Short Communication - Diabetes Management (2018) Volume 8, Issue 2
Families with diabetes under poverty threshold
- *Corresponding Author:
- Diana L. Malkin-Washeim
Director-Nutritional Services
Bronx Care Diabetes Center of Excellence Bronx
NY 10457, USA
E-mail: dwasheim@bronxleb.org
Abstract
Short Communication
The United Nations (UN) adopted the Convention of the Rights of the Child (CRC) in 1989 [1]. The CRC helps shape the way we view children, create an environment that is safe and protect all children from neglect, exploitation and abuse. The provisions include that every child enjoy the highest attainable standard of health [2].
Diabetes and Poverty
There are 1.25 million Americans living with type 1 diabetes (T1D) including approximately 200,000 children under 20 years old. Five million people in the U.S. are expected to have T1D by 2050, including nearly 600,000 youth [3]. An estimated 387 million people have diabetes worldwide, of which T1D accounts for between 5% and 10%. However, the prevalence of T1D is increasing worldwide [4]. Alongside the rise of diabetes, there is an increase rate of obesity and Type 2 diabetes among children [5,6]. In September 2017, the U.S. Census Bureau reported that the national poverty rate decreased 0.8 percentage points [7]. In 2015, more than 43 million people lived below the poverty threshold in the U.S. and of those, 14.5 million were children (4). The poverty threshold reflects the estimated number of Americans living in poverty each year, and poverty guidelines refer to the corresponding eligibility for specific federal programs [8,9]. In the U.S., Americans spend less than 10% on food [10]. According to the Foundation for International Community in 2016, three billion people live on less than $2.50 per day and more than 1.2 billion live in extreme poverty, living on less than $1.25 per day [10].
40 million children worldwide live without adequate shelter and 270 million children have no access to health services [11].
Poverty over time
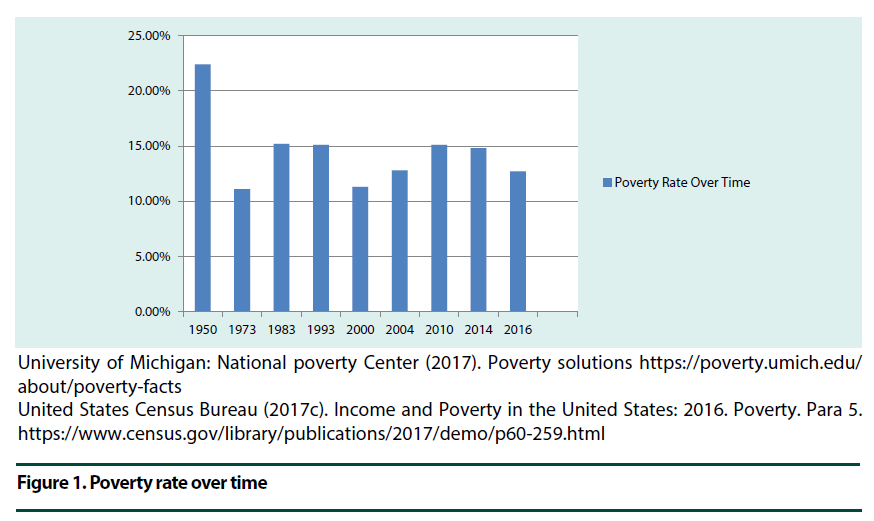
The poverty rate for Americans have fluctuated from 22.4% in the 1950s to as low as 11.1% in the early 1970s reaching a peak level of 15.2% in the 1980s then dipping to 12.7% in 2016 (Figure 1) [12,13].
