to work from home as far as possible.
Evidence of successful implementation of TM during the COVID19 pandemic is available from various specialties including orthopaedics, neurosurgery, oncology and adolescent services [1-4]. It is recognised as effective, feasible and well-received by patients and physicians alike. TM seemed unlikely to be useful prior to pandemic times in say, orthopaedics and neurosurgery where many management decisions seemed dependent on clinical examination; however, it still had a role. Similarly, TM was successfully used in oncology and adolescent services despite these specialties often requiring lengthy communication, perhaps more suited to Face To Face (FF) consultation.
This study aimed to provide a rapid service evaluation of the TM service instituted during the height of the COVID-19 pandemic at our department to inform future plans for remodeling of endocrinology services post COVID-19.
Methods
■ Setting
This prospective questionnaire based survey was completed by eight clinicians (4 consultants and 4 specialty registrars) who each did a minimum of four TM general endocrinology clinics during the month of June 2020.
■ Questionnaire
The questionnaire assessed clinician and patient satisfaction with 9 questions and also evaluated factors and outcomes such as access to blood tests, non-attendance rates and ability to discharge from the service.
■Clinic booking
Appointments took place in pre-existing clinic lists in morning or afternoon slots as previously booked. A member of the admin team contacted each patient in the week before to remind of the TM appointment. All appointments were conducted as telephone consultations.
■Patient cohort
Baseline patient clinical characteristics were collected on all patient contacts including the endocrine diagnosis.
■Comparator cohorts within the department
Departmental clinic data base
The departmental clinic database is coded for 7 diagnostic categories (Pituitary; Adrenal; Thyroid; Reproductive; Calcium and bone; Neuroendocrine tumours; ‘Other’) and was analysed to identify the proportion of endocrine outpatients in each diagnostic category. This was compared with the TM cohort to ensure the TM cohort was representative of our outpatient practice.
Pre-COVID Face to Face (FF) appointment cohort
To allow comparison to the pre-COVID service, retrospective Data on baseline clinical characteristics, diagnostic categories, discharge rates and non-attendance rates were collected for 4 general endocrinology clinic lists per clinician from January 2020. These lists were conducted by the same 8 clinicians.
■Statistics
Descriptive statistics were used to present data and IBM SPSS Statistics for Windows, Version 17.0 (IBM Corp., Armonk, N.Y., USA) statistical software package was used for data analysis.
Results
■Baseline characteristics
The TM cohort consisted of 402 patients Males (M)-160 (39.8%), Females (F)-240 (59.7%), missing data 2 (0.5%), with mean age 50.06 years (SD 19.97 years). The majority 302/402 (75.1%) of the sample were Follow up (FU) patients. The pre-COVID FF cohort was composed of 264 patients M-92 (34.8%), F-172 (65.2%) with mean age 50.16 years (SD 17.96 years). The majority 186/264 (70.5%) were FU patients similar to the TM cohort (TABLE 1).
| TM cohort | Pre-COVID Face to face cohort | |
|---|---|---|
| Males | 160 (39.8%) | 92 (34.8%) |
| Females | 240 (59.7%) | 172 (65.2%) |
| Median age | 49 years (Range 15-90 years) | 50.5 years (Range 17-89 years) |
| New patients | 99 (24.6%) | 78 (29.5%) |
| Follow up patients | 302 (75.1%) | 186 (70.5%) |
| Total | 402 | 264 |
TABLE 1. Base line characteristics of TM and Face to face cohorts (TM: Telemedicine).
Recent investigations were unavailable to review for 70.4% TM patient encounters and clinicians requested blood tests to be done in primary care for 48% of patients. Ninety two of the 402 patients (22.9%) were asked to attend the endocrine department for blood tests after the TM consultation.
