Research Article - Neuropsychiatry (2018) Volume 8, Issue 1
Fear Avoidance Beliefs and Disability among Women with Low Back Pain
- Corresponding Author:
- Syamala Buragadda
Rehabilitation Health Sciences Department, College of Applied Medical Sciences, King Saud University, Riyadh, KSA 11433, PO box 10219, Saudi Arabia
Tel: +966 531262956
Abstract
Abstract
Background: Low back pain (LBP) is common among females. Many factors are associated with different levels of disability caused by low back pain, including Fear avoidance behavior. The fear avoidance beliefs of women with chronic low back pain are not clear. The objective of this cross-sectional study was to assess the disability level and fear avoidance beliefs of women with chronic LBP.
Methods: This was a cross-sectional survey of 227 females with chronic LBP. Demographic information was obtained from each participant. Disabilities due to LBP and fear-avoidance beliefs were assessed using the Oswestry Disability Index (ODI) and the Fear Avoidance Belief Questionnaire (FABQ), respectively. Descriptive data were analyzed using the chi-square test and an ANOVA for continuous variables.
Keywords
Avoidance beliefs, Back pain disability, Chronic pain, Health advice, Physical activity
Introduction
Low back pain (LBP) is one of the most common problems, with more than 70% individuals experiencing it at least once in their lifetime. It also epitomizes a major medical, social and economic health issue globally [1]. It is defined as “pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without sciatica, and is considered chronic when it persists for 12 weeks” [2]. It was argued that chronic back pain lasts for more than 7–12 weeks beyond the expected period of healing, and it may not have well-defined underlying pathological causes [3]. Some clinicians consider frequently recurring back pain as chronic pain as it intermittently affects an individual over a longer period. The rate of incidence among US population was 1.39 per 1000 individuals and it accounted for 3.15% of all visits to the emergency department [4]. Despite the fact that there are few studies on LBP and its disability in the Kingdom of Saudi Arabia, a survey conducted by Alshami showed that problems at the lumbar spine is one of the most common spinal disorders in Saudi Arabia, with a prevalence of 53.1% [5]. It was also observed that the prevalence is high in Saudi females as compared to that in males [6]. Vitamin D deficiency is considered a major contributor for chronic LBP among Saudis, especially among women [7]. Similarly, work-related LBP was studied among nurses working in the Taif region of Saudi Arabia, and it was found that LBP led to increased rates of sick leaves [8,9]. Pain is one of the most common and persisting symptoms in humans that may be linked to fear [10]. According to the gate-control theory of pain, the perception of pain varies among individuals depending on their mood, emotional condition, and prior experience [11]. Recently, substantial attention has been paid to the role of cognitive factors in the development of chronic LBP and disability. The development of a disability may proceed from it being merely a medical condition to leading to activity limitation or restricted participation. The fear-avoidance model provides a cognitive-behavioral framework to recognize why some patients with LBP develop persistent disability. Additionally, it explains how pain-related attitudes and beliefs, in particular, catastrophic clarifications of a pain experience, can actually lead to avoidance of movements and activities, which in turn, adds to the disability [12]. Fear avoidance may lead to interference in activities of daily living (ADL) and may play an active role in the transition from acute to chronic pain [13,14]. It has been demonstrated that fear-avoidance beliefs were linked to the degree of disability, and that those with higher fear-avoidance beliefs have a higher level of disability [15]. Another study recommended that fear avoidance beliefs need to be considered in the management of pain and disability caused by LBP [16]. Previous studies have reported that patients with chronic LBP were more fear-avoidant, reported severe disability, and displayed less lumbar flexion than pain-free individuals [17]. Religious factors also affect health behaviors and beliefs. However, there is a lack of evidence about fear avoidance and health beliefs among Arab women [18]. Hence, we aimed to assess the correlation between disability and fear avoidance beliefs among Saudi women with chronic LBP.
