Case Report - Neuropsychiatry (2018) Volume 8, Issue 5
Focal Seizures and Borderline Personality Disorder Associated with Protein S Deficiency and Multiple White Matter Ischemic Lesions
- Corresponding Author:
- Masako Kinoshita
Department of Neurology, Utano National Hospital, National Hospital Organization 8 Ondoyama-Cho, Narutaki, Ukyoku, Kyoto 616-8255, Japan
Tel: +81-75-461-5121
Fax: +81-75-464-0027
Abstract
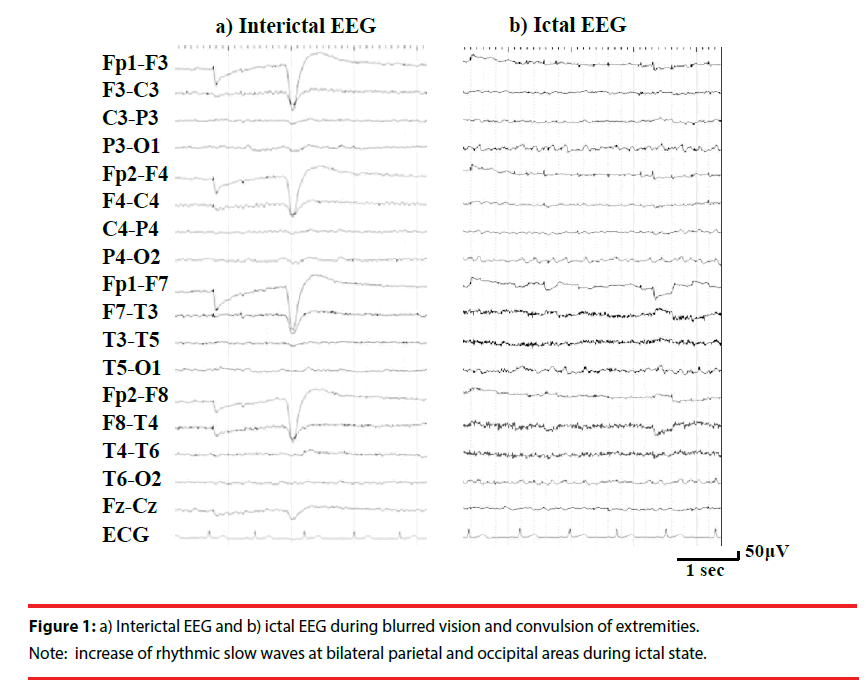
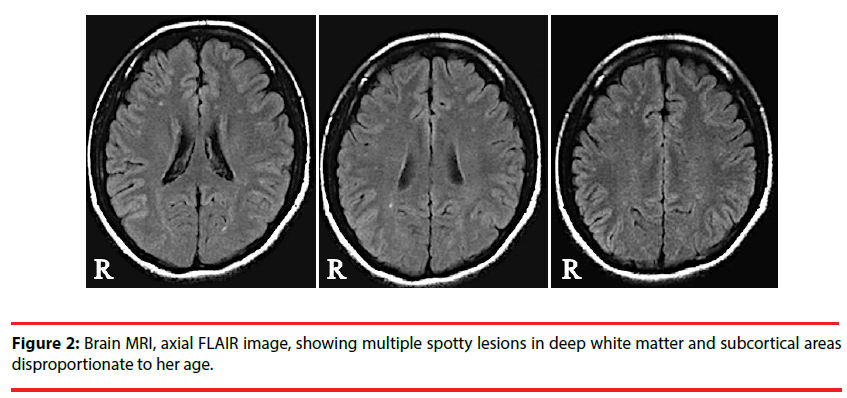
Neurological symptoms of patients with protein S deficiency remain elusive. We report a female case with protein S deficiency who started having episodes of sudden nausea, white out of the whole visual field, loss of consciousness, and falling down with convulsion at the age of 18. She was co-morbid with borderline personality disorder and gender identity disorder, and was treated with psychotherapy. She was suffering from extreme emotional lability causing deterioration of interpersonal relationships and repeated episodes of a suicidal attempt. Long-term video EEG revealed that her seizures started with abrupt visual symptoms followed by fine convulsion of extremities. Interictal EEG showed intermittent rhythmic slow waves and repetitive epileptiform discharges at bilateral parietal and occipital areas, and these activities became more frequent during ictal state. Brain MRI showed multiple spotty T2 and FLAIR high intensity lesions in deep white matter and subcortical areas disproportionate to her age. In blood test, the quantity of protein S was decreased to 53% (normal range; 65%-135%). The data of this patient suggest relationship among focal seizures, psychological complications, coagulation disorders, and brain ischemic lesion, which should be further investigated.
