Case Report - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 4
From pancreatic neoplasm to increase of glands: A case report of IgG4-related disease and its spectrum
- Corresponding Author:
- Pedro Weingrill
1Department of Rheumatology
Universidade da Região de Joinville – UNIVILLE. Joinville, Santa Catarina, Brazil
E-mail: weingrill@terra.com.br
Abstract
Background: IgG4-Related Diseases (IgG4-RD) represent a fibroinflammatory immune-mediated condition that might affect several organs. Due to its variable clinical presentation and differential diagnosis, early and accurate diagnosis is a real challenge. This case report aims to improve the general knowledge about IgG4-RD, enabling early and correct diagnosis, avoiding unnecessary interventions, and ensuring the best quality of life for the patient. Case Report: A 44-year-old man with diabetes mellitus and dyslipidemia presented with submandibular glands hypertrophy and a positive rheumatoid factor. He had a recent medical history of undiagnosed urinary symptoms and findings of renal nodules on an abdominal Computed Tomography. Besides that, he had undergone laparotomy with enteroanastomosis after pancreatic cancer was suspected, one year before the glands’ hypertrophy appeared. After he has been reassessed by a rheumatologist, the IgG4-RD was considered due to increase in serum IgG4, affection of a pair of salivary glands, presence of low-density areas in the renal cortex, bilaterally, affection of the pancreas and biliary ducts with dense inflammatory infiltrate and storiform fibrosis in the pancreas biopsy. The treatment with prednisone was started and the patient evolved with clinical, laboratory, and radiologic resolution after that. Conclusions: The IgG4-RD is worth reporting due to the many different clinical presentations. In this case, the diagnosis was done after years of the initial symptoms, and the patient evolved with significant improvement after the right treatment was prescribed. Corroborating to the importance of correct and early diagnosis.
Keywords
rheumatology • immunoglobulin G4-related disease • submandibular gland • autoimmune diseases
Abbreviations
IgG4-RD: IgG4-Related Disease; SGOT: Serum Glutamic-Oxaloacetic Transaminase; SGPT: Serum Glutamic Pyruvic Transaminase; GGT: Gamma-Glutamyl Transferase; ALP: Alkaline Phosphatase; CRP: C-Reactive Protein; ESR: Erythrocyte Sedimentation Rate; ANF: Anti-Nuclear Factor; HBsAg: Hepatitis B surface Antigen; HCV: Hepatitis C virus; AIP: Autoimmune pancreatitis; CT: Computed Tomography
Introduction
IgG4-related disease (IgG4-RD) represents a fibroinflammatory immune-mediated condition that might affect several organs. It is a complex disease with highly variable clinical manifestations, that can mimic countless other inflammatory and neoplastic conditions, and with a characteristic histopathological appearance. Its pathophysiology remains unclear, although recent researches suggest the existence of an antigenic trigger, starting and also perpetuating the disease [1]. Common features of IgG4-RD include multiple organs involvement, causing tumor-like swellings, fibrosis, tissue infiltration, and a classic pathological form of storiform lesions [2]. We report a clinical case of IgG4-RD with special futures about the challenges in the diagnosis and how that impacts on the clinical course of the disease.
Case report
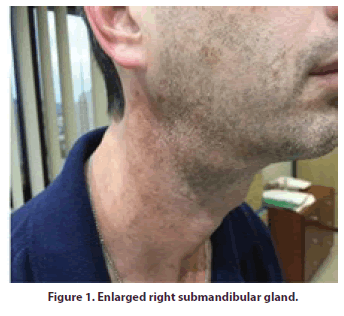
A 44-years-old male, proceeding of Joinville/ Santa Catarina, comes to rheumatological interview on August 2nd, 2017 referred from the otorhinolaryngologist due to submandibular glands hypertrophy (Figure 1) associated with a positive rheumatoid factor.
His medical history from November 2016 showed that he started experiencing urinary symptoms, such as pollakiuria, terminal drip, and weak jet, when he decided to see a urologist and was medicated only with symptomatic and released without a diagnosis.