Methods
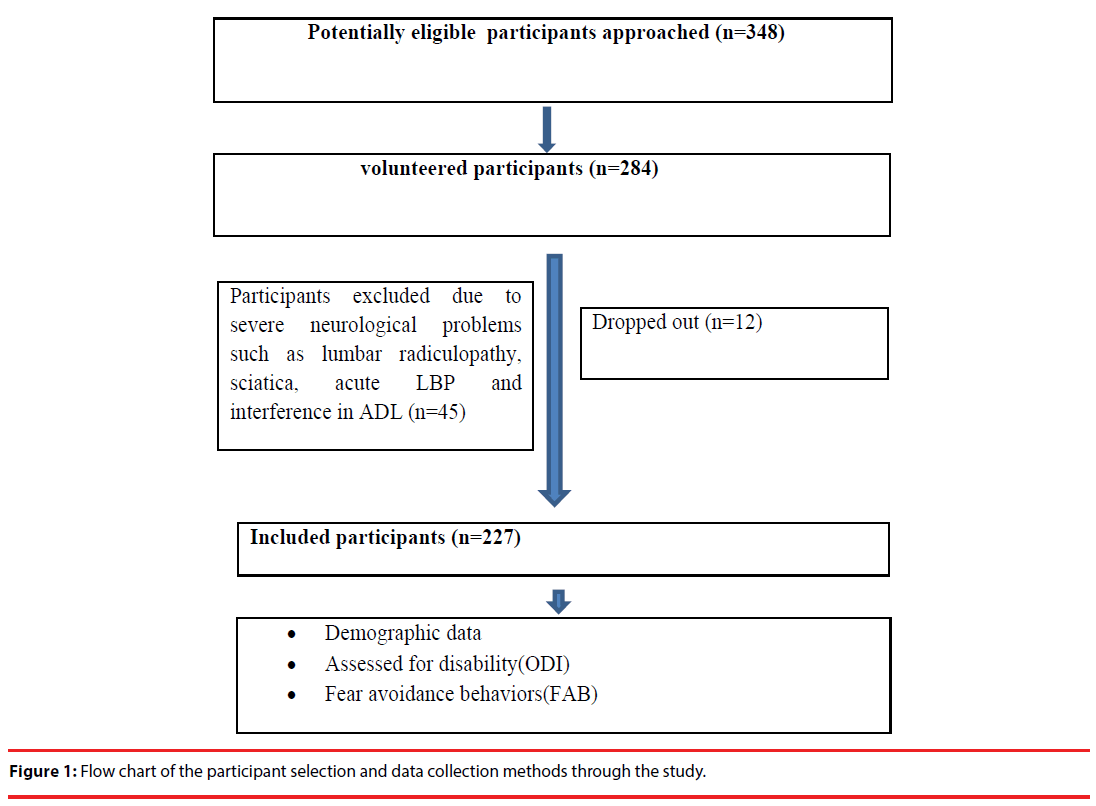
This was a cross sectional observational study. Out of 284 Saudi women volunteered to participate, only 227 were enrolled in the study (Figure 1). They ranged in age from 20 to 60 years. A power analysis was conducted to determine the sample size based on the prevalence of non-specific LBP (for more than 3 months) among Saudi females. Subjects with a history of non-specific chronic LBP for more than three months and without any neurological symptoms, and who were able to read and understand Arabic or English were included in the sample. Those with a history of acute or sub-acute LBP, or any condition affecting their daily activities, were excluded. Participants were recruited from different health care centers and pain clinics in Riyadh. The study was conducted in 2015. All the participants provided written informed consent, and the Institutional Review Board of King Saud University approved the study protocol. Demographic data such as age, job description, number of LBP episodes in the last year, their need to seek health advice, and any interference with normal daily activities were recorded. Selfadministered questionnaires such as the Oswestry Disability Index (ODI), and fear-avoidance beliefs questionnaire (FABQ) were used to measure disability and fear avoidance beliefs, respectively.
