Review Article - Interventional Cardiology (2011) Volume 3, Issue 4
Femoral vascular access-site complications in the cardiac catheterization laboratory: diagnosis and management
- Corresponding Author:
- Ion S Jovin
Department of Medicine, Virginia Commonwealth University, McGuire VAMC
1201 Broad Rock Boulevard 111J, Richmond, VA 23249, USA
Tel: +1 804 6755419
Fax: +1 804 6755420
E-mail: isjovin@yahoo.com
Abstract
Keywords
arteriovenous fistula, cardiac catheterization, hematoma, pseudoaneurysm, retroperitoneal hemorrhage, vascular access-site complications
Cardiac catheterization and percutaneous intervention can result in vascular access-site complications. It is important for individuals caring for the patient returning from the cardiac catheterization laboratory to be aware of and recognize the various complications that can occur and how they should be treated. This article will focus on the vascular access-site complications via the femoral approach, which can lead to significant morbidity and mortality.
Anatomy & technique
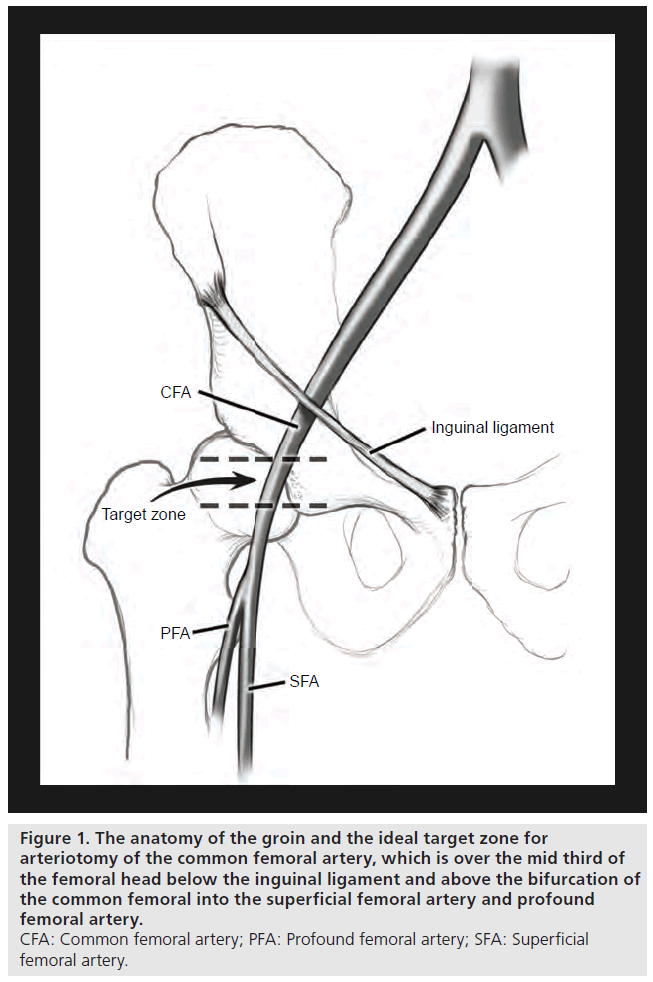
The external iliac artery crosses under the inguinal ligament to become the common femoral artery. The inferior epigastric artery branches off the external iliac artery inferiorly [1]. The common femoral artery bifurcates below the inguinal ligament into the superficial and profunda arteries. The common femoral artery is housed in the femoral triangle and has the benefit of being a large superficial vessel that can be compressed against the femoral head to achieve hemostasis [2]. Three key landmarks have traditionally been used in obtaining femoral access: the inguinal crease, the maximal pulsation of the femoral artery and bony landmarks (such as a line drawn from the anterior superior iliac crest to the pubic symphysis) [3]. The femoral artery can be cannulated at the base of the femoral triangle, just inferior to the inguinal ligament but above the bifurcation of the femoral artery [4,5]. This location corresponds to 2–3 cm below the mid-point of the pubic symphysis and the anterior superior iliac crest [6]. Because the inguinal skin crease is located below the femoral artery bifurcation in over 70% of patients, using it as a landmark for cannulation can lead to low femoral puncture [3,6]. Garrett et al. found that the femoral artery bifurcation was below the inguinal ligament and the middle of the femoral head in nearly all patients studied. The bifurcation of the common femoral artery was below the middle of the femoral head in 99% of cases [7]. Fluoroscopy is helpful in locating the position of the femoral head and therefore aids in more accurately guiding femoral puncture. Using the location of maximal femoral pulsation has been shown to ensure more consistent puncture of the common femoral artery as the maximal femoral pulse was found over the femoral artery in 93% of cases [6,8]. The goal of femoral puncture is to access the femoral artery where the artery overlies the middle third of the femoral head as depicted in Figure 1 [9].
Figure 1: The anatomy of the groin and the ideal target zone for
arteriotomy of the common femoral artery, which is over the mid third of
the femoral head below the inguinal ligament and above the bifurcation of
the common femoral into the superficial femoral artery and profound
femoral artery.
CFA: Common femoral artery; PFA: Profound femoral artery; SFA: Superficial
femoral artery.