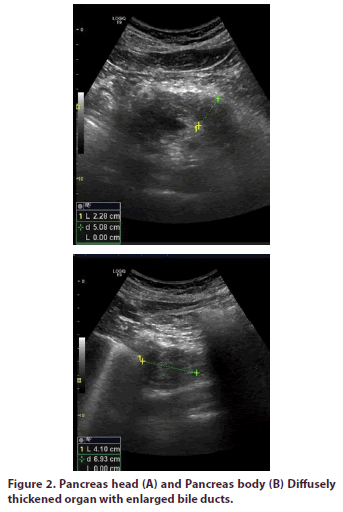
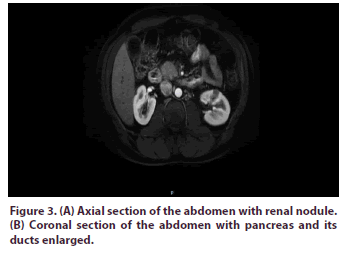
Still, in 2016, he presented diffuse abdominal pain, diarrhea, jaundice, choluria, acholia, and weight loss, undergoing hospitalization for investigation. December 2016 hospitalization exams showed: amylase 43 U/L, ferritin 815 mg/ml, glucose 202 mg/dl, SGOT 133 U/L, SGPT 354 U/L, GGT 312 U/L, total bilirubin 5,4 mg/ dl, conjugated bilirubin 4,4 mg/dl and unconjugated 1,0 mg/dl, ALP 271 U/L, CRP 17,8 mg/dl (normal reference value of <10 mg/dl), urine was normal, creatinine 0,84 mg/dl, urea 35 mg/dl. The investigation proceeded with an abdomen Ultrasonography (Figure 2), which demonstrated a diffusely thickened pancreas with enlarged bile ducts, and an abdomen Nuclear Magnetic Resonance (Figure 3), that showed a thickened pancreas with dilated intrahepatic and extrahepatic bile ducts, thickening of choledochal above pancreas head, with subsequent abrupt reduction, in addition to renal nodules.
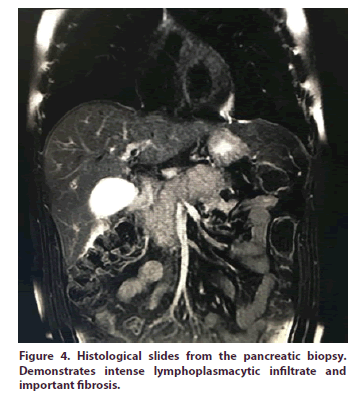
In the face of the image findings, pancreatic neoplasm was raised as a primary diagnosis hypothesis and the patient was submitted to a laparotomy. An enteroanastomosis (hepatojejunoanastomosis) was performed as well as cholecystectomy and biopsies. The anatomopathological’ results showed that the gallbladder presented fibrous thickening of the wall, with moderate muscle hypertrophy and diffuse mono and polymorphonuclear inflammatory infiltration, rich in eosinophils, consistent with chronic cholecystitis. In colledochus, dense fibrosis and lymphocyte infiltration permeated by plasma cells and diffuse polymorphonuclear, related to a chronic inflammatory process, was observed. Pancreas biopsy (Figure 4) demonstrated extensive fibrosis, with marked lymphoplasmacytic, polymorphonuclear, and fibrosis inflammatory infiltration, consistent with chronic pancreatitis. After the procedure, the patient evolved with an improvement in his condition and resolution of symptoms. At that time he was medicated only with analgesics and anti-inflammatories.
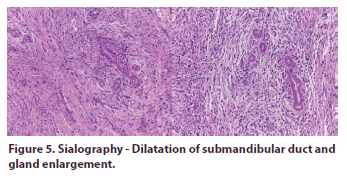
In June 2017 he presented an increase in the volume of submandibular regions, when he consulted an otorhinolaryngologist. A sialography (Figure 5) was performed and showed the duct of the right submandibular gland with a slightly dilated diameter throughout, besides an increase in glandular volume. After finding a positive rheumatoid factor in laboratory tests, the patient was referred to a rheumatologist. He was being treated for diabetes mellitus and dyslipidemia using sitagliptin 50 mg/day, metformin 500 mg/ day, and simvastatin 20 mg/day. He denied other symptoms, alcoholism, and smoking. As a background, he had been submitted to splenectomy for traumatic rupture of the spleen in an automobile accident. On physical examination, only an increase in the submandibular glands was observed. Cardiorespiratory apparatus without abnormalities. Abdomen with a scar, normotensive, painless, and without palpable masses.