▪ Disability due to low back pain
The ODI was used to measure the disability caused by LBP. The ODI is one of the most commonly used outcome measures for individuals with LBP. The modified ODI (version 2.0) is a self-administered questionnaire that requires 5 minutes to complete and 1 minute to score. Reliability is reported to range from ICC=.84–.94, and the internal consistency Cronbach’s α ranges from .71 to .87. The total score is expressed as a percentage, with a higher score representing a higher level of disability [19]. Percentage scores of 0–20% indicate minimal disability, those from 21–40% indicate moderate disability, those from 41–60% indicate severe disability, and those from 61–80% indicate being crippled.
▪ Fear avoidance beliefs
Fear avoidance was measured using the FABQ. It contains 16 items, scored from 0–6 (completely agree to completely disagree). It consists of two subscales, the physical activity subscale (FABQ PA), scored out of 24 (scores of ≤15 indicate low and >15 indicate high fear avoidance), and work (FABQ W), scored out of 42 points (scores of ≤34 indicate low and >34 indicate high fear avoidance). The reliability of the FABQ-PA and FABQ-W was reported to be 0.72 to 0.90 and 0.8 to 0.91, respectively. Additionally, the total FABQ was reported to have a reliability score of 0.97. Both FABQ-W and FABQ-PA have a good internal consistency (α = 0.90 and 0.81, respectively) and acceptable construct validity [20].
Statistical Analysis
Descriptive data were analyzed using the chi-square for categorical data and an ANOVA for continuous variables. In order to test the role of demographic variables in scores on the self-reported disability and fear avoidance levels, a multiple regression analysis was performed with scores on the ODI and FABQ as dependent variables. In addition to performing the sub group analysis on scores of individuals with different levels of disability, the Pearson correlation was used to examine the relationship between the ODI and FABQ scores. The missing data was assigned a code of 99, and other variables were correlated to reduce non-response bias. The analyses were performed using the SPSS-21 software. P values of less than .05 were considered significant.
Results
In total, 348 potentially eligible participants were identified, out of which, only 284 participants volunteered to participate. They were screened and 45 participants were excluded as they did not meet the inclusion criteria, and twelve dropped out during the study (Figure 1).
Finally, the 227 participants were divided into four groups. The descriptive characteristics of the sample have been presented (Table 1).
| Minimal disability N(%) | Moderate disability N(%) | Severe disability N(%) | Crippled N (%) | |
|---|---|---|---|---|
| Sample n (%) | 152 (67) | 57 (25.1) | 15 (6.6) | 3 (1.3) |
| Age groups | ||||
| 20-39 Years; M±SD [24.2± 4.1] | 139 (91.4) | 36 (63.1) | 2 (13.4) | 1 (33.3) |
| 40-60 Years; M±SD [47.4±4.8] | 13 (8.5) | 21 (36.8) | 13 (86.6) | 2 (66.6) |
| Type of job | ||||
| Home makers | 11 (7.2) | 22 (38.5) | 9 (60) | 3 (100) |
| Students | 98 (64.4) | 13 (22.8) | - | - |
| Working women | 43 (28.2) | 22 (38.5) | 6 (40) | - |
| Previous LBP Episodes | ||||
| 1-3 episodes | 29 (19) | 8 (14) | 4 (26.6) | - |
| 4-10 episodes | 54 (35.5) | 11 (19.2) | 2 (13.3) | - |
| < than 10 episodes | 69 (45.3) | 38 (66.6) | 9 (60.1) | 3 (100) |
| Did they seek health professional advice? | ||||
| Yes | 39 (25.6) | 29 (50.9) | 12 (80) | |
| No | 113 (74.3) | 28 (50.1) | 3 (20) | 3 (100) |
| Interference in activities of daily living | ||||
| Yes | 61 (40.1) | 47 (82.4) | 15 (100) | 3 (100) |
| No | 91 (59.8) | 10 (17.5) | - | - |
| ODI scores; [M±SD] | 5.7 (2.7) | 15.2 (2.8) | 23.8 (2.9) | 33.7 (1.2) |
| FABQ-PA scale [M±SD ] | 9.5 (5.9) | 13.3 (6.5) | 15.4 (8.2) | 3.5 (18.3) |
| Low category FABQ-PA | 126 (82.8) | 36 (63.1) | 6 (40) | 1 (33.3) |
| High category FABQ-PA | 26 (17.1) | 21 (36.8) | 9 (60) | 2 (66.6) |
| FABQ-W Scale [ M±SD] | 15.09 (10.2) | 18.39 (10.2) | 24 (13.7) | 30.7 (4.0) |
| Low category FABQ-W | 145 (59.3) | 55 (96.4) | 11 (73.3) | 2 (66.6) |
| High category FABQ-W | 7 (4.7) | 2 (3.6) | 4 (26.7) | 1 (33.3) |
Table 1: Demographic characteristics of the sample.
