Research Article - Interventional Cardiology (2021) Volume 13, Issue 6
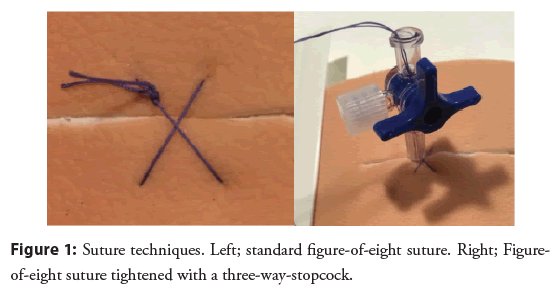
Figure-of-eight suture combined with a three-way stopcock for venous closure following left atrial appendage occlusion or patent foramen ovale closure
- Corresponding Author:
- Asger Andersen
Department of Cardiology,
Aarhus University Hospital,
Aarhus,
Denmark,
E-mail: asger.andersen@clin.au.dk
Received date: August 30, 2021; Accepted date: September 13, 2021; Published date: September 20, 2021
Abstract
Background: No guidelines exist regarding venous access site closure after catheterbased procedures. This study aimed to compare standard figure-of-eight suture with a modified version tightened by a three-way-stopcock with regards to postprocedural bleeding incidence, bleeding duration, time to ambulation and possible predictors of bleeding.
Methods and findings: A prospective cohort study of consecutive patients undergoing left atrial appendage occlusion or patent foramen ovale closure between April 2019 and October 2020 (n=208). A standard figure-of-eight suture closed with a surgical knot was applied in the first 103 patients and a three-way-stopcock was used to close the figure-of-eight suture in the subsequent 105 patients. Study outcomes were any postprocedural bleeding, duration of bleeding and time to ambulation. Bleeding was categorized as minor if time to ambulation was unchanged, moderate if time was prolonged or severe if the bleeding required intervention (transfusion or surgery).
Results: A total of 208 patients were included. Any bleeding occurred in 77 patients (75.5%) in the standard-group and 79 patients (75.2%) in the stopcock-group, p=0.97. Moderate bleeding occurred in 39 (37.9%) and 40 (38.1%) patients in the standard versus stopcock-group, respectively, p=0.99. In patients with moderate bleeding, median bleeding duration was 296 min (IQR: 195-555) in the standard group and 195 min (IQR: 87.5-302.5) in the stopcock group, p<0.01. Time to ambulation did not significantly differ between the groups (120 min vs. 90 min, p=0.31). No predictors of bleeding were identified.
Conclusion: A three-way-stopcock to secure the figure-of-eight suture did not reduce bleeding incidence, but bleeding duration was reduced in patients with moderate bleeding. Data must be confirmed by larger randomized studies.
Keywords
Three-way stopcock • Figure-of-eight suture • Hemostasis • Patent foramen ovale • Left atrial appendage
Abbreviations
ACT: Activated Clotting Time; APT: Anti-Platelet Therapy; BMI: Body Mass Index; CRF: Case Report Form; HEM: Hematoma; IQR: Interquartile range; LAA: Left Atrial Appendage; LMWH: Low-Molecular-Weight Heparin; NOAC: Non-vitamin K oral anticoagulants; PFO: Patent Foramen Ovale; PO: Postoperative; SD: Standard Deviation; SL: Skin Leakage; VKA: Vitamin-K Antagonists; VL: Venous Leakage; SAPT: Single Antiplatelet Therapy
Introduction
The most common complications following cardiac catheterization procedures are related to the vascular access site [1]. The use of larger venous sheaths to deploy devices has expanded, resulting in a corresponding increase of groin complications [2,3]. In contrast to venous closure techniques, a variety of closure devices are available for arterial puncture sites, and no guidelines exist regarding closure of venous access sites.