Keywords
Focal seizures, Borderline personality disorders, Protein S deficiency, Lacunar infarction, Subcortical infarction
Introduction
Cerebrovascular disease is one of the most important risk factors of lifetime epilepsy [1]. Cerebral infarction in large, with cortical involvement, with hemorrhagic transformation, and in patients with systemic vascular feasibility by preexisting causes such as hypertension, is known to be associated with seizures [2]. Subcortical small deep brain infarctions are more commonly seen in Japan than in European countries [3,4]. However, the role of small subcortical infarctions in development of epileptic seizures has not been fully investigated, with a variable seizure frequency of 0 to 23% [5-10]. These previous studies were conducted based on brain CT scans which can underdiagnose small cerebral lesions.
Approximately 1% of Japanese population is reported to have protein S deficiency [11]. They are presumably at high risk for coagulation disorders; however, characteristics of neurological symptoms of these patients remain elusive.
Here we investigated clinical characteristics of focal seizures in a juvenile female patient with protein S deficiency and white matter ischemic lesions. The data in this study were obtained through thorough clinical evaluation of the patient, and written informed consent was obtained from the patient. Part of this manuscript was presented in the 10th Asian & Oceanian Epilepsy Congress, held in Singapore, 2014.
Case Report
A 19-year-old right-handed female started having episodes of sudden nausea, white out of the whole visual field, loss of consciousness, and falling down with convulsion of all extremities at the age of 18. She was co-morbid with borderline personality disorder and gender identity disorder, and was treated with psychotherapy. She was suffering from extreme emotional lability causing deterioration of interpersonal relationships and repeated episodes of a suicidal attempt. She had no history of central nervous system infection, head trauma, delivery complications, or developmental abnormalities. The patient was thoroughly evaluated for the purpose of clinical management. We performed blood tests, long-term video EEG monitoring, and imaging studies.
In interictal state she had no abnormality in physical and neurological examinations. Recorded seizures comprised of abrupt visual symptoms followed by fine convulsion of one to all extrem-ities with preserved consciousness. Neurological examination during seizures revealed anisocoria, myoclonic upward eyes deviation, and positive Babinski sign. Interictal EEG showed intermittent rhythmic slow waves and repetitive epileptiform discharges at bilateral parietal and occipital areas, which became more frequent during ictal state (Figure 1). The morphology of these waves resembled to lambda waves but they were recognized irrelevant to visual scanning. Brain MRI (1.5 T) showed multiple spotty T2 and FLAIR high intensity lesions in deep white matter and subcortical areas (Figure 2). There were no microbleeds in T2* image. In blood test, the level of protein S antigen was decreased to 53% (normal range; 65%-135%) and that of protein C antigen was normal (104%, normal range; 70%- 150%). She had no causes for decreased protein S antigen such as anti-phospholipid antibody syndrome, systemic lupus erythematosus, or liver failure. She was not taking steroid or oral contraceptive. Antinuclear antibodies, anti-DNA antibody, PR3-ANCA, MPO-ANCA, anti-cardiolipin antibody, and anti-CLβ2GPI antibody were negative. Cerebrospinal fluid examination was unremarkable. We diagnosed that the patient had focal seizures associated with protein S deficiency. Her seizures were fairly controlled, but not fully suppressed, by valproate and levetiracetam. She could not tolerate with carbamazepine, gabapentin, or lamotrigine because of side effects as sleepiness, dizziness, and fever. Her emotional instability and extreme behaviors including suicidal attempt prevented her from adherence to therapy. No specific treatment was commenced for protein S deficiency; the patient was given precaution that she should avoid hypercoagulability state and that she would need careful observation during pregnancy.