University of Michigan: National poverty Center (2017). Poverty solutions https://poverty.umich.edu/about/poverty-facts
United States Census Bureau (2017c). Income and Poverty in the United States: 2016. Poverty. Para 5. https://www.census.gov/library/publications/2017/demo/p60-259.html
Figure 1. Poverty rate over time
Weight among Children
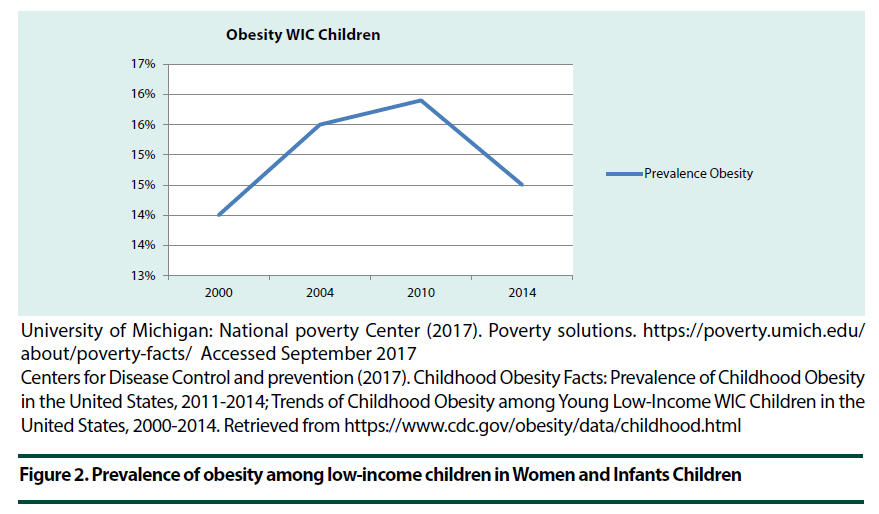
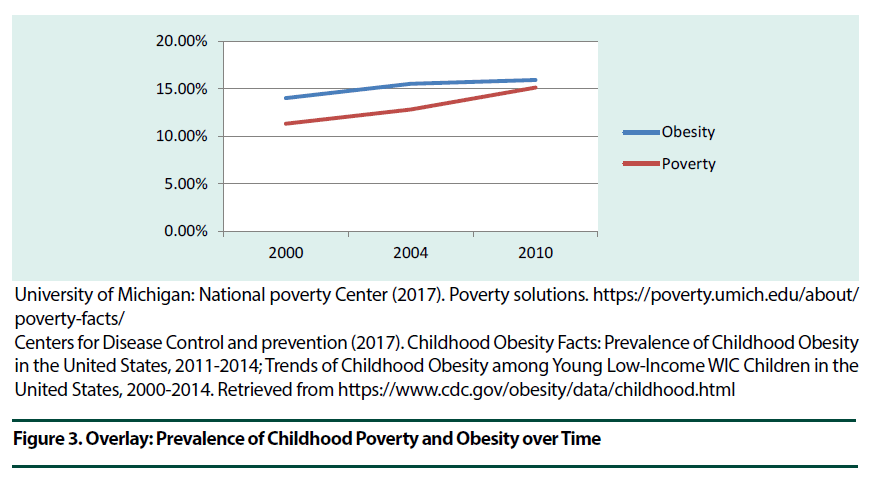
Since 1980 the prevalence of obesity has doubled in more than 70 countries, with a greater increase of obesity occurring in children than that of the adult population. In 2015 there were approximately 108 million children living with obesity worldwide [5]. The Centers for Disease Control and Prevention (CDC) reported that “during 2000–2010, the overall prevalence of obesity among young low-income children in Women, Infants and Children (WIC) increased significantly [14] (Figure 2). It appears that there is a linear relationship over time between poverty rates and obesity among low- income children in WIC (Figure 3). Since the 1970s, children with obesity in the U.S. have more than tripled, and currently, one in five school-aged children (ages 6 – 19) has obesity [15].