Traditionally, manual compression followed by application of a compression bandage and bed rest has been the way to obtain hemostasis after venous puncture. However, suture-based techniques such as the figure-of-eight suture, the Proglide suture (Abbott, USA) and the purse-string suture have emerged as alternative methods of closing venous puncture sites [4-7].
Venous access closure by a figure-of-eight suture reduces time to hemostasis, the time in the laboratory and risk of access site complications as compared to manual compression [8-10]. Time to ambulation is reduced when using a purse-string suture instead of manual compression [11].
Suture-based closure techniques requires suture removal by nursing staff, and when removed, tension cannot be maintained or resumed if subsequent bleeding occurs. These challenges may be manageable by modifying the figure-of-eight suture with a three-way-stopcock. This enables loosening or tightening of the suture to gradually assess hemostasis and reobtain compression by tightening the suture if bleeding occurs. A prior retrospective study suggests a three-way-stopcock secured figure-of-eight suture as safe as the standard figure-of-eight suture when achieving immediate hemostasis in atrial ablation procedures [6]. However, this was limited by a small study population (n=100) and the use of only small sheath sizes. The three-way-stopcock secured figureof- eight suture has also been shown safe and with reduced time to hemostasis in cryoablated patients compared to the standard figure-of-eight suture. This study suggest the suture secured by the three-way-stopcock safe for closure of venous access sites using larger sheaths sizes [12]. The literature is promising regarding the three-way-stopcock secured figure-of-eight suture, though limited to the studies above. Thus, further studies are warranted.
The present study was intended to prospectively compare the figureof- eight suture with the three-way-stopcock secured figure-ofeight suture in patients undergoing intracardiac echocardiography guided occlusion of either Patent Foramen Ovale (PFO) or Left Atrial Appendage (LAA). Our aim was to evaluate the impact on postprocedural bleeding incidence, duration of bleeding and time to ambulation. Our main hypothesis was that a three-waystopcock secured figure-of-eight suture technique would allow improvements in workflow by reducing duration of postprocedural bleeding, time to ambulation and required nursing staff resources. Furthermore, we aimed to identify potential predictors of groin bleeding.
Materials and Methods
Study design
We performed a prospective, non-randomized cohort study including 208 consecutive patients, who underwent occlusion of either LAA (n=108), or PFO (n=100) between April 2019 and October 2020. All procedures were performed at the Department of Cardiology, Aarhus University Hospital and executed by experienced operators. Baseline and procedural characteristics, along with closure technique and outcomes were prospectively collected. All outcomes were adjudicated based on the electronic patient medical records. The study included two consecutive cohorts, the first 103 patients received the standard figure-of-eight suture and the subsequent 105 patients received the figure-of-eight suture using the three-way-stopcock approach. One patient was excluded as no suture was applied at the laboratory. The study used an explorative approach to the analysis of data.
As per Danish law, the study was approved by the institution and performed in accordance with the Danish Data Protection Act. All patients gave informed consent before their designated procedure.