Figure 2: Brain MRI, axial FLAIR image, showing multiple spotty lesions in deep white matter and subcortical areas disproportionate to her age.
Discussion
It has been reported that coagulation disorder like protein S deficiency is an independent risk factor of white matter ischemic lesion [12]. Brain MRI (1.5 T) of the present case showed multiple ischemic lesions in deep white matter and subcortical areas disproportionate to her age. When multiple subcortical infarcts are detected by standard brain MRI (<3 T), high-resolution 7 T MRI and neuropathological examination reveal countless intracortical infarcts [13]. Deposition of hemosiderin, gliosis, meningocerebral cicatrix, and down-regulation of GABAergic pathway in the ischemic lesion are associated with pathogenesis of epilepsy [13-15]. A previous case report suggests that cerebral microbleeds may cause epileptogenic focus [16]. Therefore, the data of our patient suggest a possible association between cerebral ischemic lesions due to protein S deficiency and development of focal epileptogenicity.
Patients with protein S deficiency are prone to venous thromboembolism, and recent genetic studies have demonstrated mechanism of functional abnormality leading to hypercoagulable state [17-19]. A recent study showed association between genetically proven congenital protein S deficiency and abdominal vein thromboses [20]. Arterial thrombosis can be due to deficient protein S and cause ischemic stroke in young adults [21]. Although genetic testing has not been performed in the present patient and there remain other possibilities causing to protein S deficiency, she should avoid predisposing factors for thrombosis.
Suicidal ideation and behavior in personality disorder are often difficult to manage, and several treatment options have been demonstrated including aripiprazole, time-limited use of very low dosages of sublingual buprenorphine, and mentalization-based treatment [22-24]. Patients with personality disorder are at increased risk for cardiovascular disease and stroke [25,26]. The present patient suggests that coexistence of epilepsy may play significant role in development of both suicidal ideation and personality disorder.
Conclusion
In summary, the data of this patient suggest relationship among focal seizures, psychological complications, coagulation disorders, and brain ischemic lesion. Further investigation should be performed to clarify underlying mechanisms.
Conflicts of Interest
No potential conflict of interest was reported by the authors.
References
- Li X, Breteler MM, de Bruyne MC, et al. Vascular determinants of epilepsy: the Rotterdam Study. Epilepsia 38(11), 1216-1220 (1997).
- Menon B, Shorvon SD. Ischaemic stroke in adults and epilepsy. Epilepsy. Res 87(1), 1-11 (2009).
- Turin TC, Kita Y, Rumana N, et al. Ischemic stroke subtypes in a Japanese population: Takashima Stroke Registry, 1988-2004. Stroke 41(9), 1871-1876 (2010).
- Takeda H, Takagi M, Yamamoto Y. Branch atheromatous disease: how do we analyze its pathophysiology and treat it to prevent the progression of neurological symptoms? Rinsho. Shinkeigaku 50(1), 921-924 (2010).
- Shinton RA, Gill JS, Melnick SC, et al. The frequency, characteristics and prognosis of epileptic seizures at the onset of stroke. J. Neurol. Neurosurg. Psychiatry 51(2), 273-276 (1988).
- Burn J, Dennis M, Bamford J, et al. Epileptic seizures after a first stroke: the Oxfordshire Community Stroke Project. BMJ 315(7122), 1582-1587 (1997).
- Sung CY, Chu NS. Epileptic seizures in thrombotic stroke. J. Neurol 237(3), 166-170 (1990).