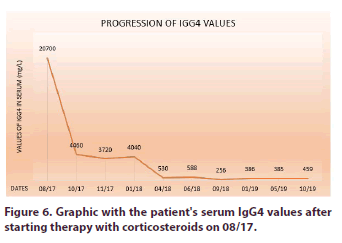
Laboratory tests were requested and showed the following results: rheumatoid factor 34, IgG3 544 mg/L, IgG2 5.110 mg/L, IgG1 10.600 mg/L, IgG4 20.700 mg/L (RV< 201 mg/L), Erythrocyte Sedimentation Rate (ESR) 87 mm/H, SGOT 108 U/L and SGPT 172 U/L, hemoglobin (Hb) 13,6 g/dL and hematocrit (Ht) 42.4%, Leukocytes 8173/uL and Platelets 424.800/uL, urine was normal and creatinine 0.71 mg/dL. Research of Anti-nuclear factor (ANF), Ro Antibodies and La Antibodies, Hepatitis B surface antigen (HBsAg), and hepatitis C virus (HCV) were non-reactive. At this time, the diagnosis of IgG4-related disease was considered and prednisone 40 mg was initiated. The patient had a gradual decrease in the salivary glands. A gradual taper of prednisone was performed with a significant drop of IgG4, coming close to normal values (Figure 6), resolution of clinical symptoms and significant reduction of the submandibular glands, when prednisone was discontinued.
Figure 6: Graphic with the patient's serum IgG4 values after starting therapy with corticosteroids on 08/17.
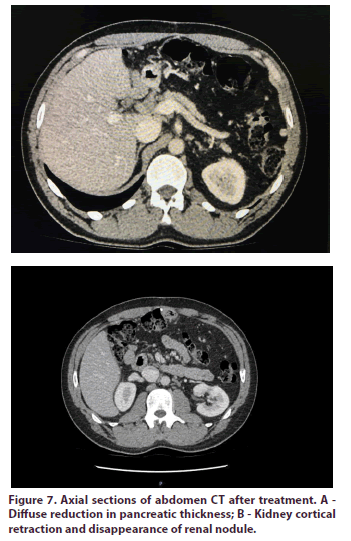
An abdominal CT was requested (Figure 7), which found a diffuse reduction in the thickness of the pancreas and virtual disappearance of renal nodules, but with new regions of cortical retraction that suggested fibrous scarring alterations. After 2 months the patient presented a worsening condition, with the salivary glands resurfacing. Salivary Ultrasonography was requested and showed diffuse sialadenitis, and prednisone 10 mg per day was started again. The patient had a further reduction of the glands, with no significant increase in IgG4.
Discussion
The spectrum of IgG4-RD is not fully understood and, nowadays, this disease is generally considered to be a rare condition, although its true epidemiology has not yet been completely clarified 1. The pathogenesis of this disorder is also unknown, but it shows that the disease has an autoimmune character, with an important role for cells TCD4 + and T-follicular (Tfh) helper cells and that IgG4 antibodies are not exactly pathogenic. Several self-antigens have been listed and had more than one antigen that is plausible and likely to trigger this condition [3]. It’s known that IgG4 is the least common among the four IgG classes, corresponding to 3-6% of the total. These molecules are not able to activate a classic complement pathway, making them unlikely to activate immune responses. When they bond with the Fc part of other circulating filters, they have an antiinflammatory and protective action against allergic reactions4. Like most diseases mediated by the immune system, it probably has immunological triggers, such as chemicals and infectious agents. Besides, studies on genetics and epigenetics influence are being carried out to better understand these pathogenic variables of the disease [4].
Tissue fibrosis characterized by massive infiltration of lymphocytes, the most objective manifestation of the disease, is related to the action of interleukin IL-1, Tumor Growth Factor-beta (TGF-b) and interferongamma, developed in the inflammatory cascade. It is important to note that IgG4-RD is not mediated by type 1 T helper lymphocytes, like most immunological diseases [4]. This inflammatory cascade stimulates IgG4 secretion, resulting in elevated serum levels. It also causes eosinophilia and increased serum IgE. Approximately 50% of patients with increased IgG4 have eosinophilia in the peripheral blood. However, it is not known whether the fibrous damage typical of the disease is caused by excess IgG4 or if this increase is only a consequence of the inflammatory cascade, with no direct relationship with tissue damage. Another important aspect is the production of IgG4 molecules with unique characteristics. One of these characteristics is the instability in bonding with antigens, being unable to cross-link with each other, which makes it impossible for these molecules to activate the classic complement pathway, resulting in limitation of immune activation in general [4].