Interventional procedures
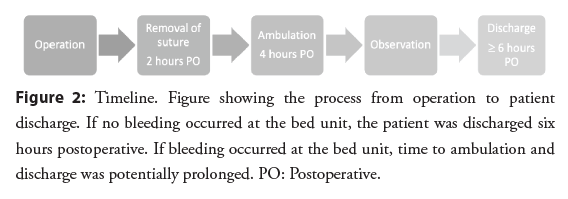
Venous access was established through ultrasound-guided puncture of the right femoral vein. The size of sheaths ranged from 6-12 Fr for the PFO procedures and from 8-14 Fr for the LAA procedures. All patients had two separate vein punctures in the right femoral vein with insertion of two separate sheaths. A 20 cm long 9F Terumo sheath was inserted into the most inferior and medial puncture site for introducing the ICE catheter and the more superior and lateral venous puncture site was used for the transseptal sheath and the device delivery sheaths. PFO closure was performed with an Amplatzer™ PFO occluder (Abbott Vascular, Plymouth, MN) or a GORE® CARDIOFORM Septal Occluder (GSO; W.L. Gore and Associates, Flagstaff, AZ). LAA devices used were the Watchman FLX (Boston Scientific, Marlborough, Massachusetts), size 20-35 mm or the Amplatzer Amulet (Abbott, Abbott Park, Illinois), size 16-34 mm. During the procedure, weight-adapted heparin (100 IE/kg) was administered and Activated Clotting Time (ACT) was measured at the end of the procedure. Before removing the sheaths, venous access sites were closed using either a figure-ofeight suture or a figure-of-eight suture and three-way-stopcock (Figure 1). The suture used was non-absorbable and was removed two hours postoperatively if hemostasis was obtained. Patients were ambulated following additional two hours. If patients were successfully ambulated, defined as a well-being patient with no observed groin bleeding, the patient was observed for at least two hours before discharge (Figure 2). In the event of groin bleeding, standard practice for achieving hemostasis started by compression or tightening of the three-way-stopcock. Compression was done either manually or by placing a sandbag. In the need for further intervention to obtain hemostasis, the nurses chose between a hemostatic wound dressing or a suture according to the bleeding severity.
Data registration
Data was collected prospectively using a pre-specified Case Report Form (CRF). Data completeness and correctness was monitored based on source data from the electronic patient medical file.
Bleeding definitions
Postoperative groin bleeding was defined as any bleeding observed and documented during the time at the ward and characterized as either venous leakage, skin leakage or hematoma. Bleeding was categorized as minor, moderate, or severe. Minor bleeding was defined as patients with successful ambulation after four hours in bed despite observed minor bleeding. Moderate bleeding defined patients with observed bleeding resulting in prolonged time to ambulation. Severe bleeding was bleeding that required intervention e.g. transfusion or surgery.
Bleeding duration was defined as time from first observation of a bleeding until ambulation without bleeding. Prolonged time to ambulation was defined as more than four hours in bed after the procedure caused by groin bleeding. Prolonged time to ambulation caused by busy staff or other adverse events was categorized as regular time to ambulation if no groin bleeding was observed.
Statistical analyses
The distribution of data was assessed using QQ-plot and histogram. Continuous variables were expressed as mean with Standard Deviation (SD), or median with Interquartile Range (IQR), and were compared using the student t-test or Mann-Whitney U test as appropriate. Categorical variables were reported as counts and percentages, and groups were compared using Fishers exact test. A multivariable logistic regression model was used to estimate risk ratios with adjustment for between group imbalances. A 2-tailed p-value<0.05 was considered statistically significant. Statistical analysis was performed using STATA (STATA IC, version 14.2, StataCorp, College Station, Texas).
Results
A total of 208 patients who underwent occlusion of either LAA or PFO were included in the study. A standard figure-of-eight suture was applied in 103 patients (Standard-group) and a three-waystopcock was applied to tighten the figure-of-eight suture in 105 patients (Stopcock-group). Mean age in the cohort was 62 years (± 15.6) years and 73% were male. Further baseline characteristics are summarized in Table 1. No differences were found between the groups concerning age, gender, comorbidities, and smoking status. However, the procedure time was longer, and the size of the largest sheath was wider in the standard-group. Heparin dosage was higher in the stopcock-group, though the ACT did not differ between the two groups. Furthermore, use of antithrombotic therapy varied between the two groups, and groin bleeding started slightly later in the stopcock-group. No major complications such as arterio-venous fistulas or pseudoaneurysms were observed.