Definitions
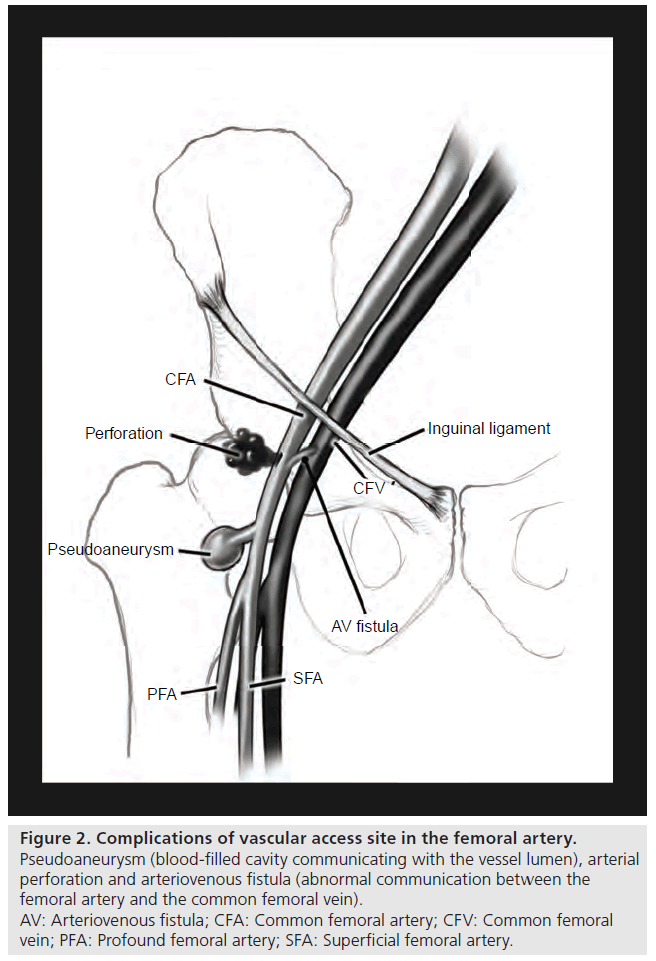
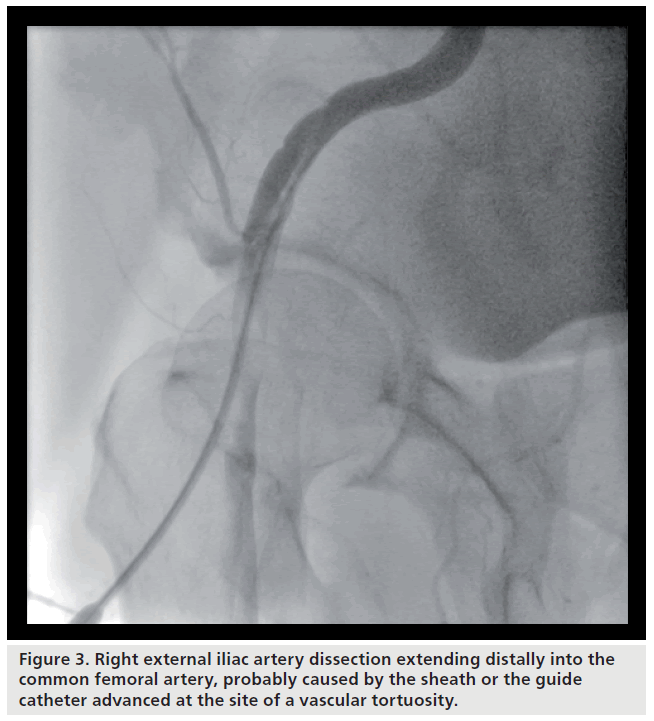
Vascular complications of cardiac catheterization and coronary intervention can be divided into minor and major complications. Minor complications include minor bleeding, ecchymosis and stable hematoma. Major complications include pseudoaneurysm, arteriovenous (AV) fistula, hematoma requiring transfusion, retroperitoneal hemorrhage, arterial dissection, embolism, thrombosis, infection, vessel rupture/perforation and limb ischemia. An illustration of a pseudoaneurysm and AV fistula can be seen in Figure 2. Bleeding is the most common complication of the transfemoral approach to catheterization and can manifest as a stable or unstable hematoma, uncontrolled bleeding, pseudoaneurysm or retroperitoneal hemorrhage. Hematomas can expand in 10–15% of patients and can manifest as hemorrhagic shock [10]. A retroperitoneal hemorrhage is a potential life threatening complication of femoral artery puncture that should be suspected in any postcatheterization patient who develops hypotension, ipsilateral flank, abdominal or back pain, or a drop in hemoglobin without a source. A pseudoaneurysm (false aneurysm) is a communication between the femoral artery and the overlying fibromuscular tissue resulting in a blood-filled cavity [11]. It is formed when blood escapes from the lumen of an artery through a defect in one or more layers of the arterial wall and forms a pocket beneath the adventitia of the artery or in the surrounding tissue near the site of arterial puncture. A pseudoaneurysm has continuity with the arterial lumen whereas a hematoma does not [10,12]. Pseudoaneurysms frequently result from failure to achieve adequate hemostasis after the catheter or sheath is removed [12]. An AV fistula is an abnormal connection between a vein and artery that is generally asymptomatic. It is more likely to result from arterial puncture below the femoral artery bifurcation and is typically created between the superficial or deep femoral artery and the adjacent lateral circumflex vein [10]. Dissection can occur in the femoral or iliac artery, but is most common in the iliac arteries due to atherosclerosis and tortuosity in these vessels [10]. Figure 3 shows an external iliac artery dissection caused by the vascular sheath. Embolic complications after catheterization are uncommon, but can lead to emboli lodging into small vessels and causing tissue ischemia [10]. Local thrombosis leading to limb ischemia is rare [9].
Figure 2: Complications of vascular access site in the femoral artery.
Pseudoaneurysm (blood-filled cavity communicating with the vessel lumen), arterial
perforation and arteriovenous fistula (abnormal communication between the
femoral artery and the common femoral vein).
AV: Arteriovenous fistula; CFA: Common femoral artery; CFV: Common femoral
vein; PFA: Profound femoral artery; SFA: Superficial femoral artery.
Incidence
The incidence of vascular access-site complications following catheterizations varies and in general depends on the study population. Femoral access-site complications are generally higher for interventional procedures than diagnostic procedures, which is likely related to anticoagulant therapy and sheath diameter. Femoral accesssite complications have been reported to range from 0 to 17% in patients undergoing diagnostic and interventional cardiovascular procedures [2]. Chandrasekar et al. reported that femoral access-site complications were 1.8% for diagnostic and 4% for interventional procedures [13]. The incidence of major bleeding complications ranges from 2 to 6% after percutaneous coronary angioplasty [10]. Access-site injury rates requiring procedural or surgical intervention or bleeding requiring transfusion range from 2.6 to 6.6% [14]. Rates for major bleeding (bleeding requiring transfusion of more than two units of blood) in trials of glycoprotein (GP) IIb/IIIa inhibitors ranged from 1.9 to 14% [14]. Tsetis et al. reported that a significant hematoma or uncontrollable bleeding requiring transfusion or invasive procedure occurs in <1% of catheterizations [15]. Yatskar et al. found that a hematoma is the most frequent periprocedural complication and can occur in anywhere from 2 to 12% of cases [16]. The incidence of pseudoaneurysm ranges from 0.5 to 6.3% and many sources site an approximate incidence of 1% [17–22]. Samal et al. cites that femoral pseudoaneurysms can occur in 0.1–1.5% of diagnostic angiography and in up to 7.7% of interventional procedures [10]. The incidence of AV fistulas has been reported to be 0.2–2.1% [17–22]. Retroperitoneal hemorrhage has an incidence from 0.15 to 0.5% [11,23–25]. Trimarchi et al. studied 112,340 patients undergoing percutaneous coronary intervention (PCI) and found the incidence of retroperitoneal hemorrhage to be 0.4% [26]. Arterial dissection occurs in 0.01–0.4% of procedures [9]. Arterial thrombosis can occur in <0.5% of cases [15,21]. Risks of vascular accesssite complications have changed with the advent of arterial closure devices and additional possible complications with these devices include the risk of infection, stenosis and embolism [10].