The clinical manifestations of IgG4-RD are extremely diverse. Patients are usually asymptomatic at the time of diagnosis and do not have a fever. However, those with multiple organ disease lose approximately 9 to 14 kg over months, until the correct diagnosis is made [3]. Single or multiple organs may be involved in IgG4-RD. The presentation is usually subacute with the development of a localized mass or nodule, commons places are in the orbit, kidney, and lung, or diffuse enlargement of an organ, such as the pancreas. Takeuchi et al. (2014) and Sah et al. (2010) reported the involvement of multiple organs in 60-90% of patients with disorders related to IgG4 [5,6]. There is a great diversity of symptoms, which can be mild and very common to other diseases, or severe disorders, such as severe insufficiency of multiple organs due to the disseminated fibrosis that occurs in the natural course of the disease. Constitutional symptoms such as fever, weight loss, anorexia, and nighttime sweating may also be present. Approximately 30% of patients have a history of atopies, such as asthma, atopic dermatitis, nasal polyps, and allergic rhinitis. Those who do not have this characteristic, have an IgE serum increase [4]. Initially, the most affected organ is the pancreas, occurring with the damage to the bile duct. It results in autoimmune pancreatitis (AIP) type 1 associated with sclerosing cholangitis [4]. The involvement of salivary glands or sclerosing sialodenite, as a combination of enlarged lacrimal, parotid and submandibular glands (Mikulicz's disease), may be part of the disease. The orbital disease, with edema, proptosis, dacryoadenitis or orbital pseudotumor, is also often seen. Retroperitoneal fibrosis is frequent, affecting the ureters and leading to hydronephrosis and kidney damage3. Therefore, autoimmune pancreatitis, sialadenitis, dacryoadenitis, and retroperitoneal fibrosis are the most common characteristics of the disease [4,7].
The IgG4-RD cohorts have a slight predominance of middle-aged and older men. The predilection for older men is very expressive in AIP type 1 (related to IgG4), retroperitoneal fibrosis, IgG4-related tubulointerstitial nephritis and many other organ manifestations.
However, patients with head and neck involvement, in which the higher prevalence in women. The disease is also increasingly associated with children [3].
IgG4-RD can mimic autoimmune rheumatic diseases, such as Sjogren's Syndrome (SS), Systemic Lupus Erythematosus (SLE) and granulomatosis with polyangiitis, and many other conditions. Also, IgG4- RD can overlap on autoimmune diseases, including Antiphospholipid Syndrome and Rheumatoid Arthritis [3]. Besides, there is a relationship between IgG4-RD and an increased chance of malignancies of around 7.4%. The most common neoplasm is B-cell lymphoma of the extranodal zone, which can occur in ocular annexes, salivary glands, and dura mater within 5 years of diagnosis of the disease [4].
Therefore, it is clear that the patient, in addition to fitting the epidemiological profile of the disease, a middleaged man, had a subacute presentation and multiple organ involvement. Initially, he presented with urinary symptoms, probably due to the disease affecting the urinary tract, followed by pancreatic involvement, which is the most affected organ in IgG4-RD. Subsequently, he also showed signs of chronic cholecystitis, enlargement of submandibular glands and nodules, and cortical retractions in the kidneys.
The investigation of IgG4-RD is complex and usually requires a combination of clinical, imaging, histological, and serological tests. However, no single finding is specific for IgG4-RD. Therefore, its diagnosis requires careful interpretation of test results in context with the patient's clinical presentation, as well as the exclusion of a wide variety of differential diagnoses. The dependence of IgG4 levels presents a potential limitation, as these may be within the normal range in a considerable part of patients histologically confirmed to have IgG4-RD [1]. Elevated IgG4 concentrations in the serum and tissue, although typical, are not specific and occur in a reasonable number of diseases, such as recurrent infections, allergic conditions, cystic fibrosis, neoplasms, multicentric Castleman's disease, eosinophilic granulomatosis with polyangiitis (Churg-Strauss), sarcoidosis and other conditions [3]. However, the patient’s clinical and radiological presentation was not compatible with any of these diseases and strongly indicated IgG4-RD.
Laboratory tests usually show CRP and ESR increased, thrombocytosis, anemia, and peripheral eosinophilia. Hypocomplementemia, hypergammaglobulinemia, elevated rheumatoid factor (16-50%) and ANF present (20%) can occur [4]. Typical histopathological findings consist of a triad with lymphoplasmacytic infiltrate, storiform fibrosis, and obliterative phlebitis. Tissue eosinophilia and increased plasma IgG4 increase the correct diagnosis [2].