| Total (n=208) | Standard (n=103) | Stopcock (n=105) | p-value | |
|---|---|---|---|---|
| Age, year | 62 (15.6) | 64 (15.9) | 61 (15.2) | 0.14 |
| Male, gender, n (%) | 151 (72.6%) | 76 (73.8%) | 75 (71.4%) | 0.76 |
| Hypertension, n (%) | 103 (49.5%) | 53 (51.5%) | 50 (47.6%) | 0.68 |
| Diabetes, n (%) | 42 (20.2%) | 19 (18.4%) | 23 (21.9%) | 0.61 |
| BMI | 27.3 (4.7) | 26.8 (4.4) | 27.7 (5.0) | 0.15 |
| Smoking status, n (%) | ||||
| Never smokers | 94 (47.0%) | 49 (47.6%) | 45 (42.9%) | 0.69 |
| Current smokers | 25 (12.5%) | 15 (14.6%) | 10 (9.5%) | 0.49 |
| Ex-smokers | 81 (40.5%) | 36 (35.0%) | 45 (42.9%) | 0.36 |
| Hgb (mmol/L), median (IQR) | 8.7 (7.7, 9.3) | 8.4 (7.4, 9.2) | 8.8 (7.8, 9.3) | 0.23 |
| Antithrombotic therapy, n (%) | ||||
| None | 28 (13.5%) | 18 (17.5%) | 10 (9.5%) | 0.11 |
| VKA or LMWH | 18 (8.7%) | 10 (9.7%) | 8 (7.6%) | 0.63 |
| NOAC | 52 (25.0%) | 30 (29.1%) | 22 (21.0%) | 0.2 |
| SAPT | 89 (42.8%) | 41 (39.8%) | 48 (45.7%) | 0.4 |
| Combination | 21 (10.1%) | 4 (3.9%) | 17 (16.2%) | 0.005 |
| Procedure, n (%) | ||||
| PFO | 100 (48.1%) | 43 (41.7%) | 57 (54.3%) | 0.07 |
| LAA | 108 (51.9%) | 60 (58.3%) | 48 (45.7%) | 0.07 |
| Procedure time, (min), median | 29 (19, 41) | 32 (22, 44) | 23 (17, 36) | <0.01 |
| Largest sheath (F) | ||||
| 8 Fr | 13 (6.2%) | 10 (9.7%) | 3 (2.9%) | 0.048 |
| 9 Fr | 2 (1.0%) | 2 (1.9%) | 0 (0.0%) | 0.24 |
| 11 Fr | 83 (39.9%) | 30 (29.1%) | 53 (50.5%) | 0.002 |
| 12 Fr | 24 (11.5%) | 12 (11.7%) | 12 (11.4%) | 0.99 |
| 14 Fr | 86 (41.3%) | 49 (47.6%) | 37 (35.2%) | 0.99 |
| ACT (sec) | 300.3 (51.9) | 298.8 (54.7) | 301.7 (49.2) | 0.69 |
| Hemostasis, lab, n (%) | 208 (100.0%) | 103 (100.0%) | 105 (100.0%) | 1 |
| Heparin dosage, lab (I IE), median | 8000 (7000, 9000) | 7500 (7000, 8500) | 8500 (7500, 9500) | 0.01 |
Abbreviations: IQR: Interquartile range; VKA: Vitamin-K Antagonists; LMWH: Low-Molecular-Weight Heparin; NOAC: Non-vitamin K oral anticoagulants; PFO: Patent Foramen Ovale; LAA: Left Atrial Appendage; ACT: Activated Clotting Time; SAPT: Single Antiplatelet Therapy
Table 1: Baseline characteristics.
Bleeding incidence
Bleeding occurred in 77 patients (75.5%) in the standard-group and in 79 patients (75.2%) in the stopcock-group, p=0.97. Minor bleeding without prolonged time to ambulation occurred in 38 patients (36.9%) in the standard-group and in 39 patients (37.1%) in the stopcock-group, while moderate bleeding occurred in 39 patients (37.9%) in the standard-group and in 40 patients (38.1%) in the stopcock-group, p=0.99. There were no patients with severe bleeding (Table 2). In a logistic regression model adjusting for ACT, sheath size, antithrombotic therapy, BMI, smoking status, procedure type and duration, the relative risk of bleeding using the stopcock method was 1.00, (CI 0.84-1.18), p=0.96.