Risk factors
Risk factors for vascular complications of cardiac catheterization can be divided into patientrelated and procedure-related factors. Patientrelated risk factors include female gender, low body weight, obesity, lower body surface area, older age, peripheral vascular disease, renal failure or elevated creatinine, and low platelet count [2,9,14]. Some studies report conflicting results on other associations with vascular complications, such as myocardial infarction, cardiogenic shock, diabetes mellitus and hypertension [14]. Procedural-related factors include previous catheterization at the same site, high doses and longer duration of anticoagulation, use of thrombolytic agents, use of GP IIb/IIIa inhibitors (particularly abciximab), larger arterial sheaths, concomitant venous sheaths, prolonged indwelling sheath duration, prolonged procedure duration, repeat PCI and location of the arterial puncture [2,9,14,27]. Sherev et al. found that 71% of all vascular access-site complications were due to low or high femoral artery puncture sites [2]. Fewer femoral complications have been noted in patients undergoing elective PCI using 6 F compared with 7- or 8-F guiding catheters [9].
Independent predictors of hematomas requiring blood transfusions include smaller patients, older age, female gender, chronic renal insufficiency, complex coronary lesions, patients with acute myocardial infarction or cardiogenic shock presenting for an emergent procedure, use of GP IIb/IIIa inhibitors and the use of thrombolytics [16]. There is a higher risk of the formation of a pseudoaneurysm with interventional procedures than diagnostic procedures because of the length of the procedure, larger devices (and size of puncture) and more aggressive anticoagulation [28]. Low arterial access, female gender, older age, diabetes and obesity have been associated with pseudoaneurysm formation [9]. Risk of bleeding into the retroperitoneal space is increased with a high femoral puncture (particularly above the inguinal ligament and puncturing the back wall of the vessel) and postcatheterization anticoagulation [3,9,23]. Sherev et al. found that arterial puncture above the most inferior border of the inferior epigastric artery in patients undergoing PCI was associated with 100% of all retroperitoneal hemorrhages [2]. It is more difficult to compress the artery against the femoral head when the arterial puncture site is below the bifurcation because the pressure is applied primarily against soft tissue rather than the bone of the femoral head in this situation [2,6]. Above the inguinal ligament, the artery resides in the retroperitoneal space making compression and hemostasis difficult. Female sex and preprocedural GP IIb/IIIa inhibitors had an odds ratio over 2 for being independent predictors of retroperitoneal hemorrhage. The use of bivalirudin was associated with a lower risk of the development of a retroperitoneal hemorrhage [26]. A high or low femoral arterial puncture, multiple puncture attempts and prolonged clotting times can increase the risk of AV fistula formation. The risk factors for lower extremity ischemia include the use of larger catheters or sheaths in relatively smaller arteries, peripheral vascular disease, older age, cardiomyopathy, hypercoagulable states and vessel dissection [9].
Prevention
There are several approaches in preventing vascular access-site complications. The radial artery has been investigated as an alternate route for cardiac catheterization. Fluoroscopic guidance has been proposed to allow for better visualization of anatomic landmarks. Advances in anticoagulant and antiplatelet agents offer reduction in bleeding complications. Arterial closure devices have been developed and are currently being studied to determine their efficacy in reducing vascular access-site complications.
▪ Choice of access site
Alternative vascular access sites, such as the radial, brachial and axillary artery have been investigated. Complications associated with brachial artery access are similar to those seen with femoral access, but ischemic complications are generally more common with brachial access [10]. Radial access has been associated with lower complication rates (as low as <0.7%), improved patient comfort and reduced hospital costs [6,29]. Disadvantages of radial access include a higher incidence of procedure failure that necessitates resorting to the femoral approach, longer procedural times (at least in the ‘learning curve’ phase), postprocedural radial artery spasm and occlusion [29].
Radial access has been shown to significantly reduce bleeding complications. The PRESTOACS study revealed that the radial approach was associated with a significant decrease in bleeding and a nonsignificant decrease in the net clinical outcome during hospitalization compared with the femoral approach [30]. The radial approach has been found to have a decrease on death or reinfarction rates, bleeding and net clinical outcome at 1-year follow-up compared with the femoral approach. This was true despite more intense procedural use of antiplatelet therapy in patients undergoing the radial approach. The RIVAL trial investigated whether radial access was superior to femoral access in patients undergoing angiography [31]. Large hematomas and pseudoaneurysms requiring closure occurred more frequently with femoral access than radial access. Procedure time, length of hospital stay, pain at the access site and PCI contrast volume were similar in both routes, but fluoroscopy time was longer for radial access by 1.8 min. Patients were nine times more likely to prefer the radial approach for catheterization compared with the femoral approach if they were to have another procedure. There was no difference in death, myocardial infarction, stroke or noncoronary artery bypass graft-related major bleeding in the two groups.
The rate of bleeding complications requiring transfusions for radial access is 0.15% [32]. Pseudoaneurysm and AV fistula are even more uncommon with the radial approach compared with the femoral approach [33]. Radial artery occlusion is more common than femoral artery occlusion because of the smaller artery to sheath ratio and prolonged high pressure compression. Pancholy et al. found the incidence of radial artery occlusion to be 9% [34] but in the newer series (and with the use of patent hemostasis) the incidence is closer to 3%. The decision to use the radial approach must be balanced by weighing the advantages and disadvantages. Radial access may be associated with fewer hematomas, pseudoaneurysms and AV fistulas, but it carries its own risk of arterial occlusion and arterial spasm. It is preferred by patients, costs less, may be associated with shorter hospital stays and has similar (if not better) outcomes as compared with femoral access. However, operators may not be as experienced with this route leading to longer procedures. The radial approach is a promising technique that can significantly reduce the incidence of access complications and, as its use will be more widely adopted, more long-term results will become available.
▪ Fluoroscopy of the femoral head
Determining the ideal site of femoral artery cannulation with fluoroscopy can reduce a number of vascular access-site complications. Fluoroscopy can be used to identify the location of the medial border of the femoral head, which is the most reliable landmark for the common femoral artery [6]. Jacobi et al. found that the use of fluoroscopy resulted in more ideal arterial sheath placement, particularly in obese patients, but did not dramatically reduce complication rates [35]. Abu-Fadel et al. showed that fluoroscopy decreased the number of low arteriotomies, but did not decrease the number of arterial punctures or complications rates. This study did show benefit in the use of fluoroscopy in obese and in female patients [36]. Fitts et al. aimed to reduce vascular accesssite complications in patients undergoing PCI and found that the use of fluoroscopy was associated with a significantly lower incidence of pseudoaneurysms and arterial injury, but found no significant difference in the incidence of bleeding complications [37]. Fluoroscopy is quick and appears to result in more successful arteriotomies while only adding a minimal amount of radiation. The routine use of fluoroscopy could be beneficial in most patients undergoing catheterization and in our experience fluoroscopy of the femoral head especially prevents the sticks above the inguinal ligament, which are most often associated with retroperitoneal bleeds.
▪ Ultrasound guidance
The FAUST trial studied procedural and clinical outcomes of femoral arterial access using ultrasound guidance compared with standard fluoroscopic guidance. In general, ultrasound guidance reduced the number of attempts, time to access, risk of accidental venipuncture and vascular complications (i.e., fewer hematomas) when obtaining femoral arterial access. However, the study found that ultrasound guidance improved cannulation rates only in patients who had a high common femoral artery bifurcation compared with standard fluoroscopic guidance [38].