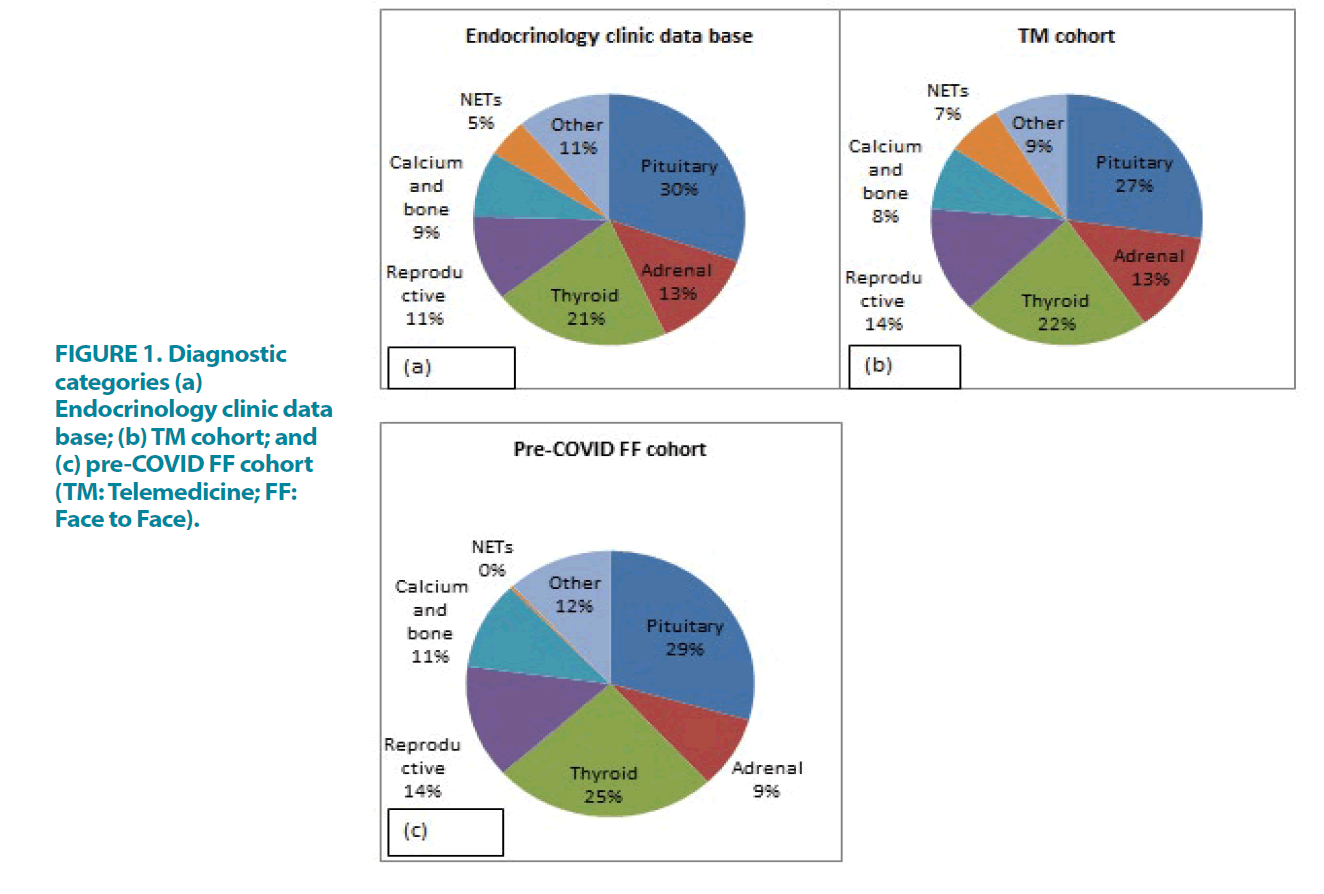
With regard to diagnostic categories, almost half of the TM patients had pituitary (27%) or thyroid disorders (22%). The diagnostic category spread was similar to the endocrine clinic database (N=3346 patients) confirming the TM cohort is representative of the out-patient activity in the endocrinology department. FIGURE 1).
Figure 1: Diagnostic categories (a) Endocrinology clinic data base; (b) TM cohort; and (c) pre-COVID FF cohort (TM: Telemedicine; FF: Face to Face).
■ Patient and clinician satisfaction with TM
The majority of patients [322/402 (80%)] were satisfied with a TM consultation, while 11% (44/402) were dissatisfied. The main reason cited by patients for FF preference was being ‘more comfortable with face to face discussion’ (TABLE 2).
Category |
Follow up | New | Total |
|---|---|---|---|
| Patients satisfied with TM consultation | 251 (82.8%) | 71 (71.7%) | 322 (80%) |
| Patients not-satisfied with TM consultation | 30 (9.9%) | 14 (14.1%) | 44 (11%) |
| Patient satisfaction status unknown | 9 (3%) | 2 (2%) | 11 (3%) |
| Missing data | 13 (4.3%) | 12 (12.1%) | 25 (6%) |
| Reasons for patient dissatisfaction (44/402) | |||
| communication problems | 4 (9.0%) | 1 (2.27%) | 5 (11.3%) |
| more comfortable with FF discussion | 20 (45.4%) | 5 (11.3%) | 25 (56.8%) |
| prefer to get blood tests from OCDEM | 2 (4.54%) | 2 (4.54%) | 4 (9.0%) |
| Reason for dissatisfaction is not recorded | 4 (9.0%) | 6 (13.6%) | 10 (22.7%) |
| Total | 30 (68.1%) | 14 (31.8%) | 44 (100%) |
| TM: Telemedicine; FF: Face to Face; OCDEM: Oxford Centre for Diabetes, Endocrinology and Metabolism | |||
TABLE 2. Patient’s satisfaction regarding TM consultation.