| Total (n=208) | Standard (n=103) | Stopcock (n=105) | p-value | |
|---|---|---|---|---|
| Groin bleeding, ward, n (%) | 156 (75.4%) | 77 (75.5%) | 79 (75.2%) | 0.97 |
| Time to bleeding from vascular closure (min), median | 130 (76, 158) | 127 (62, 150) | 136 (119, 167) | 0.03 |
| Bleeding characteristics | ||||
| Hematoma | 4 (2.6%) | 1 (1%) | 3 (4%) | 0.62 |
| Venous leakage | 93 (59.6%) | 46 (60%) | 47 (59%) | 1 |
| Skin leakage | 27 (17.3%) | 13 (17%) | 14 (18%) | 1 |
| HEM+VL | 16 (10.3%) | 9 (12%) | 7 (9%) | 0.61 |
| HEM+SL | 2 (1.3%) | 1 (1%) | 1 (1%) | 1 |
| VL+SL | 10 (6.4%) | 6 (8%) | 4 (5%) | 0.53 |
| HEM+VL+SL | 4 (2.6%) | 1 (1%) | 3 (4%) | 0.62 |
| Bleeding categorization | ||||
| Minor | 77 (37.0%) | 38 (36.9%) | 39 (37.1%) | 1 |
| Moderate | 79 (38.0%) | 39 (37.9%) | 40 (38.1%) | 1 |
| Severe | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 |
| Duration of bleeding (min), median | 120 (10, 280) | 180 (10, 390) | 90 (10, 245) | 0.15 |
| Prolonged ambulation, n (%) | 79 (38.0%) | 39 (37.9%) | 40 (38.1%) | 0.97 |
| Additional time to ambulation (min), median | 0 (0, 75) | 0 (0, 90) | 0 (0, 75) | 0.81 |
Abbreviations: VL: Venous Leakage; SL: Skin Leakage; HEM: Hematoma
Table 2: Outcomes of this study.
Bleeding duration
The overall bleeding duration in in the standard-group was 180 min (IQR: 10-390) and 90 min (IQR: 10-245) in the stopcockgroup, p=0.15. The median bleeding duration in patients with minor bleeding was 10 min (IQR: 5-60) in the standard-group, and 10 min (IQR: 5-90) in the stopcock-group, p=0.94. The median bleeding duration in patients with moderate bleeding was 296 min (IQR: 195-555) in the standard-group and 195 min in the stopcock group (IQR: 87.5-302.5), p<0.01.
Time to ambulation
The median prolonged time to ambulation in patients with moderate bleeding was 120 min (IQR: 60-600) in the standardgroup, and 90 min (IQR: 60-180) in the stopcock-group, p=0.31.
Approaches to obtain hemostasis3
Actions for achieving hemostasis were taken by the nurses at the ward. Compression, either manual or using a sandbag, was performed in 63 patients (81.8%) in the standard-group and in 64 patients (81.0%) in the stopcock-group, p=1.00. A hemostatic wound dressing was used in four patients in the standard-group, and in four patients in the stopcock-group. One patient in the standard group was treated with the FemoStopTM (Abbott, United States of America) and five patients received a skin-suture in the stopcock-group. The three-way-stopcock was retightened in 12 patients.