▪ Type of anticoagulant & antiplatelet agents used
Vascular access-site complications are associated with the use of anticoagulant and antiplatelet agents. The use of GP IIb/IIIa inhibitors, particularly abciximab, has been shown to increase vascular access-site complications [39,40]. The combination of abciximab and unfractionated heparin was associated with an increased risk of bleeding in the EPIC trial [41]. The combination of abciximab and low-dose weight-adjusted heparin conferred substantial clinical benefit without increased bleeding complications in the EPILOG trial [42]. The reversal of abciximab’s antiplatelet action is slow. On the contrary, eptifibatide and tirofiban selectively bind to the GP IIb/IIIa receptor and their effect on platelets is rapidly reversed when discontinued. If bleeding occurs, the effects of eptifibatide and tirofiban can be reversed with platelet transfusion [43].
Bivalirudin binds specifically and reversibly to both fibrin bound and unbound thrombin [44]. In the REPLACE-2 trial, bivalirudin with selective GP IIb/IIIa inhibition provided similar protection from periprocedural ischemia and was associated with less major bleeding compared with low-dose heparin plus GP IIb/IIIa inhibition [24]. Bivalirudin was associated with similar rates of bleeding and ischemia as heparin in patients with moderate or high-risk acute coronary syndromes who were undergoing intervention with GP IIb/ IIIa inhibitors. Bivalirudin alone was associated with significantly lower rates of bleeding and similar rates of ischemia [45]. Compared with heparin plus GP IIb/IIIa inhibition, bivalirudin alone resulted in significantly reduced 30-day rates of major bleeding and major adverse cardiovascular events in patients with ST-segment elevation myocardial infarctions undergoing primary PCI [46]. This was true despite the significantly higher peak activated coagulation time among patients treated with bivalirudin.
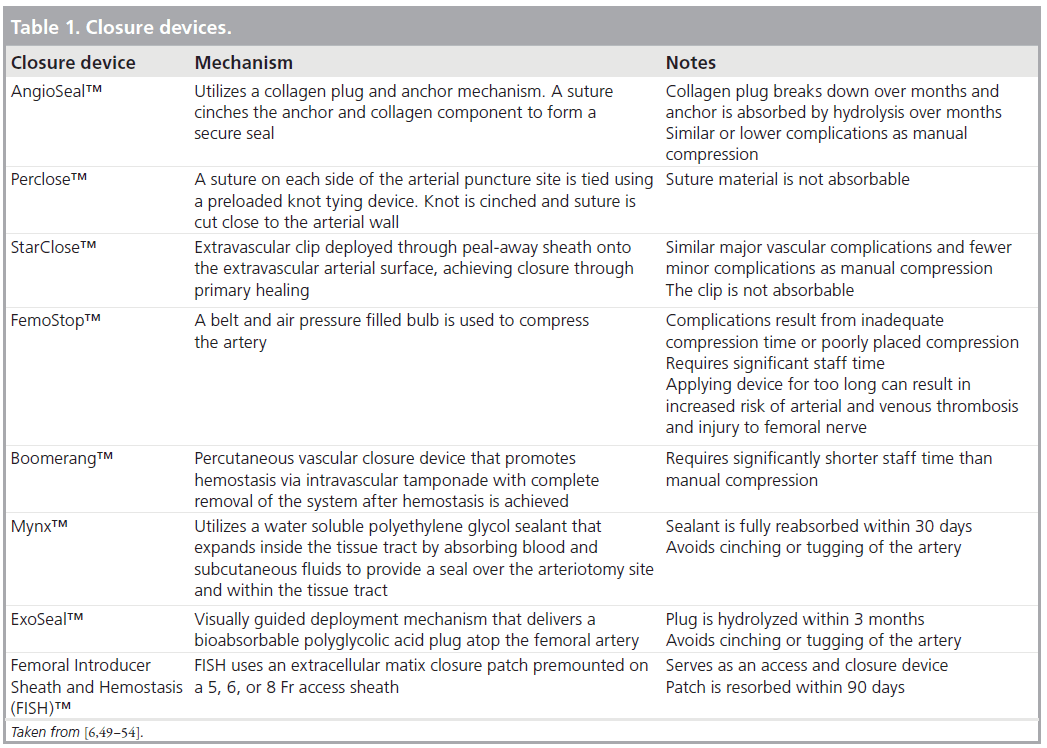
▪ Arterial closure devices
Arterial closure devices were initially designed as active closure methods. The two main types of active arterial closure devices are collagen plug closure devices (e.g., AngioSeal™; St. Jude Medical) and suture-mediated closing devices (e.g., Perclose™; Abbott Vascular) [10,47]. StarClose™ (Abbott Vascular) is a newer active closure method involving surgical staple/ clip technology. Passive closure devices focus on enhanced manual compression utilizing assisted compression with mechanical clamps (e.g., FemoStop™; St. Jude Medical), external patches or plugs (e.g., the Mynx™ Vascular Closure Device [AccessClosure] and the ExoSeal™ device [Cordis]) and wire-stimulated track thrombosis (e.g., the Boomerang™ Catalyst Wire; Cardiva Medical). Some of these devices have the disadvantage of not inducing immediate hemostasis [48]. An overview of closure devices and their main features is provided in Table 1 [6,49–54].
Some of the complications that arise from the use of arterial closure devices are similar to complications with manual compression: bleeding (from incomplete closure), hematoma, pseudoaneurysm (from a persisting arterial leak) and AV fistulas. Other complications include thrombus formation, embolization of the collagen plug or clip, late stenosis of the artery (which can lead to limb ischemia), compression of the femoral vein access site infections, septic emboli, femoral endarteritis and limb ischemia [6,10,55]. Infectious complication rates with closure devices have been observed to be anywhere from 0.0 to 5.1%, with Staphylococcus aureus being the most common infectious agent followed by coagulasenegative Staphylococcus [55]. The foreign material in the intravascular space and arterial wall may serve as a nidus for infection. The median time from arterial closure device usage to site infection is 8 days. Mycotic pseudoaneurysm is the most common complication of infection from arterial closure devices.