University of Michigan: National poverty Center (2017). Poverty solutions. https://poverty.umich.edu/about/poverty-facts/ Accessed September 2017
Centers for Disease Control and prevention (2017). Childhood Obesity Facts: Prevalence of Childhood Obesity in the United States, 2011-2014; Trends of Childhood Obesity among Young Low-Income WIC Children in the United States, 2000-2014. Retrieved from https://www.cdc.gov/obesity/data/childhood.html
Figure 2. Prevalence of obesity among low-income children in Women and Infants Children
University of Michigan: National poverty Center (2017). Poverty solutions. https://poverty.umich.edu/about/poverty-facts/
Centers for Disease Control and prevention (2017). Childhood Obesity Facts: Prevalence of Childhood Obesity in the United States, 2011-2014; Trends of Childhood Obesity among Young Low-Income WIC Children in the United States, 2000-2014. Retrieved from https://www.cdc.gov/obesity/data/childhood.html
Figure 3. Overlay: Prevalence of Childhood Poverty and Obesity over Time
Food Patterns
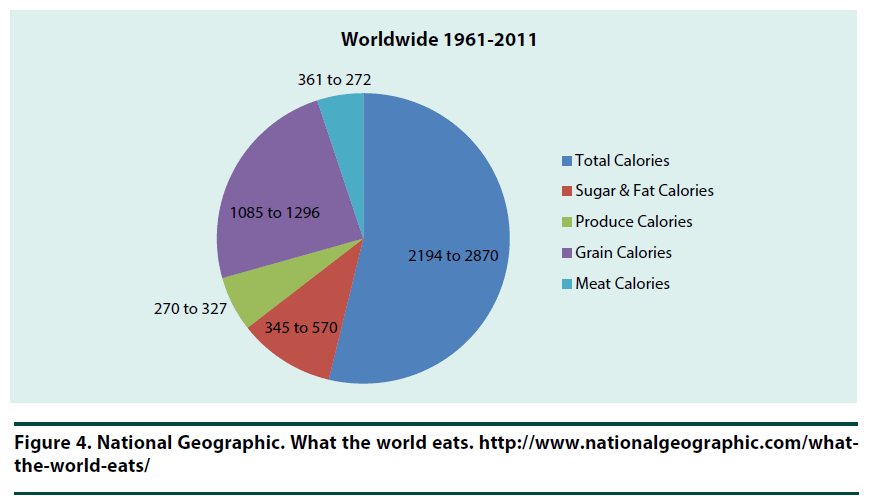
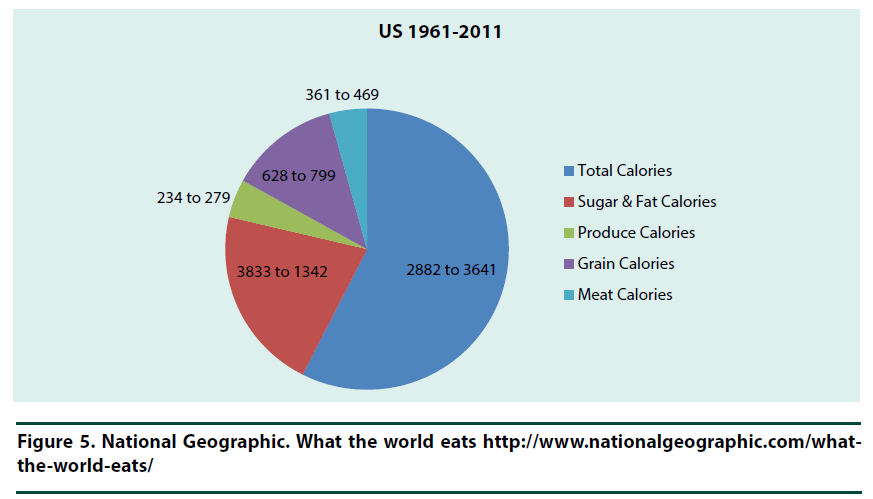
Food patterns change over time due to the environment (such as natural disasters and culture), as well as housing, economic and political events. Food patterns provide an overall view of caloric consumption which equates to energy, and ultimately, potential insight into food access and behavior. However, these patterns do not focus on specific nutrients. Food patterns have shifted worldwide over the last 50 years (1961 to 2011) (Figure 4). In the US, there was a shift of total calories (from 2882 to 3641) (Figure 5). Fruits and vegetable consumption has not changed significantly, remaining at 8% of total calories consumed. The U.S. consumes more meat than any other country second to China, with poultry reported as the fastest growing preferred meat of choice [16].