Predictors of bleeding
No predictors of bleeding were identified by univariate analysis (Table 3).
| No bleeding (N=52) | Minor bleeding (N=77) | Moderate bleeding (N=79) | p-value | |
| Age, year | 60 (16.1) | 61 (16.0) | 65 (14.7) | 0.21 |
| Male, gender, n (%) | 38 (73.1%) | 57 (74.0%) | 56 (70.9%) | 0.9 |
| Hypertension, n (%) | 26 (50.0%) | 32 (41.6%) | 45 (57.0%) | 0.16 |
| Diabetes, n (%) | 13 (25.0%) | 13 (16.9%) | 16 (20.3%) | 0.51 |
| BMI | 27.5 (5.9) | 26.7 (3.9) | 27.6 (4.5) | 0.39 |
| Smoking status, n (%) | ||||
| Never smokers | 23 (44.2%) | 34 (44.2%) | 37 (46.8%) | 0.9 |
| Current smokers | 10 (19.2%) | 8 (10.4%) | 7 (8.9%) | 0.38 |
| Ex-smokers | 18 (34.6%) | 31 (40.3%) | 32 (40.5%) | 0.79 |
| Hgb (mmol/L), median | 8.7 (8.0, 9.3) | 8.5 (7.4, 9.3) | 8.8 (7.8, 9.2) | 0.92 |
| Procedure, n (%) | ||||
| PFO | 28 (53.8%) | 39 (50.6%) | 33 (41.8%) | 0.35 |
| LAA | 24 (46.2%) | 38 (49.4%) | 46 (58.2%) | 0.35 |
| Procedure time, median | 25 (18.5, 38.5) | 25 (18, 38) | 32 (20, 42) | 0.23 |
| Largest sheath (Fr), n (%) | ||||
| 8 | 4 (7.7%) | 6 (7.8%) | 3 (3.8%) | 0.51 |
| 9 | 1 (1.9%) | 0 (0.0%) | 1 (1.3%) | 0.72 |
| 11 | 22 (42.3%) | 32 (41.6%) | 29 (36.7%) | 0.78 |
| 12 | 5 (9.6%) | 10 (13.0%) | 9 (11.4%) | 0.89 |
| 14 | 20 (38.5%) | 29 (37.7%) | 37 (46.8%) | 0.89 |
| ACT (sec) | 293.7 (48.7) | 297.4 (55.0) | 307.6 (50.3) | 0.3 |
| Heparin dosage on lab (I IE), median | 7500 (6500, 9750) | 8000 (7000, 8500) | 8000 (7500, 9000) | 0.14 |
| Antithrombotic therapy, n (%) | ||||
| None | 8 (15.4%) | 10 (13.0%) | 10 (12.7%) | 0.9 |
| VKA or LMWH | 5 (9.6%) | 6 (7.8%) | 7 (8.9%) | 0.95 |
| NOAC | 9 (17.3%) | 18 (23.4%) | 25 (31.6%) | 0.17 |
| SAPT | 25 (48.1%) | 34 (44.2%) | 30 (38.0%) | 0.5 |
| Combination | 5 (9.6%) | 9 (11.7%) | 7 (8.9%) | 0.84 |
Abbreviations: PFO: Patent Foramen Ovale; LAA: Left Atrial Appendage; ACT: Activated Clotting Time; VKA: Vitamin-K Antagonists; LMWH: Low-Molecular-Weight Heparin; NOAC: Non-vitamin K oral anticoagulants; SAPT: Single Antiplatelet Therapy
Table 3: Predictors of bleeding.
Discussion
Data showed a reduction in bleeding duration of 101 min when using the three-way-stopcock compared to the traditional figure-of-eight suture in patients with moderate groin bleeding. However, this reduced bleeding duration did not reduce the time to ambulation. No predictors of bleeding were identified.
Bleeding risk
Our study did not show a reduced incidence of bleeding with the three-way-stopcock approach. Similar findings have previously been reported with a modified figure-of-eight suture secured by a torque device, probably equivalent to the mechanism of a threeway- stopcock [13].
Bleeding from the venous puncture site was observed in approximately 75% of our cohort. This is a fairly high bleeding rate compared to other studies. However, definitions of an event of groin bleeding may vary across studies. When focusing on patients with bleeding leading to prolonged time to ambulation, the bleeding rate is 37.9% in the standard-group and 38.1% in the stopcock-group. This number corresponds to a study of manual compression of either four or six hours, after venous puncture, where venous bleeding complications were identified in 38.1% of the patients [14].