- Dávalos A, de Cendra E, Molins A, et al. Epileptic seizures at the onset of stroke. Cerebrovasc. Dis 2(6), 327-331 (1992).
- Shorvon SD, Gilliatt RW, Cox TC, et al. Evidence of vascular disease from CT scanning in late onset epilepsy. J. Neurol. Neurosurg. Psychiatry 47(3), 225-230 (1984).
- Roberts RC, Shorvon SD, Cox TCS, et al. clinically unsuspected cerebral infarction revealed by computed tomography scanning in late onset epilepsy. Epilepsia 29(2), 190-194 (1988).
- Kojima T. Congenital anticoagulant deficiency. Jap. J. Thromb. Haemost 20(1), 484-486 (2009). Japanese.
- Yano C, Iwata M, Uchiyama S. Risk factors for small cortical infarction on diffusion-weighted magnetic resonance imaging in patients with acute ischemic stroke. J. Stroke. Cerebrovasc. Dis 20:68-74 (2011).
- Jouvent E, Poupon C, Gray F, et al. Intracortical infarcts in small vessel disease. A combined 7-T Postmortem MRI and neuropathological case study in cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Stroke 42(3), e27-e30 (2011).
- Ferro JM, Pinto F. Poststroke epilepsy: epidemiology, pathophysiology and management. Drugs. Aging 21(10), 639-653 (2004).
- Camilo O, Goldstein LB. Seizures and epilepsy after ischemic stroke. Stroke 35(7), 1769-1775 (2004).
- Nakagami Y, Sugihara G, Uemura K, et al. Rapidly progressive cognitive disturbances due to nonconvulsive status epilepticus associated with a cerebral microbleed: clinical application of FDG-PET. Epilepsy Seizure 7(1), 23-29 (2014).
- Comp PC, Esmon CT. Recurrent venous thromboembolism in patients with a partial deficiency of protein S. N. Engl. J. Med 311(24), 1525-1528 (1984).
- Castoldi E, Maurissen LF, Tormene D, et al. Similar hypercoagulable state and thrombosis risk in type I and type III protein S-deficient individuals from families with mixed type I/III protein S deficiency. Haematologica 95(9), 1563-1571 (2010).
- Taniguchi F, Morishita E, Sekiya A, et al. Gene analysis of six cases of congenital protein S deficiency and functional analysis of protein S mutations (A139V, C449F, R451Q, C475F, A525V and D599TfsTer13). Thromb. Res 151(1), 8-16 (2017).
- Makoto I, Usui M, Wada H, et al. Congenital Thrombophilia in Patients With Superior Mesenteric Venous Thrombosis or Portal Vein Thrombosis. Clin. Appl. Thromb. Hemost 1(1), 1-7 (2018).
- Martinez HR, Rangel-Guerra RA, Marfil LJ. Ischemic stroke due to deficiency of coagulation inhibitors. Report of 10 young adults. Stroke 24(1), 19-25 (1993).
- Nickel MK, Muehlbacher M, Nickel C, et al. Aripiprazole in the treatment of patients with borderline personality disorder: a double-blind, placebo-controlled study. Am. J. Psychiatry 163(5), 833-838 (2006).
- Yovell Y, Bar G, Mashiah M, et al. Ultra-Low-Dose Buprenorphine as a Time-Limited Treatment for Severe Suicidal Ideation: A Randomized Controlled Trial. Am. J. Psychiatry 173(5), 491-498 (2016).
- Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am. J. Psychiatry 166(12), 1355-1364 (2009).
- Moran P, Stewart R, Brugha T, et al. Personality disorder and cardiovascular disease: results from a national household survey. J. Clin. Psychiatry 68(1), 69-74 (2007).
- Chen MH, Hsu JW, Bai YM, et al. Risk of stroke among patients with borderline personality disorder: A nationwide longitudinal study. J. Affect. Disord 219(1), 80-85 (2017).