In a pooled sample of participants with LBP, the participants were divided into the following four subgroups based on their ODI score: minimal disability (n = 152), moderate disability (n = 57), severe disability (n = 15) and crippled (n = 3). The majority of participants in the minimal disability group were students, aged between 20 and 40 years, most of them had not sought any health professional advice, and most had not reported any interference in their daily activities due to LBP. More than half of the low disability group had a low-level of FABQ scores on both physical activity and work. Unlike the individuals with minimal disability, the moderate disability group had an equal number of homemakers and workers, most participants were aged in the range of 20 to 40 years, and most of them reported interference in their ADLs. Majority of them had more than 10 episodes of LBP during the last year, and half of them had sought health professional advice. The severe disability group mostly comprised homemakers, participants aged between 41 and 60 years, and those with a high number of LBP episodes in the last year. A greater proportion of severe and crippled groups reported that they sought health professional advice, and that LBP interfered with their routine activities.
A chi-square test was conducted to determine the association between the categorical variables. Increased age was significantly associated with the history of LBP, seeking health advice, and interference in daily activities. No significant association was found between job description and other variables, except for interference in daily activities. A higher frequency of episodes of LBP was associated with increased frequency in seeking health advice and greater interference in daily activities. The level of significance was set at .05.
Descriptive data were compared for those with different levels of disability using a one-way ANOVA for the continuous data. There was a difference in age, type of job, number of LBP episodes, seeking health advice, and daily activity interference between and within the groups (p < .05) (Table 2).
| Variables | Sum of Squares | df | Mean Square | F | Sig. | |
|---|---|---|---|---|---|---|
| age | Between Groups | 27.115 | 1 | 27.115 | 79.974 | .000* |
| Within Groups | 76.286 | 225 | .339 | |||
| Total | 103.401 | 226 | ||||
| Type of job | Between Groups | 30.561 | 1 | 15.280 | 46.990 | .000* |
| Within Groups | 72.840 | 225 | .325 | |||
| Total | 103.401 | 226 | ||||
| LBP episodes | Between Groups | 4.507 | 2 | 2.254 | 5.105 | .000* |
| Within Groups | 98.894 | 224 | .441 | |||
| Total | 103.401 | 226 | ||||
| Seeking health advice | Between Groups | 13.742 | 1 | 13.742 | 34.485 | .000* |
| Within Groups | 89.659 | 225 | .398 | |||
| Total | 103.401 | 226 | ||||
| Interference in daily activities | Between Groups | 19.089 | 1 | 19.089 | 50.943 | .000* |
| Within Groups | 84.311 | 225 | .375 | |||
| Total | 103.401 | 226 |
Table 2: Differences based on Levels of Disability using a One-way Analysis of Variance.