A meta-analysis of nine studies found a reduction in access site bleeding when standard figure-of-eight suture was compared to manual compression [8]. The application of a three-way-stopcock should theoretically apply the same tension as a standard suture, however, the advantages lies in the ability to continuously assess and re-assess hemostasis by loosening and tightening the suture if needed.
Bleeding duration
In patients with moderate groin bleeding, the bleeding duration was significantly reduced when using the three-way-stopcock. The underlying mechanisms of this observation are unclear, but likely related to the actions performed by the nursing staff. The slow release of tension and the possibility to assess the puncture site without removing the suture, may be one of the explanations. However, the three-way-stopcock was only retightened in 12 patients - a relative low number when considering 40 patients with moderate bleeding in the stopcock-group. In light of this, application of the three-way-stopcock may not explain the entire reduction in bleeding duration seen in our study. The explanation is likely multifactorial.
Reduced bleeding duration after invasive procedures is convenient for the patient and may free up clinical resources. Compression conducted to obtain hemostasis was executed equally between the standard- and the stopcock group, but the time spent on compression might be different. The figure-of-eight suture was removed two hours postoperatively. If hemostasis was not obtained, the nurses had the opportunity of manual compression or placing a sandbag. Most frequently, manual compression was performed, taking up valuable resources. A median bleeding time of 296 min in the group of moderate bleeding with figure-of-eight suture could thus entail prolonged occupation of staff for manual compression. If the bleeding did not stop by compression, a hemostatic wound dressing, skin suture or FemoStopTM was applied. All of these approaches are staff-dependent and time-consuming. Tightening a three-way-stopcock is quick, easy, and provides the staff with a possibility to evaluate the grade of hemostasis continuously without removing the suture. Therefore, the use of a three-waystopcock could potentially be a resource-efficient and cost saving method for closing venous access sites. In addition, removal of the three-way-stopcock might be less uncomfortable and faster than the figure-of-eight suture, though not examined in our study.
Time to ambulation
Time to ambulation did not significantly differ between the two groups in our study. This confirms data from a study concerning cryoablation procedures comparing the standard figure-of-eight suture with the figure-of-eight suture and three-way-stopcock [12]. However, the suture was removed four hours postoperative as opposed to two hours in our study. The median time to ambulation was four hours, which is comparable to our study. Thus, removing the suture after two hours did not seem to modify the time to ambulation. Furthermore, using a three-way-stopcock did not decrease time to ambulation. Groin bleedings occurred earlier after the procedures in the standard-group compared to the stopcock-group, which may partly explain the comparable time to ambulation despite longer bleeding duration.
Approaches to obtain hemostasis
The use of a three-way-stopcock enables a new approach for the ward staff to obtain hemostasis. Surprisingly, utilization of the possibility to tighten the three-way-stopcock was infrequent. This may reflect lack of confidence in this approach between the nurses. We speculate that an extended use of the opportunities given by the three-way-stopcock, may reduce the duration of bleeding even more than showed in our study.
Predictors of bleeding
We were not able to identify any predictors of bleeding after closure of the femoral vein access. Low BMI and use of antiplatelet therapy are reported as risk factors of bleeding after closure of venous access sites [14]. In this case, manual compression was used to obtain hemostasis, and bleeding was defined as hemorrhage needing recompression. Age, gender, hypertension, diabetes and procedure time were not identified as predictors of bleeding [13]. A study of access site complications after electrophysiological procedures showed no association between age, gender, BMI, ACT or sheath size and the development of access site hematomas [15]. Thus, it seems reasonable to view the differences in procedure time and sheath size found between the standard- and the stopcockgroups in our study to contribute with insignificant confounding.