Arterial closure devices are generally safe and allow for earlier mobility, improved patient comfort, earlier discharge, potentially reduced healthcare costs and arguably reduced groin complications (particularly hematomas and pseudoaneurysms). They are effective in small arteries and vessels affected by connective tissue disorders [6,15]. Earlier experience with arterial closure devices revealed higher vascular complication rates than with manual compression [56]. A meta-analysis conducted by Koreny et al. in 2004 found that time to hemostasis was shorter with arterial closure devices, but they potentially conferred a higher risk of hematoma and pseudoaneurysm formation [57]. Another meta-analysis in 2004 conducted by Nikolsky et al. showed that vascular complications were similar with AngioSeal, Perclose, and VasoSeal™ (Datascope Corporation) compared with mechanical compression for diagnostic cardiac catheterization; vascular complications with AngioSeal and Perclose were similar to mechanical compression for PCI, but complication rates were higher with VasoSeal compared with mechanical compression [58]. Arora et al. found that arterial closure devices reduced the risk of vascular complications compared with manual compression in patients undergoing both diagnostic angiography and PCI [59]. Newer generations of vascular closure devices and more operator experience are likely reducing the vascular complication rates and may be reducing cost. One study found that the routine use of AngioSeal was associated with a lower cost per PCI procedure compared with manual compression [60]. A study comparing AngioSeal to Mynx found that the rates of major vascular complications were not significantly different between the two devices, but Mynx was associated with a higher rate of device failure [61]. The main advantage of vascular closure devices used after diagnostic coronary angiography is shortening the time to ambulation. This may become less relevant as more procedures are performed using the radial access route. After PCI, where the patient is at much higher risk of bleeding, there may be some advantage with the use of closure devices, although transradial PCI may change this paradigm as well.
Diagnosis
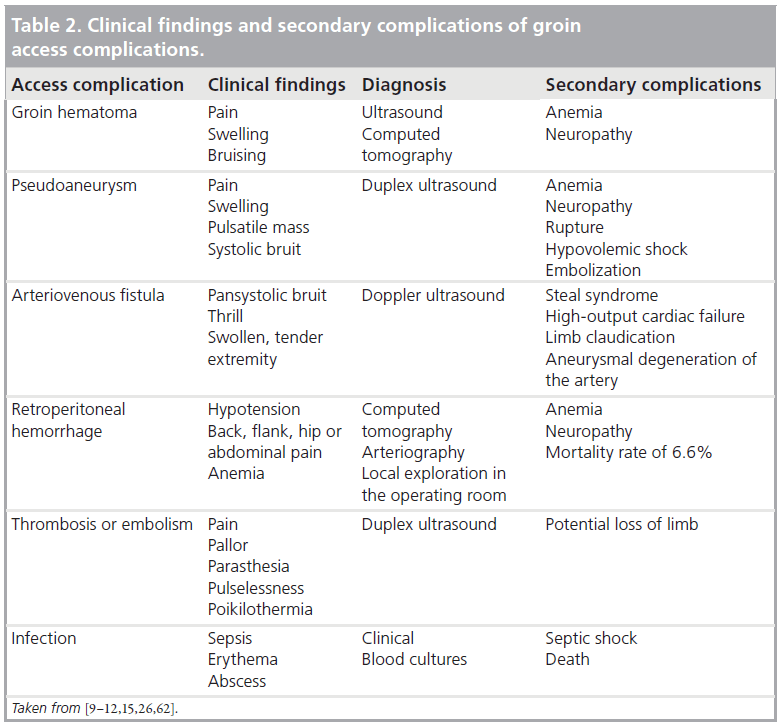
The diagnosis of the various vascular complications is based on history and physical examination findings and can typically be confirmed by imaging. Ultrasound is usually the initial imaging procedure in the evaluation of patients with suspected minor vascular access-site complications as it can accurately and reliably diagnose AV fistulas and pseudoaneurysms [61]. Femoral angiography performed during catheterization can assist in identifying complications and some operators advocate performing a femoral angiogram for every case. An overview of the clinical findings and secondary complications of groin access complications is presented in Table 2 [9–12,15,62].
Treatment of vascular access-site complications
Hematomas can progress to shock in some cases. If a hematoma develops ensued by hypotension during catheterization, the femoral artery may have been nicked. A larger sheath size should be utilized and if this is not successful, then manual pressure should be applied. Anticoagulation should be stopped and reversed and hypotension should be managed with fluids and blood products as needed. If bleeding cannot be controlled with manual compression, the bleeding site can be localized with angiography with a sheath inserted in the contralateral femoral artery and potentially tamponaded with balloon inflation [10].
Small pseudoaneurysms, less than 3 cm, can typically be observed as they can clot spontaneously over time (within 4 weeks). Ultrasoundguided compression can compress the site of communication between the pseudoaneurysm and the native artery and allow thrombosis of the aneurysmal sac. A FemoStop device can also be used to compress a pseudoaneurysm. Ultrasoundguided percutaneous thrombin injection into the pseudoaneurysm can cause thrombosis of the pseudoaneurysm within a few seconds after the injection. However, this method has the risk of thrombosis of the native artery and in some cases the femoral vein. Thrombin injection appears to be more effective than ultrasound-guided compression for femoral pseudoaneurysms. Other methods that have been investigated include paraaneurysmal saline where saline is injected into the communication between the false aneurysm and the native artery resulting in elimination of blood flow. Endovascular techniques such as coil embolization, detachable balloons and stent-grafts have also been used to treat femoral pseudoaneurysms. Surgery is the gold standard treatment for pseudoaneurysms requiring treatment. Indications for surgical treatment include rapid expansion of the pseudoaneurysm, concomitant distal ischemia or neurological deficit, mycotic pseudoaneurysm, failure of percutaneous intervention and compromised soft tissue viability. Surgical options include simply suturing the defect after hematoma evacuation or by patch angioplasty where surgical repair is achieved by using a patch [11,12,28,63,64].
Retroperitoneal hemorrhages can typically be treated conservatively with fluid administration, blood transfusions, and discontinuation and reversal of antiplatelet and anticoagulant agents. This is typically sufficient in many patients as accumulated blood will tamponade the site of bleeding. Ongoing active bleeding should prompt immediate vascular surgery consultation. Endovascular methods are available for treating the bleeding. The main endovascular method is balloon tamponade [65]. Other endovascular methods include selective intra-arterial embolization or stent-grafting. Embolization can use a combination of agents including coils, gelatin, and polyvinyl alcohol, and these agents should be placed proximal and distal to the site of bleeding [11]. One proposed indication for embolization was based on hemodynamic instability and degree of blood loss (requiring four or more units of blood within a 24-h period or six or more units within a 48-h period) [66]. Surgical intervention is indicated for unstable patients not responding to fluid and blood product administration if interventional radiology is not successful or available, or for the development of abdominal compartment syndrome due to a large retroperitoneal hemorrhage, or for femoral neuropathy [11,66]. In one study, 16% of patients who developed a retroperitoneal hemorrhage required surgical intervention [67].
AV fistulas can be treated conservatively by monitoring in most patients. They are generally small, not hemodynamically significant and close spontaneously. When AV fistulas become symptomatic, they require closure to prevent increased shunting and distal swelling and tenderness. Options include prolonged bandaging, ultrasound-guided compression, percutaneous implantation of covered stents, percutaneous coil embolization and surgical repair. In many cases, the fistula may be too short or long to be compressed effectively by ultrasound. Surgical intervention is generally reserved for patients who fail a less invasive approach [9,11,15].