Figure 4. National Geographic. What the world eats. http://www.nationalgeographic.com/what-the-world-eats/
Figure 5. National Geographic. What the world eats http://www.nationalgeographic.com/what-the-world-eats/
Psychosocial
Given the cost of food, housing, utilities, health insurance and the portfolio of diabetes technology that has entered mainstream healthcare of recent years, it is imperative that every child and their family not only survives but also thrives. Both T1D, an autoimmune disease dependent on insulin, and Type 2 diabetes (T2D), relative to multiple risk factors that include family history, weight, dietary indiscretions, high blood pressure and ethnicity [17], elevate stressors on families that may already have multiple stressors such as food insecurity, limited financial resources, unemployment and other disruptive life events such as incarceration, shelter living, transient housing and mental health conditions [18]. When a family is living under the poverty threshold and their child is diagnosed with diabetes, it sets the stage for multiple challenges including: limited financial resources; food insecurity; needle phobia; anxiety, depression, eating disorders; control issues; and stress. The above stressors can affect the mental and emotional wellbeing of the entire family. Stress can also affect the body’s physical status inducing the onset of headaches, muscle pain or tension, sleeping too much or too little, general feelings of illness, fatigue, discouragement, irritability, depression, restlessness, lack of concentration, memory loss and anxiety. The child with diabetes and their sibling(s) may experience symptoms that are out of character, such as withdrawing from friends and family, eating too much or too little, acting out in anger, drinking alcohol to excess, smoking tobacco and using drugs [19]. In addition, responsive feeding practices may be affected by poverty where parents are not practicing “responsive feeding practices” [20] between the child and caregiver and this has been associated with the development of poor dietary habits and/or increased childhood obesity [20]. Food insecurity impacts a child’s health long term and can negatively affect development, physical functioning and behavior. According to the American Academy of Pediatrics children living in food insecure households are more likely to experience “stress, depression and anxiety; worse overall health; more hospitalizations when three years old or younger; iron deficiency; lower bone density in preadolescent boys; obesity due to lack of access to healthy foods; lower cognitive skills; developmental problems affecting school performance; and malnutrition that can lead to diabetes, hyperlipidemia and cardiovascular disease later in life” [21,22]. The time period after diagnosis can be challenging for families. There are feelings that may include denial, depression, anger, shock, sadness, fear and guilt. Children may fear of punishment in that they did something wrong [23].
Strategy Tips for Families: Remind, Encourage and Participate
1. Learn about diabetes while taking the time to acclimate to diagnosis and reinforcing positivity
2. Participating in supplemental assistance programs: Supplemental Nutrition Assistance Program (SNAP), Welfare or Temporary Assistance for Needy Families (TANF), Medicaid and Children’s Health Insurance Program (CHIP), Public Housing (affordable apartments for low-income families) and the Housing Choice Voucher Program (Section 8) (a family may find their own place and use a voucher to pay for all or part of the rent
3. Sharing diabetes knowledge with friends and family
4. Taking control over their diabetes management
5. Joining a support group
6. Exploring available resources, e.g., diabetes camp
7. Encouraging feelings-focused dialogue and discussion
8. Being emotionally present, for example, asking what specifically the child or family member(s) would like to work on
9. Asking the child or family member(s) if they have or are experiencing any fear(s)
10. Avoiding blame placement
11. Focusing on the child as a whole person and not someone with diabetes
12. Encouraging the exploration and use of mental health resources
Screening/Assessment Tool
Conducting a thorough assessment will help screen for psychosocial issues, prevalent socioeconomic influences and nutrition deficiencies by including:
A. A 24-hour dietary recall (provides a snap-shot in time)
B. Asking questions including: 1) Are you feeling down, sad or hopeless (Yes or No)? 2) Do you have little interest or pleasure in doing things (not at all, several days per week, or nearly daily)? and 3) Have your sleep patterns changed (none or to little sleep or too much sleep)?