Clinicians were satisfied with TM for 63% [254/402] of appointments, though this is more pronounced in FU patients (70.5%). Clinicians reported not being satisfied with TM consultations for over half of new patients [51/99 (51.5%)] (TABLE 3). Difficulty to perform clinical examination [74/132 (56%)] was the highest cited reason for physician dissatisfaction followed by unavailability of investigations to review tests [22/132 (16.6%)] and communication difficulties [15/132 (11.3%)]. Endocrine conditions of the pituitary (25%) or thyroid (25%) were the most common diagnoses when clinicians deemed TM consultation satisfactory.
| New/Follow up | |
| 1 | Endocrine diagnosis/Presenting complaint |
| 2 | Were recent blood results available to review Y/N |
| 3 | Did you request bloods at GP (Y/N) |
| 4 | Did you request bloods in OCDEM (Y/N) |
| 5 | Clinician satisfied with TM-Y/N |
| 6 | Clinician satisfied with TM-If N please give details |
| 7 | Patient satisfied with TM-Y/N |
| 8 | Patient satisfied with TM-If N please give details |
| 9 | Is next OPA appropriate as TM Y/N |
| FU: Follow Up; Y: Yes; N: No; GP: General Practitioner; OCDEM: Oxford Centre for Diabetes, Endocrinology and Metabolism; TM: Telemedicine | |
TABLE 3. Survey questionnaire.
Type of the cohort |
Category of patients | Attended for consultation | Non-attendance/unable to contact | Total |
|---|---|---|---|---|
| TM cohort | Follow up | 291 (72.4%) | 11 (2.7%) | 302 (75.1%) |
| New | 95 (23.6%) | 4 (1%) | 99 (24.6%) | |
| Total | 387 (96.3%) | 15 (3.7%) | 402 (100%) | |
| FF cohort | Follow up | 167 (63.3%) | 19 (7.2%) | 186 (70.5%) |
| New | 72 (27.3%) | 6 (2.3%) | 78 (29.5%) | |
| Total | 239 (90.53%) | 25 (9.5%) | 264 (100%) | |
| TM: Telemedicine; FF: Face to Face | ||||
TABLE 4: Clinic attendance rates of the TM cohort and FF cohort.
■ Clinic outcomes
Clinicians reported 162/402 (40.3%) patients appropriate for TM follow up (rather than FF) at the end of TM appointments. In comparison to pre-COVID FF cohort, non-attendance rates were significantly lower in the TM cohort [15/402 (3.7%) vs. 25/264 (9.5%), p=0.004] while there was no significant difference in discharge rates [68/402 (16.9%) vs. 47/264 (17.8%); p=0.843).
Discussion
Until recent times, TM was predominantly used in rural medical care services where distance to quality medical care was a recognised barrier to health care delivery [5]. During the COVID-19 pandemic, TM proved to be a successful model of care and was rapidly put into practice by many endocrine departments in the UK.
Our study shows the majority of patients (80%) and clinicians (63%) were satisfied with the TM-endocrine service confirming it as a viable alternative to traditional FF consultation. Findings of a similar survey in sports medicine [6] showed significantly high patient (95.0%) and clinician (92%) satisfaction with TM and a sizable majority of patient (80%) from a rare cancer unit study preferred at least some future appointments to be TM [3].
Patients’ most commonly reported reason for dissatisfaction with TM was ‘would feel more comfortable with FF discussion’. There are obvious benefits to FF interaction: better opportunities to establish rapport, sensitive communication of worrying results, advantages of non-verbal cues and communication. This may be an area where video consultation has an increasing role to give the benefit of a more personal interaction.
Inability to perform clinical examination was our top cited (56%) reason for clinician dissatisfaction, a limitation also reported by others [4]. Video provides a possible alternative: Alexander et al. successfully used video interfacing with common electronic medical record platforms as a virtual tool for clinical examination including standard wound and range-of-motion checks in an orthopedic service [1]. Similarly, effective video neurologic examinations and TM services are already established in tele-stroke care with benefits including shorter duration of hospital stay, rapid access to rehabilitation assessments, diagnostic testing and imaging when compared to standard stroke unit care [2].
Inability to access contemporaneous blood results is a common issue in TM and we found this a limiting factor in 70.4% TM appointments. This highlights the importance of developing better hub phlebotomy centres and having the IT infrastructure to overcome any limitation on investigations posed by not having a patient physically in the clinic. Following their TM appointment, 23% of our patients were asked to attend the department for lab tests which negates the key purpose of TM. Better triaging systems should identify where blood tests will affect clinic outcome and hence be arranged prior to TM.