If patients develop lower extremity ischemia, angiography should be obtained to characterize the anatomic basis of ischemia. Blood flow can be restored by balloon angioplasty with or without thrombolytic therapy, stents or catheter thrombectomy. Surgical thrombectomy and repair may be required if percutaneous methods are not successful [9]. When arterial dissection is identified, angiography should be obtained to characterize the extent of dissection. Removal of catheters and wires could potentially allow spontaneous resolution of the dissection when identified. If catheter removal is unsuccessful, treatment options include balloon angioplasty, endovascular stent placement or surgical repair to stabilize a flow limiting dissection [9,10]. Treatment of arterial thrombosis consists of thrombectomy performed either percutaneously or surgically. Thrombolytic therapy with tissue plasminogen activator can be considered if a large thrombus burden persists after thrombectomy [15].
Clinical consequences of vascular access-site complications
Bleeding complications during cardiac catheterization have been found to result in longer hospital stays, additional treatments and higher healthcare costs. Yatskar et al. found that patients undergoing PCI who developed hematomas requiring transfusion had a fivefold increase in in-hospital death and a fourfold increase in 1‑year mortality [16]. Kinnaird et al. studied patients between 1991 and 2000 and found that major and minor bleeding complications were associated with an increase in in-hospital death and major adverse cardiac events [68]. Blood transfusions were an independent predictor of in-hospital and 1-year mortality. Patients with major bleeding complications had an average hospital stay of 8.9 days compared with 3.1 days for those without any bleeding complications. Patients undergoing PCI from 1992 to 2003 who developed a retroperitoneal hemorrhage had a higher rate of transfusion, increased length of hospital stay and higher mortality rate [1]; this may be due to the different anticoagulation regimen used at that time. Bleeding is a complication with economic implications as well: the increase in cost was found to range from US$6022 to US$11,767 for each bleeding event [69]. Major vascular access-site complications can lead to the discontinuation of dual antiplatelet therapy in patients who have had recent PCI. Discontinuation of antiplatelet therapy in patients with minor vascular access-site complications is not always necessary and can result in other complications such as recurrent ischemia, myocardial infarction and stent thrombosis [69].
Other vascular access-site complications
Infections and neurologic complications can also occur. The frequency of such complications is not well defined, perhaps because they are rarely observed. Infectious complications include local abscess or cellulitis and sepsis. Less than 1% of patients develop local infection at the site of femoral arterial access and the most common organisms isolated are Staphylococcus aureus and Staphylococcus epidermidis. Neurologic complications include femoral neuropathy, foot drop, paresthesia and chronic pain. Femoral neuropathy occurs in approximately 0.2% of patients. It is typically seen in association with a large hematoma or pseudoaneurysm, which causes pressure on the femoral nerve. When caused by a hematoma or pseudoaneurysm, pressure is exerted on the femoral cutaneous nerve resulting in a sensory neuropathy; this tends to resolve when the pressure is relieved. When caused by retroperitoneal bleeding, pressure is exerted on the femoral nerve resulting in weakness in the upper leg and pain in the thigh and calf; this may not be entirely reversible [4].
Conclusion
Vascular access-site complications continue to pose a significant challenge for invasive and interventional cardiologists. The preventive measures discussed earlier offer promise for reduction of such complications and improvement in patient outcomes.
Future perspective
Fortunately, the incidence of bleeding complications appears to be decreasing. The incidence of major bleeding complications after PCI at the Mayo Clinic decreased from 8.4% in 1994– 1995 to 3.5% in 2000–2005 [55]. This decrease is likely due to a decrease in the mean sheath size (from 8.2-F to 6.4-F), decreased use of a venous sheath (13% to 6%), decreased intensity of anticoagulation with heparin as assessed by peak activated coagulation time (405 s to 312 s), decreased use of postprocedure heparin (80% to 27%) and a decrease in procedure time (1.7 h to 1.4 h) [69]. This decrease in major bleeding complications was found despite the increased use of GP IIb/IIIa inhibitors and procedures performed on older patients. Advancements in anticoagulant and antiplatelet agents and newer generations of arterial closure devices offer some promise in decreasing vascular access-site complications. Alternative access sites, particularly the radial approach, are gaining favor and could result in further decreases in complication rates.
Acknowledgement
The authors want to thank Mary Beatty-Brooks for her help with the illustrations.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪ Vascular access-site complications of cardiac catheterization range from minor complications such as stable hematomas and pseudoaneurysms to major conditions including arteriovenous fistulas, hematomas requiring transfusion, retroperitoneal hemorrhage, arterial dissection, embolism, thrombosis, infection, vessel rupture and limb ischemia.
▪ The incidence of vascular access-site complications is generally higher for interventional procedures than for diagnostic procedures.
▪ Risk factors for vascular complications of cardiac catheterization can be divided into patient-related and procedural-related risk factors.
▪ Catheterizations performed using radial access have been associated with lower complication rates, improved patient comfort and reduced hospital costs.
▪ Routine fluoroscopy may result in better arterial sheath placement and may lower access-site complications.
▪ Vascular access-site complications are associated with the use of anticoagulant and antiplatelet agents. Bivalirudin appears to be associated with fewer bleeding complications.
▪ Newer generations of arterial closure devices have been shown to reduce vascular access-site complications.
▪ Diagnosis of the vascular access-site complications can typically be confirmed by ultrasound. Treatment is dependent upon the complication identified.
▪ Vascular access-site complications result in longer hospital stays, additional treatments and higher healthcare costs.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Ellis SG, Bhatt D, Kapadia S, Lee D, Yen M, Whitlow PL. Correlates and outcomes of retroperitoneal hemorrhage complicating percutaneous coronary intervention. Catheter Cardiovasc. Interv. 67(4), 541–545 (2006).
- Sherev DA, Shaw RE, Brent BN. Angiographic predictors of femoral access site complications: implication for planned percutaneous coronary intervention. Catheter Cardiovasc. Interv. 65(2), 196–202 (2005).
- Turi ZG. Optimal femoral access prevents complications. Cardiac Interventions Today 35–38 (2008).
- Davis C, VanRiper S, Longstreet J, Moscucci M. Vascular complications of coronary interventions. Heart Lung 26(2), 118–127 (1997).
- Moore KL, Dalley AF. Clinically Oriented Anatomy. 4th Edition. Lippincott Williams & Wilkins, Baltimore, MD, USA, 541–545 (1999).
- Cox N. Managing the femoral artery in coronary angiography. Heart Lung Circ. 17, S65–S69 (2008).
- Garrett PD, Eckart RE, Bauch TD, Thompson CM, Stajduhar KC. Fluoroscopic localization of the femoral head as a landmark for common femoral artery cannulation. Catheter Cardiovasc. Interv. 65(2), 205–207 (2005).
- Grier D, Hartnell G. Percutaneous femoral artery puncture: practice and anatomy. Br. J. Radiol. 65(752), 602–604 (1990).
- Wiley JM, White CJ, Uretsky BF. Noncoronary complications of coronary intervention. Catheter Cardiovasc. Interv. 57(2), 257–265 (2002).