The following variables were associated with the ODI and FABQ (PA & W) scores in the regression model: age, type of job, number of LBP episodes, seeking health advice, and daily activity interference. Table 3 shows the coefficients of the regression analyses. Age was a significant predictor of all the dependent variables. Individuals seeking health advice and those who were homemakers reported higher fear avoidance behaviors than working people did. Finally, age and the type of job were superior in predicting disability and fear avoidance beliefs than number of LBP episodes and interference in daily activities were (Table 3).
| Dependent variable | Predictor | R | R2 | Adjusted R2 | Lower 95% | Upper 95% | P value |
|---|---|---|---|---|---|---|---|
| ODI | Age | 0.24 | 0.05 | 0.05 | -6.21 | -1.91 | 0.00** |
| Job type | 0.34 | 0.11 | 0.11 | 1.91 | 4.08 | 1.22 | |
| LBP episodes | 0.06 | 0.00 | -0.00 | -1.71 | 0.6 | 0.3 | |
| seek health advise | 0.27 | 0.07 | 0.07 | 2.48 | 6.58 | 2.04 | |
| daily activities | 0.10 | 0.01 | 0.00 | -0.35 | 3.24 | 0.11 | |
| FAB(PA) | Age | 0.17 | 0.03 | 0.02 | -4.95 | -0.81 | 0.00** |
| Job type | 0.19 | 0.03 | 0.03 | 0.52 | 2.67 | 0.00** | |
| LBP episodes | 0.03 | 0.00 | -0.00 | -1.41 | 0.82 | 0.6 | |
| seek health advise | 0.14 | 0.02 | 0.01 | 0.29 | 4.31 | 0.02* | |
| daily activities | 0.05 | 0.00 | -0.00 | -0.94 | 2.48 | 0.3 | |
| FAB(W) | Age | 0.12 | 0.01 | 0.01 | -7.14 | 0.04 | 0.05* |
| Job type | 0.22 | 0.05 | 0.04 | 1.37 | 5.05 | 0.00** | |
| LBP episodes | 0.05 | 0.00 | -0.00 | -2.71 | 1.13 | 0.4 | |
| seek health advise | 0.07 | 0.00 | 0.00 | -1.44 | 5.52 | 0.24 | |
| daily activities | 0.03 | 0.00 | -0.00 | -2.14 | 3.76 | 0.58 |
Table 3: Findings of the Regression Analysis for Comparing the Disability and Fear Avoidance Scores to Other Variables.
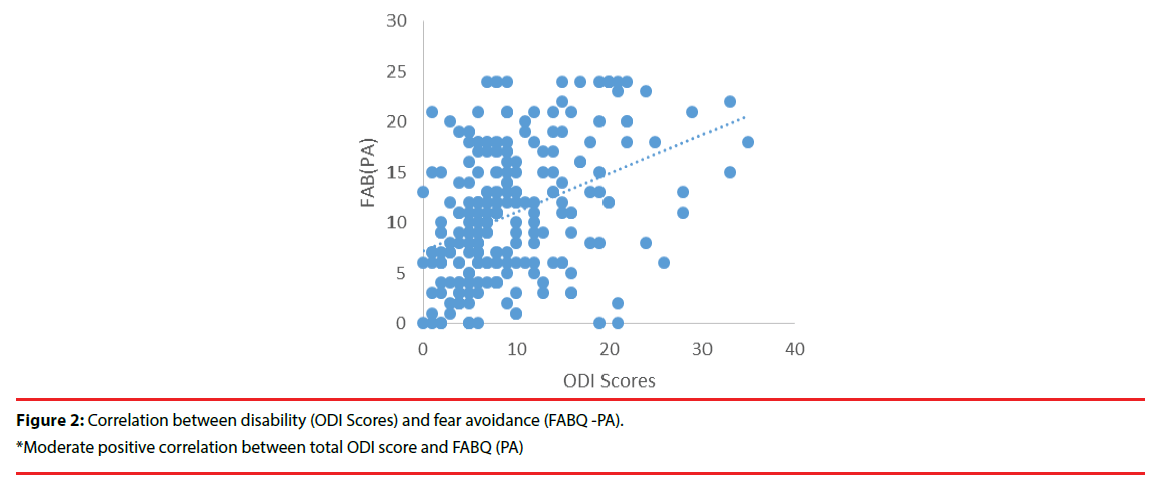