Therefore, to systematize and facilitate the diagnosis, the Japanese Society of Sjögren's Syndrome, in 2008, approved a criterion, cited by LANG et al. (2016), which bases the diagnosis of IgG4-RD on three factors. The first consists of clinical history and findings of physical examination and imaging tests. The second, in the increase of serum IgG4 values, and, finally, the third, of histopathological findings of lymphoplasmacytic and IgG4 infiltrate, storiform fibrosis, and obliterating phlebitis. If the first two criteria are identified, the patient is classified as a possible carrier of the disease. The presence of the first and third criteria makes the diagnosis probable, and finally, if the patient meets the three criteria mentioned, it is defined as the definitive carrier of IgG4-RD [1].
At the time of diagnosis, in 2017, the criteria mentioned above classified the case reported as possible for IgG4- RD, since the patient did not have the classic findings of storiform fibrosis and phlebitis obliterans on biopsy [1]. However, even with the diagnosis being considered only as possible by this criterion, due to the clinical presentation and the elevation of IgG4 being very suggestive of the diagnosis, treatment with corticosteroids was performed, which showed excellent clinical outcome and reduced IgG4.
In 2019 the Executive Committee of the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR) approved new diagnostic criteria. This new criteria is divided into 3 steps and the diagnosis can be safely established when the patient meets the entry criteria (step 1), does not present any of the exclusion criteria (step 2), and receives a score equal to or greater than 20 in the criteria of inclusion (step 3) [8].
The first step, called entry criteria, must be presented by the patient for the diagnostic to advance. The entry criteria require clinical or radiological evidence of an organ typically affected by the IgG4-RD, such as pancreas, salivary glands, biliary duct, orbit, kidneys, lungs, aorta, retroperitoneum, pachymeninx, or thyroid (Riedel thyroiditis); or pathological evidence of unknown cause of an inflammatory process associated to lymphoplasmacytic infiltrate, typically present in the aforementioned organs [8]. The second step for the diagnostic consists of exclusion criteria- i.e., clinical, radiological, and pathological manifestations that justify another specific disease- which must be verified and excluded. If no exclusion criteria are observed, the diagnostic may advance. Finally, the third step consists of inclusion criteria. There are several of those, and here we mention only the ones presented by the patient in question and their respective number of points: increase in serum IgG4 five times the upper limit of the normal range (11 points); affected a pair of salivary glands (6 points); affected the pancreas and biliary ducts (19 points); low-density areas in the renal cortex, bilaterally (10 points); presence of dense inflammatory infiltrate in the pancreas biopsy (4 points) [8].
When considered the ACR/EULAR diagnostic criteria, the patient is easily diagnosed with IgG4-RD. He presented both entry criteria, no exclusion criteria, and a total of 50 points in the inclusion criteria.
A histopathological review of the same pancreas biopsy slides (Figure 4) was performed, looking for classical evidence of the IgG4-RD. After careful examination, a storiform fibrosis pattern was found in the dense inflammatory infiltrate. However, obliterative phlebitis has not been identified, possibly due to the advanced stage of tissue damage the patient was in. The finding of storiform fibrosis further corroborates the diagnostic.
Regarding the enteroanastomosis that the patient was submitted, the improvement in the symptoms presented after cannot be explained plausibly. The use of only nonsteroidal anti-inflammatory drugs after the procedure would not justify the important clinical improvement obtained. Therefore, this aspect remains unclear in the patient's clinical course.
Early drug intervention is beneficial in most patients, as fibrosis or affected organs become symptomatic in advanced stages. Glucocorticoids are the first-line therapy for remission and prednisone (30-40 mg/day) is recommended as first choice. Patients with mild symptoms may start with lower doses, always with strict clinical follow-up to control effectiveness [9]. Although the majority of the patients respond to glucocorticoid therapy, the reappearance of symptoms is common and the patient's comorbidities may invalidate the treatment [10]. These factors will impact in the duration of the treatment with glucocorticoids, but, generally, it is recommended prednisone for maintenance in low doses, for a period of three years. In most cases, if there is a satisfactory clinical response, the immunosuppression does not exceed six months [9].