- Samal AK, White CJ. Percutaneous management of access site complications. Catheter Cardiovasc. Interv. 57(1), 12–23 (2002).
- Levine GN, Kern MJ, Berger PB et al. Management of patients undergoing percutaneous coronary revascularization. Ann. Intern. Med. 139(2), 123–136 (2003).
- Tisi PV, Callam MJ. Treatment for femoral pseudoaneurysms (review). Cochrane Database Syst. Rev. 2 (2009).
- Chandrasekar B, Doucet S, Bilodeau L et al. Complications of cardiac catheterization in the current era: a single-center experience. Catheter Cardiovasc. Interv. 52(3), 289–295 (2001).
- Piper WD, Malenka DJ, Ryan TJ Jr et al. Predicting vascular complications in percutaneous coronary interventions. Am. Heart J. 145(6), 1022–1029 (2003).
- Tsetis D. Endovascular treatment of complications of femoral arterial access. Cardiovasc. Intervent. Radiol. 33(3), 457–468 (2010).
- Yatskar L, Selzer F, Feit F et al. Access site hematoma requiring blood transfusion predicts mortality in patients undergoing percutaneous coronary intervention: Data from the National Heart, Lung, and Blood Institute Dynamic Registry. Catheter Cardiovasc. Interv. 69(7), 961–966 (2007).
- Popma JJ, Satler LF, Pichard AD et al. Vascular complications after balloon and new device angioplasty. Circulation 88(1), 1569–1578 (1993).
- Johnson LW, Esente P, Giambartolomei A et al. Peripheral vascular complications of coronary angioplasty by the femoral and brachial techniques. Cathet. Cardiovasc. Diagn. 31(3). 165–172 (1994).
- Wyman RM, Safian RD, Portway V et al. Current complications of diagnostic and therapeutic cardiac catheterization. J. Am. Coll. Cardiol. 12(6), 1400–1406 (1988).
- Kresowik TF, Khoury MD, Miller BV et al. A prospective study of the incidence and natural history of femoral vascular complications after percutaneous transluminal coronary angioplasty. J. Vasc. Surg. 13(2). 328–333 (1991).
- Oweida SW, Roubin GS, Smith RB 3rd, Salam AA. Postcatheterization vascular complications associated with percutaneous transluminal coronary angioplasty. J. Vasc. Surg. 12(3), 310–315 (1990).
- Skillman JJ, Kim D, Baim DS. Vascular complications of percutaneous femoral cardiac interventions. Incidence and operative repair. Arch. Surg. 123(10), 1207–1212 (1988).
- Sreeram S, Lumsden AB, Miller JS, Salam AA, Dodson TF, Smith RB. Retroperitoneal hematoma following femoral arterial catheterization: a serious and often fatal complication. Am. Surg. 59(2), 94–98 (1993).
- Lincoff AM, Bittl JA, Harrington RA et al. Bivalirudin and provisional glycoprotein IIb/ IIIa blockade compared with heparin and planned glycoprotein IIb/IIIa blockade during percutaneous coronary intervention: REPLACE-2 randomized trial. JAMA 289(7), 853–863 (2003).
- Kent KC, Moscucci M, Mansour KA et al. Retroperitoneal hematoma after cardiac catheterization: prevalence, risk, and optimal management. J. Vasc. Surg. 20(6), 905–910 (1994).
- Trimarchi S, Smith DE, Share D et al. Retroperitoneal hematoma after percutaneous coronary intervention: prevalence, risk factors, management, outcomes, and predictors of mortality: a report from the BMC2 (Blue Cross Blue Shield of Michigan Cardiovascular Consortium). JACC Cardiovasc. Interv. 3(8), 845–850 (2010).
- Nasser TK, Mohler ER 3rd, Wilensky RL, Hathaway DR. Peripheral vascular complications following coronary interventional procedures. Clin. Cardiol. 18(11), 609–614 (1995).
- Ahmad F, Turner SA, Torrie P, Gibson M. Iatrogenic femoral artery pseudoaneurysms – a review of current methods of diagnosis and treatment. Clin. Radiol. 63(12), 1310–1316 (2008).
- Franchi E, Marino P, Biondi-Zoccai GG, De Luca G, Vassanelli C, Agostoni P. Transradial versus transfemoral approach for percutaneous coronary procedures. Curr. Cardiol. Rep. 11(5), 391–397 (2009).
- Sciahbasi A, Pristipino C, Ambrosio G et al. Arterial access-site-related outcomes of patients undergoing invasive coronary procedures for acute coronary syndromes (from the ComPaRison of early invasive and conservative treatment in patients with Non– ST-ElevatiOn acute coronary syndromes [PRESTO-ACS] vascular substudy). Am. J. Cardiol. 103(6), 796–800 (2009).
- Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomized, parallel group, multicentre trial. Lancet 377(9775), 1409–1420 (2011).
- Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact of major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157(1), 132–140 (2009).
- Sanmartin M, Cuevas D, Goicolea J, Ruiz-Salmeron R, Gomez M, Argibay V. Vascular complications associated with radial artery access for cardiac catheterization. Rev. Esp. Cardiol. 57(6), 581–584 (2004).
- Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusionpatent hemostasis evaluation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after transradial catheterization. Catheter Cardiovasc. Interv. 72(3), 335–340 (2008).
- Jacobi JA, Schussler JM, Johnson KB. Routine femoral head fluoroscopy to reduce complications in coronary catheterization. Proc. (Bayl. Univ. Med. Cent.) 22(1), 7–8 (2009).
- Abu-Fadel MS, Sparling JM, Zacharias SJ et al. Fluoroscopy vs. traditional guided femoral arterial access and the use of closure devices: a randomized controlled trial. Catheter Cardiovasc. Interv. 74(4), 533–539 (2009).
- Fitts J, Ver Lee P, Hofmaster P, Malenka D. Fluoroscopy-guided femoral artery puncture reduces the risk of PCI-related vascular complications. J. Interv. Cardiol. 21(3), 273–278 (2008).
- Seto AH, Abu-Fadel MS, Sparling JM et al. Real-time ultrasound guidance facilitates femoral arterial access and reduces vascular complications: FAUST (femoral arterial access with ultrasound trial). JACC Cardiovasc. Interv. 3(7), 751–758 (2010).
- Lefkovits J, Plow EF, Topol EJ. Platelet glycoprotein IIb/IIIa receptors in cardiovascular medicine. N. Engl. J. Med. 332(23), 1553–1559 (1995).
- Proimos G. Platelet aggregation inhibition with glycoprotein IIb–IIIa inhibitors. J. Thromb. Thrombolysis 11(2), 99–110 (2001).
- The EPIC Investigators: use of a monoclonal antibody directed against the platelet glycoprotein IIb/IIIa receptor in high-risk coronary angioplasty. The EPIC investigation. N. Engl. J. Med. 330(14), 956–961 (1994).