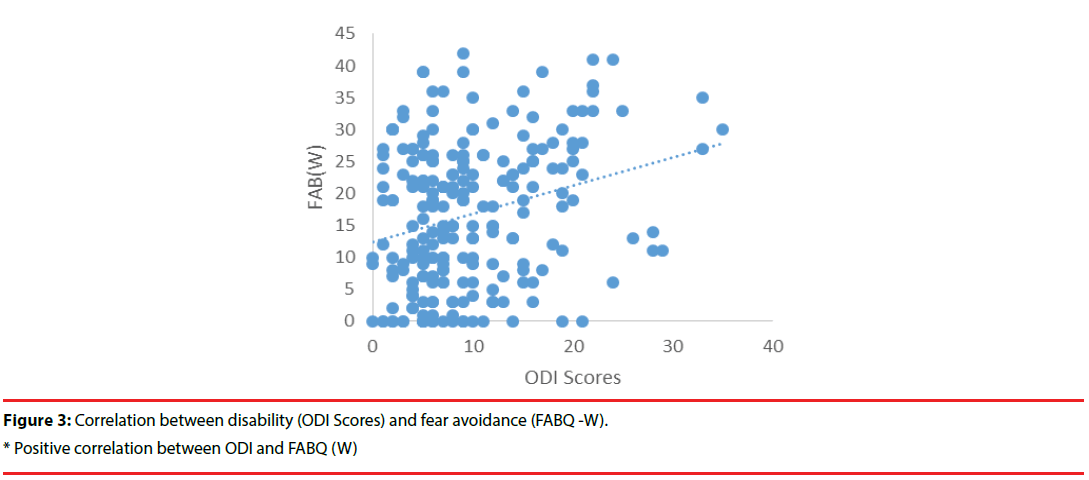
The moderate, severe, and crippled disabilitylevel groups reported significantly greater fear avoidance beliefs about physical activity (FABPA) as compared to the minimal disability group. A correlation analysis was conducted to assess the association between the disability and fear avoidance beliefs. Greater disability (ODI score) was associated with higher levels of fear avoidance beliefs about physical activity (FABQ-PA scores) (r = 0.39, p < .01) and work (FAB-W; r = 0.26, p < .01) (Figures 2 and 3).
Discussion
To our knowledge, this is the first ever study on Saudi females, investigating their health behaviors and beliefs related to disability due to LBP. Our research project elaborated the behaviors and health literacy among women with LBP and this paper was a part of the same project. The current study involved Saudi females who had experienced nonspecific chronic LBP for more than 3 months duration. Previous studies have also involved chronic conditions, but none has exclusively considered that in females [10]. The descriptive analysis on the sample showed the predominance of the minimal disability population. In this study, 67% of the participants experiences minimal disability. The high frequency of minimal disability can be explained by the fact this sample consisted of young female students, workers, and homemakers, as opposed to the studies that included elderly and middle aged workers of both genders [21]. Prevalence of moderate to severe disability increased with age and has been reported in previous studies [3]. In contrast, studies by Briggs et al. (2010) and Denison, Asenlof, and Lindberg (2004) showed that there was no effect of age on the level of disability, and found no significant correlation (r = 0.01) between age and disability due to chronic musculoskeletal pain [15,22].