C. Asking caretaker questions including: 1) Who do you live with? and 2) Do you have a para or care-taker?
D. Asking questions including: Are you receiving public assistance, e.g., child support, SNAP and/or social security disability?
E. Identifying families with young children as being at risk for food insecurity by asking food insecurity questions: 1)
Within the past 12 months have you worried whether your food would run out before you got money to buy more? and 2) Within the past 12 months has the food you bought lasted? If no, did you have money to get more? [21,24] (Answers include often true, sometimes true, or never true)
F. Asking social support questions: 1) Who checks in on you? and 2) What is your biggest fear regarding diabetes? (These two questions may open up a dialogue about social services, and what level of support there is from family and friends)
We can support our children with diabetes and their families living under the poverty threshold with community resources, education and providing social support. As professionals, we need to maintain our code of ethics which is to support and promote high standards of our professional practice for the benefit of clients and the public [25].
References
- The WORLD Policy Analysis Center. CRC 25th Anniversary.
- Brink S, Wei Rhen Warren Lee, Pillay K et al. Diabetes in children and adolescents. International Society for Pediatric and Adolescent Diabetes (ISPAD), 1st edition (2010).
- JDRF. Type 1 Diabetes Facts (2017).
- You W, Henneberg M (2016) Type 1 diabetes prevalence increasing globally and regionally: the role of natural selection and life expectancy at birth. BMJ. Open. Diabetes. Res. Care. 4(1), e000161 (2016).
- The GBD 2015 Obesity Collaboration. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377(1), 13–27 (2017).
- National Institute of Diabetes and Digestive and Kidney Diseases (N.D.) Diabetes in Children and Teens.
- United States Census Bureau (2017a). Income, poverty and health insurance coverage in the United States: 2016.
- https://www.census.gov/library/publications/2016/demo/p60-256.html
- United States Department of Health & Human Services: Office of The Assistant Secretary for Planning and Evaluation (2016). U.S. Federal poverty guidelines used to determine financial eligibility for certain federal programs.
- Proctor B, Semega J, Kollar M. U.S. Department of Commerce Economics and Statics Administration: Census Bureau, pp: 60-256.
- https://poverty.umich.edu/about/poverty-facts/
- United States Census Bureau (2017c). Income and Poverty in the United States: 60-259 (2016).
- Centers for Disease Control and prevention (2017). Childhood Obesity Facts: Prevalence of Childhood Obesity in the United States, 2011-2014; Trends of Childhood Obesity among Young Low-Income WIC Children in the United States, 2000-2014.
- https://www.cdc.gov/healthyschools/obesity/facts.htm.
- http://www.nationalgeographic.com/what-the-world-eats/
- https://www.niddk.nih.gov/health-information/diabetes/overview
- Jackson DB, Vaughn MG (2017) Parental history of disruptive life events and household food insecurity. J. Nutr. Educ. Behav. 49 (7), 554–560 (2017).
- http://www.healthline.com/health/diabetes-and-stress#overview1(2016)
- Robert Wood Johnson Foundation (2016) Feeding guidelines for infants and young toddlers: A responsive parenting approach. Executive summary. pp: 1-23.
- American Academy of Pediatrics. Identifying food insecurity: Two-question screening tool has 97% sensitivity. AAP News.
- O’Keefe L. American Academy of Pediatrics. Identifying food insecurity: Two-question screening tool has 97% sensitivity. AAP News. http://www.aappublications.org/content/early/2015/10/23/aapnews.20151023-1
- Ogle G, Middlehurst A, Silink M et al. Pocketbook for management of diabetes in childhood and adolescence in under-resourced countries, 2nd ed. Brussels: International Diabetes Federation (2017).
- Children’s Health Watch: Policy action brief. The Hunger Vital Sign: A new standard of care for preventive health.http://www.childrenshealthwatch.org/wp-content/uploads/FINAL-Hunger-Vital-Sign-2-pager1.pdf May 2014.
- http://www.eatrightpro.org/resources/practice/code-of-ethics