Conclusion
This study suggests that venous closure using a figure-of-eight suture secured by a three-way-stopcock does not affect the risk of groin bleeding, but may reduce duration of bleeding in patients requiring any bedside bleeding intervention. Moreover, the threeway- stopcock did not reduce time to ambulation. These findings warrant confirmation in a randomized trial.
Limitations
The study has the inherent limitations of a single-center, nonrandomized, observational study. However, comparison of two consecutive cohorts within contemporary periods should reduce bias. The relatively restricted sample size, limited number of procedures and sheath sizes may affect the power of conclusions, yet, the study was designed as an explorative, hypothesis-generating study. Postoperative groin bleeding was assessed by multiple nurses at the ward.
References
- Wiley JM, White CJ, Uretsky BF. Noncoronary complications of coronary intervention. Catheter Cardiovasc Interv. 57(2): 257-65 (2002).
- Shaw JA, Dewire E, Nugent A, et al. Use of suture-mediated vascular closure devices for the management of femoral vein access after transcatheter procedures. Catheter Cardiovasc Interv. 63(4): 439-43 (2004).
- Pacha HM, Al-Khadra Y, Soud M, et al. Percutaneous devices for left atrial appendage occlusion: A contemporary review. World J Cardiol. 11(2): 57-70 (2019).
- Geis NA, Pleger ST, Chorianopoulos E, et al. Feasibility and clinical benefit of a suture-mediated closure device for femoral vein access after percutaneous edge-to-edge mitral valve repair. Euro Intervention. 10(11): 1346-53 (2015).
- Steppich B, Stegmüller F, Rumpf PM, et al. Vascular complications after percutaneous mitral valve repair and venous access closure using suture or closure device. J Interv Cardiol. 31(2): 223-9 (2018).
- Payne J, Aznaurov S, Gautam S. Three-way stopcock suture technique for hemostasis after ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 29(12):1724-7 (2018).
- Akkaya E, Sözener K, Rixe J, et al. Venous access closure using a purse-string suture without heparin antagonism or additional compression after MitraClip implantation. Catheter Cardiovasc Interv. 96(1): 179-86 (2020).
- Mujer MT, Al-Abcha A, Flores J, et al. A comparison of figure-of-8-suture versus manual compression for venous access closure after cardiac procedures: An updated meta-analysis. Pacing Clin Electrophysiol. 43(8): 856-865 (2020).
- Jensen CJ, Schnur M, Lask S, et al. Feasibility of the figure-of-8-suture as venous closure in interventional electrophysiology: One strategy for all? Int J Med Sci. 17(7): 965-9 (2020).
- Kumar V, Wish M, Venkataraman G, et al. A randomized comparison of manual pressure versus figure-of-eight suture for hemostasis after cryoballoon ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 30(12): 2806-10 (2019).
- Kottmaier M, Bourier F, Reents T, et al. Safety and feasibility of subcutaneous purse-string suture of the femoral vein after electrophysiological procedures on uninterrupted oral anticoagulation. Am J Cardiol. 119(11): 1781-4 (2017).
- Yorgun H, Canpolat U, Ates AH, et al. Comparison of standard vs. modified "figure-of-eight" suture to achieve femoral venous hemostasis after cryoballoon based atrial fibrillation ablation. Pacing Clin Electrophysiol. 42(9): 1175-82 (2019).
- Karahalios B, Rojas SF, Singh R, et al. Torque device suture technique to achieve hemostasis in large-bore venous access. Catheter Cardiovasc Interv. 95(4): 722-5 (2020).
- Arai H, Mizukami A, Hanyu Y, et al. Risk factors for venous bleeding complication at the femoral puncture site after catheter ablation of atrial fibrillation. J Arrhythm. 36(4): 678-84 (2020).
- Dalsgaard AB, Jakobsen CS, Riahi S, et al. Groin hematoma after electrophysiological procedures-incidence and predisposing factors. Scand Cardiovasc J. 48(5): 311-6 (2014).