It has been proposed that confrontation is an adaptive response to pain while avoidance is a maladaptive behavior causing LBP patients to avoid certain daily activities that may cause pain [23]. In the acute phase of LBP, fear avoidance is considered an adaptive response to avoid movements that would cause tissue damage. However, higher levels of fear avoidance beliefs were related to persistent disability and inactivity [24]. It is therefore considered as the most important cognitive factor leading to chronic disability in LBP patients. The results of the present study confirm earlier findings that individuals with moderate to severe disability due to chronic LBP would seek medical care more often as compared to others [4]. Additionally, it was found that chronic LBP was significantly associated with daily activity limitation [25,26]. Measures of disability correlated with the FABQ work and physical activity scores with r-values of 0.39 and 0.26 respectively. A similar degree of responses was observed in earlier studies involving chronic LBP patients [27]. Our results are in good agreement with other studies that reported that there is a positive correlation between fear avoidance beliefs and disability, as patients who have a high level of disability showed increased fearavoidance beliefs [17]. Moreover, another study pointed that the increased experience of LBP can be a consequence of fear-avoidance beliefs [28].
Many influential factors affect persons’ fearavoidance beliefs. Poiraudeau et al. showed that rheumatologists have negative beliefs about back pain, which reflects in their conformity to guidelines on daily activities. Another study by Alshami et al. revealed that Saudi physical therapists’ beliefs about LBP disability are deep and defined, and that they further influenced the patients’ beliefs. Further, Grotle, Vollestad, Veierod, and Brox established the relationship that an increase in the time taken for the conversion of LBP from an acute to a chronic condition led to more profound fear avoidance beliefs [29]. Additionally, Waddell et al. indicated that work loss affects the beliefs of the patients, while age and gender have no effect on their beliefs. Adherence to treatment depends on the self-efficacy beliefs, as individuals with high self-efficacy have better adherence to treatment.
Despite the strengths of our project, there were several limitations. While working on this study, we were bounded by time. Moreover, majority of the participants fell under the minimal disability category. Thereby, the sample was heterogeneous in terms of severity of disability. In addition, the crosssectional design that did not permit the assessment of the temporal relationships among variables, the potential for social acceptability bias of the selfreported data, and the potential for uncontrolled confounding factors were other limitations of the present study.
Conclusion
In conclusion, the present findings confirm that LBP-related disability is associated with avoidance beliefs and suggest that a moderate to severe disability results in the increased use of medical services. In Saudi Arabia, sedentary behavior is more common among females. They have limited opportunities to attend health care clinics. In addition, their dependency on male members and the hot climatic conditions in Saudi Arabia results in high inactivity and low engagement in health promotion behaviors. Considering these behaviors and the level of patients’ disability, physicians and rehabilitation health providers could deliver LBP information and management methods that may enhance patients’ knowledge about their condition. To our knowledge, this is the first study on Saudi females with chronic LBP, and it has important implications for women’s health. Reduction of fear avoidance beliefs would help increase the level of patients’ contribution in daily activities and social life. Future studies on acute LBP are necessary for preventing the transformation of LBP from an acute to a chronic condition.
Acknowledgement
The research project was supported by a grant from the “Research Centre of the Female Scientific and Medical colleges”, Deanship of Scientific research, King Saud University. The authors also thank the Deanship of Scientific research and RSSU at King Saud University for their technical support. We acknowledge our sincere thanks to Ms. Alaa A. Alrayes, Ms. Fai A. AlRadady, Ms. Rima N. Al-Ayed, and Ms. Shahad M. Alrumayh, the students of King Saud University for their contribution in data collection and for participation in the study.
References
- Chou R. Low back pain (chronic). Am. Fam. Physician 84(4), 437-438 (2011).
- Waddell G, Main CJ. A new clinical model of low back pain and disability: The back pain revolution. Edinburgh: Churchill Livingstone (1998).
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet 354(9178), 581-585 (1999).
- Waterman BR, Belmont PJ. Jr, Schoenfeld AJ. Low back pain in the United States: Incidence and risk factors for presentation in the emergency setting. Spine. J 12(1), 63-70 (2012).
- Alshami AM. Prevalence of spinal disorders and their relationships with age and gender. Saudi. Med. J 36(6), 725-730 (2015).