- Kereiakes DJ, Lincoff AM, Miller DP et al. Abciximab therapy and unplanned coronary stent deployment: Favorable effects on stent use, clinical outcomes, and bleeding complications. Circulation 97(9), 857–864 (1998).
- Mascelli MA, Lance ET, Damaraju L, Wagner CL, Weisman HF, Jordan RE. Pharmacodynamic profile of short-term abciximab treatment demonstrates prolonged platelet inhibition with gradual recovery from GP IIb/IIIa receptor blockade. Circulation 97(17), 1680–1686 (1998).
- Moen MD, Keating GM, Wellington K. Bivalirudin: a review of its use in patients undergoing percutaneous coronary intervention. Drugs 65(13), 1869–1891 (2005).
- Stone GW, McLaurin BT, Cox DA et al. Bivalirudin for patients with acute coronary syndromes. N. Engl. J. Med. 355(21), 2203–2216 (2006).
- Stone GW, Witzenbichler B, Guagliumi G et al. Bivalirudin during primary PCI in acute myocardial infarction. N. Engl. J. Med. 358(21), 2218–2230 (2008).
- Stone PA, AbuRahma AF, Flaherty SK, Bates MC. Femoral pseudoaneurysms. Vasc. Endovascular Surg. 40(2), 109–117 (2006).
- Dauerman HL, Applegate RJ, Cohen DJ. Vascular closure devices: the second decade. J. Am. Coll. Cardiol. 50(17), 1617–1626 (2007).
- Applegate RJ, Sacrinty M, Kutcher MA et al. Vascular complications with newer generations of AngioSeal vascular closure devices. J. Interv. Cardiol. 19(1), 67–74 (2006).
- Hermiller JB, Simonton C, Hinohara T et al. The StarClose vascular closure system: Interventional results from the CLIP study. Catheter Cardiovasc. Interv. 68(5), 677–683 (2006).
- Doyle BJ, Godfrey MJ, Lennon RJ et al. Initial experience with the cardiva boomerang vascular closure device in diagnostic catheterization. Catheter Cardiovasc. Interv. 69(2), 203–208 (2007).
- Scheinert D, Sievert H, Turco MA et al. The safety and efficacy of an extravascular, water-soluble sealant for vascular closure: initial clinical results for Mynx. Catheter Cardiovasc. Interv. 70(5), 627–633 (2007).
- Wong SC, Bachinsky W, Cambier P et al. A randomized comparison of a novel bioabsorbable vascular closure device versus manual compression in the achievement of hemostasis after percutaneous femoral procedures: the ECLIPSE (Ensure’s Vascular Closure Device Speeds Hemostasis Trial). JACC Cardiovasc. Interv. 2(8), 785–793 (2009).
- Bavry AA, Raymond RE, Bhatt DL et al. Efficacy of a novel procedure sheath and closure device during diagnostic catheterization: the multicenter randomized clinical trial of the FISH device. J. Invasive Cardiol. 20(4), 152–156 (2008).
- Sohail MR, Khan AH, Holmes DRJ, Wilson WR, Steckelberg JM, Baddour LM. Infectious complications of percutaneous vascular closure devices. Mayo Clin. Proc. 80(8), 1011–1015 (2005).
- Dangas G, Mehran R, Kokolis S et al. Vascular complications after percutaneous coronary interventions following hemostasis with manual compression versus arteriotomy closure devices. J. Am. Coll. Cardiol. 38(3), 638–641 (2001).
- Koreny M, Riedmüller E, Nikfardjam M, Siostrzonek P, Müllner M: Arterial puncture closing devices compared with standard manual compression after cardiac catheterization: systematic review and meta-analysis. JAMA 291(3), 350–357 (2004).
- Nikolsky E, Mehran R, Halkin A et al. Vascular complications associated with arteriotomy closure devices in patients undergoing percutaneous coronary procedures. J. Am. Coll. Cardiol. 44(6), 1200–1209 (2004).
- Arora N, Matheny ME, Sepke C, Resnic FS. A propensity analysis of the risk of vascular complications after cardiac catheterization procedures with the use of vascular closure devices. Am. Heart J. 153(4), 606–611 (2007).
- Resnic FS, Arora N, Matheny M, Reynolds MR. A cost-minimization analysis of the angio-seal vascular closure device following percutaneous coronary intervention. Am. J. Cardiol. 99(6), 766–770 (2007).
- Azmoon S, Pucillo AL, Aronow WS et al. Vascular complications after percutaneous coronary intervention following hemostasis with the Mynx vascular closure device versus the AngioSeal vascular closure device. J. Invasive Cadiol. 22(4), 175–178 (2010).
- Applegate RJ. Interventional management of femoral vascular complications. Cardiac Interventions Today 31–34 (2008).
- Lenartova M, Tak T. Iatrogenic pseudoaneurysm of femoral artery: case report and literature review. Clin. Med. Res. 1(13), 243–247 (2003).
- Chan YC, Morales JP, Reidy JF, Taylor PR. Management of spontaneous and iatrogenic retroperitoneal haemorrhage: conservative management, endovascular intervention, or open surgery? Int. J. Clin. Pract. 62(10), 1604–1613 (2008).
- Silva JA, Stant J, Ramee SR. Endovascular treatment of a massive retroperitoneal bleeding: successful balloon-catheter delivery of intra-arterial thrombin. Catheter Cardiovasc. Interv. 64(2), 218–222 (2005).
- Kent KC, Moscucci M, Mansour KA et al. Retroperitoneal hematoma after cardiac catheterization: prevalence, risk factors, and optimal management. J. Vasc. Surg. 20(6), 905–910 (1994).
- Kinnaird TD, Stabile E, Mintz GS et al. Incidence, predictors, and prognostic implications of bleeding and blood transfusion following percutaneous coronary interventions. Am. J. Cardiol. 92(8), 930–935 (2003).
- Kinnaird T, Anderson R, Hill J, Thomas M. Bleeding during percutaneous intervention: tailoring the approach to minimise risk. Heart 95(1), 15–19 (2009).
- Doyle BJ, Ting HH, Bell MR et al. Major femoral bleeding complications after percutaneous coronary intervention: incidence, predictors, and impact on long-term survival among 17,901 patients treated at the Mayo Clinic from 1994 to 2005. JACC Cardiovasc. Interv. 1(2), 202–209 (2008).
▪ Study identifying characteristics associated with vascular complications and a model for predicting risk.
▪▪ Observational study investigating outcomes of patients undergoing transradial access compared to femoral access.
▪▪ Trial comparing radial and femoral access for percutaneous coronary intervention.
▪▪ Prospective study investigating angiographic suitability of puncture site using fluoroscopic guidance versus traditional anatomic landmark guidance for vascular closure device use.
▪ Prospective study comparing femoral arterial access between standard fluoroscopic guidance versus ultrasound guidance.
▪▪ Analysis of the economic advantages of angio-seal for vascular closure.
▪▪ Study reporting the decreasing incidence of femoral access complications over the past decade.