However, glucocorticoids sometimes fail to control the disease. Its use has not been fully studied about adverse effects, treatment time, and efficacy in IgG4- RD. Also, the side effects usually make treatment with glucocorticoids unviable in many patients [9]. In this case, despite the patient having diabetes mellitus, prednisone was still chosen as first-line therapy due to its recognized action in the remission of symptoms, widespread in the literature. The addition of a second immunosuppressive might be necessary sometimes, but that still is a controversial point in literature [9]. Several studies have shown that the addition is beneficial in some patients, such as those where a gradual decrease in glucocorticoid dosage is not possible. Among the possible drugs, rituximab demonstrated the greatest efficacy in remission of the disease. It can be used in association with glucocorticoids, in severe cases, and in monotherapy, when the use of glucocorticoids is not indicated. Azathioprine, mycophenolate mofetil, 6-mercaptopurine, methotrexate, tacrolimus, and cyclophosphamide have not demonstrated superior efficacy to glucocorticoids in prospective studies and need further researches [9,11]. In the future, therapeutic options may be directed towards the use of anti-fibrotic agents and anti-CD4 + T lymphocytes with cytotoxic activity, with are implicated in the pathogenesis of IgG4-RD, however, these options are incipients and need further research [10].
Cases of reoccurrence or refractory to corticosteroids are not rare, and when those occur, a new course of treatment with glucocorticosteroids can be employed. The reoccurrence of the clinical picture can be accompanied or not by an increase of serum IgG4 levels, since it shows low specificity – i.e., they also increase due to other conditions. A study published in 2015 showed that plasmablasts, which are between activated B cells and plasmatic cells, seem to be better activity markers of IgG4-RD than IgG4 levels. Hence, the serum IgG4 levels do not seem to accurately determine the moment to restart treatment [12]. As such, the small increase of IgG4 after the treatment, presented by our patient, when compared to the initial levels, was not considered as an indication to restart treatment since the clinical symptoms regressed.
Conclusion
IgG4-RD is an important disease due to the spectrum of clinical presentations. The symptoms can be considerably distinct and point to different diagnoses, making the recognition of this disease a challenge for the physician who is not prepared to considering the clinical picture in a syndromic way, especially in those patients with normal IgG4 values. This implies in the patient's clinical outcome, since the lack of treatment or the delay in the beginning of adequate therapy, can lead to irreversible fibrosis and loss of organ function. In this case, the diagnosis was done after years of the initial manifestations, and with the correct treatment, the patient experienced a great improvement in the symptoms. Therefore, this report is important to add knowledge about this disease and to encourage clinical experience in the early diagnosis and management of these patients, avoiding unnecessary interventions and progression of the symptoms.
Acknowledgments
The authors would like to acknowledge the team at the Specialized Center for Diagnosis, Assistance and Prevention (CEDAP) of Joinville for their willingness and support to the authors in the construction of this report.
Funding source
None to report.
Disclosure of conflict of interest
No conflict of interest.
References
- Lang D, Zwerina J, Pieringer H. IgG4-related disease: current challenges and future prospects. Ther. Clin. Risk. Manag. 12, 189-199 (2016).
- Al-Mujaini A, Al-Khabori M, Shenoy K et al. Immunoglobulin G4-Related Disease: An Update. Oman. Med. J. 33(2), 97-103 (2018).
- https://www.uptodate.com/contents/pathogenesis-and-clinical-manifestations-of-igg4-related-disease
- Vasaitis L. IgG4-related disease: a relatively new concept for clinicians. Eur. J. Intern. Med. 27, 1-9 (2016).
- Takeuchi M, Sato Y, Ohno K et al. T helper 2 and regulatory T-cell cytokine production by mast cells: a key factor in the pathogenesis of IgG4-related disease. Mod. Pathol. 27(8), 1126-1136 (2014).
- Sah R, Chari S, Pannala R et al. Differences in Clinical Profile and Relapse Rate of Type 1 Versus Type 2 Autoimmune Pancreatitis. Gastroenterology. 139(1), 140-148 (2010).
- Kamisawa T, Zen Y, Pillai S et al. IgG4-related disease. The Lancet. 385(9976), 1460-1471 (2015).
- Wallace Z, Naden R, Chari S et al. The 2019 American College of Rheumatology/European League Against Rheumatism Classification Criteria for IgG4-Related Disease. Arthritis. Rheum. 72, 7-19 (2020).
- Khosrosahi A, Wallace ZS, Crowe JL et al. International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis. Rheum. 67(7), 1688-1699 (2015).
- Cory P, Stone J. Current and Future Approaches to the Treatment of IgG4-related disease. Zeitschrift. Für. Rheumatologie. 75(7), 681-686 (2016).
- Pieringer H, Parzet I, Wohrer A et al. IgG4-related disease: an orphan disease with many faces. Orphanet. J. Rare. Dis. 9(1), 110 (2014).
- Wallace Z, Mattoo H, Carruthers M et al. Plasmablasts as a biomarker for IgG4-related disease, independent of serum IgG4 concentrations. Ann. Rheum. Dis. 74(1), 190-195 (2015).