- AL-Arfaj AS, AL-Saleh SS, Alballa SR, et al. How common is back pain in Al-Qaseem region. Saudi. Med. J 24(2), 170-173 (2003).
- AL Faraj S, AL Mutairi K. Vitamin D deficiency and chronic low back pain in Saudi Arabia. Spine 28(2), 177-179 (2003).
- AL Dajah S, AL Daghdi, A. Prevalence and risk factors of low back pain among nurses in Sudayr Region. ESJ 9(33), 198-205 (2013).
- Hasan M Keriri. Prevalence and risk factors of low back pain among nurses in operating rooms, Taif, Saudi Arabia.J. Med. Sci. Res 4(1), 3 (2013).
- Lundberg M, Grimby-Ekman A, Verbunt J, et al. Pain-related fear: A critical review of the related measures. Pain. Res. Treat 1-26 (2011).
- Melzack R. From the gate to the neuromatrix. Pain 82(1), S121-S126 (1999).
- Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 85(3), 317-332 (2000).
- Buer N, Linton SJ. Fear-avoidance beliefs and catastrophizing: Occurrence and risk factor in back pain and ADL in the general population. Pain 99(3), 485-491 (2002).
- Poiraudeau S, Rannou F, Le Henanff A, et al. Outcome of subacute low back pain: Influence of patients' and rheumatologists' characteristics. Rheumatology 45(6), 718-723 (2006).
- Briggs AM, Jordan JE, Buchbinder R, et al. Health literacy and beliefs among a community cohort with and without chronic low back pain. Pain 150(2): 275-283 (2010).
- Waddell G, Newton M, Henderson I, et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 52(2), 157-168 (1993).
- Basler HD, Luckmann J, Wolf U, et al. Fear-avoidance beliefs, physical activity, and disability in elderly individuals with chronic low back pain and healthy controls. The Clin. J. Pain 24(7), 604-610 (2008).
- Vu M, Azmat A, Radejko T, et al. Predictors of delayed healthcare seeking among American Muslim women. J. Womens. Health 25(6), 586-593 (2016).
- Vianin M. Psychometric properties and clinical usefulness of the Oswestry Disability Index. J. Chiropr. Med 7(4), 161-163 (2008).
- Laufer Y, Elheiga-Na'amne BA, Rozen N. Translation and validation of the Arab version of the fear avoidance beliefs questionnaire. J. Back. Musculoskelet. Rehabil 25(3), 201-208 (2012).
- Walsh IA, Oishi J, Coury HJ. Clinical and functional aspects of work-related musculoskeletal disorders among active workers. Rev. Saude. Publica 42(1), 108-116 (2008).
- Denison E, Asenlof P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain 111(3), 245-252 (2004).
- Vlaeyen JW, Seelen HA, Peters M, et al. Fear of movement/ (re)injury and muscular reactivity in chronic low back pain patients: An experimental investigation. Pain 82(3), 297-304 (1999).
- Van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain: A systematic review of randomized controlled trials of the most common interventions. Spine 22(18), 2128-2156 (1997) .
- Blyth FM, March LM, Brnabic AJ, et al. Chronic pain and frequent use of health care. Pain 111(1-2): 51-58 (2004).
- Pereira LS, Sherrington C, Ferreira ML, et al. Self-reported chronic pain is associated with physical performance in older people leaving aged care rehabilitation. Clin. Interv. Aging 9: 259-265 (2014).
- Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: Relationships with current and future disability and work status. Pain 94(1): 7-15 (2001).
- Jensen JN, Albertsen K, Borg V, et al. The predictive effect of fear-avoidance beliefs on low back pain among newly qualified health care workers with and without previous low back pain: a prospective cohort study. BMC. Musculoskelet. Disord 10:117 (2009).
- Grotle M, Vollestad NK, Veierod MB, Brox JI. Fear-avoidance beliefs and distress in relation to disability in acute and chronic low back pain. Pain 112(3), 343-352 (2004).