Communication issues were cited in 11% of clinician dissatisfaction surveys and perhaps this is most relevant in ‘breaking bad news’ consultations as confirmed by the oncology clinic study where almost half (48%) preferred FF consultation [3]. Inability to maintain privacy and confidentiality during TM consultations was also a challenge experienced by care providers in the adolescent’s clinic survey and to address this, they encouraged use of headphones, yes/no questions and the Zoom chat function [4]. Video consultation is also being increasingly utilised to better facilitate communication.
To assess the efficiency of TM service, we compared clinic outcomes of the TM cohort with the pre-COVID FF cohort. We predicted a possible reluctance to discharge patients post TM review, but we found this not to be the case. There was no significant difference in discharge rates between two cohorts. Additionally, nonattendance rate was found to be lower in the TM cohort in comparison to FF cohort. This is similar to published data in the sports medicine clinic with a ‘no show rate’ of only 2.8% [6]. This may be due to the fact that in our study the patient was alerted in the week before, confirming their TM appointment as well as the higher likelihood of contact via phoning the patient as opposed to expecting physical attendance. Thus similar discharge rates and lower non-attendance rates support TM as an efficient mode of care delivery.
Other published challenges associated with TM are technology issues, requirements for training and need for guidelines on enhanced documentation, communication and information governance [5,7,8]. Since COVID-19, the RCP, GMC and medical defence organisations have published basic guidance on conducting TM consultations, highlighting key pitfalls [9].
We acknowledge our study limitations, which was conducted as a simple survey by clinicians delivering the TM. This could lead to bias as patients are more likely to give dissatisfaction feedback to an anonymised source. However, it was important to ascertain patient satisfaction at that stage in order to see if further TM followup was appropriate. Despite short timeframe, our TM sample was of a reasonable size and representative of the endocrinology out-patient service, making the data useful for future planning. By collecting data from multiple consultants and specialist registrars we limited the impact of individual practice or experience on study outcomes.
Conclusion
We find high patient and clinician satisfaction with the TM service instituted during the COVID-19 pandemic with lower nonattendance rate when compared to pre-COVID FF appointments, supporting incorporation of TM into longer term plans for outpatient Endocrinology. This practice could be nuanced by subcategorising patients better suited to TM follow up (stable patients under long term follow up) versus those more appropriate for FF appointments (new patients or those where clinical examination needed). In a healthcare system increasingly using virtual and digital means of communication, we urgently require the inter-Trust IT infrastructure to enable systems to ‘talk’ to one another and maximise efficiency. As we contend with an impending second ‘wave’ of COVID-19, this data supports continued use of TM in endocrinology outpatient care as a practical, efficient and effective longer-term model.
Conflict of Interest
The authors declare that there is no conflict of interest.
Details of Author Contributions
B, supervised the Quality Improvement Project (QIP), A and B designed and implemented the QIP, A, analysed data and drafted the manuscript and both A and B contributed to the final version of the manuscript.
Acknowledgements
Authors would like to acknowledge Dr Christine May, Dr Bahram Jafar-Mohammadi and Professor David Ray as well as the rest of the SpR and clinical team who helped with the data collection and review of TM pathway for the purpose of this QIP.
References
- Loeb A, Rao S, Ficke J, et al. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 28, e469-e476 (2020).
- Blue R, Yang A, Zhou C, et al. Telemedicine in the era of coronavirus disease 2019 (COVID-19): A neurosurgical perspective. World Neurosurg. 139, 549-557 (2020).
- Smrke A, Younger E, Wilson R, et al. Telemedicine during the COVID-19 pandemic: Impact on care for rare cancers. JCO Global Oncology. 6, 1046-1051 (2020).
- Barney A, Buckelew S, Mesheriakova V, et al. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: Challenges and opportunities for innovation. J Adolesc Health. 67, 164-171 (2020).
- Iyengar K, Jain V, Vaishya R. Pitfalls in telemedicine consultations in the era of COVID 19 and how to avoid them. Diabetes Metab Syndr. 14, 797-799 (2020).
- Tenforde A, Iaccarino M, Borgstrom H, et al. Telemedicine during COVID-19 for outpatient sports and musculoskeletal medicine physicians. PMR. 12, 926-932 (2020).
- Bashshur R, Doarn C, Frenk J, et al. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 26, 571-573 (2020).
- Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 27, 957-962 (2020).
- Remote Consultations. General Medical Council. (2020). [Available at: https://www.gmc-uk.org/ethical-guidance/ethical-hub/remote-consultations].