Mini Review - Interventional Cardiology (2022) Volume 14, Issue 0
Gender differences on outcomes in left atrial appendage closure: An update
- Corresponding Author:
- Caroline Kleinecke
Department of Cardiology,
Klinikum Hochrhein,
Waldshut-Tiengen,
Germany,
E-mail: carolinekleinecke@web.de
Received date: 21-Dec-2021, Manuscript No. FMIC-21-48871; Editor assigned: 23-Dec-2021, PreQC No. FMIC-21-48871 (PQ); Reviewed date: 03-Jan-2022, QC No. FMIC-21-48871; Revised date: 06-Jan-2022, Manuscript No. FMIC-21-48871 (R); Published date: 13-Jan-2022, DOI: 10.37532/1755-5310.2022.14(s8).179
Abstract
Left Atrial Appendage Closure (LAAC) is an alternative to Oral Anticoagulation (OAC) for stroke prevention in selected patients with Atrial Fibrillation (AF). According to current guidelines, this procedure is recommended for patients with contraindications to OAC, prior bleeds, or an elevated bleeding risk. Growing evidence shows that LAAC provides stroke prevention comparable to OAC. Additionally, a notable reduction of bleeding events and its associated mortality is achieved by LAAC. Women with AF have an increased risk for ischemic strokes and compared to male patients strokes tend to be more severe. However, due to concerns of bleeding in elderly women, underuse or underdosing of OAC is often observed in females. Therefore, women may have an increased benefit from LAAC. Gender differences have been described in other cardiac interventions and especially periprocedural complications occur more often in women. Recent studies have analyzed gender disparities of large, multicenter and realword registries in patients undergoing LAAC with respect to patient selection, device utilization, as well as periprocedural and clinical outcomes. In this mini-review, we summarize the results of those studies.
Keywords
Gender • Left atrial appendage closure • Atrial fibrillation • Stroke prevention
Introduction
Atrial Fibrillation (AF) is the most common rhythm disorder in the aging population. It substantially increases the risk for cognitive decline, heart failure, stroke, disability, and overall mortality [1].
Gender-related differences have been reported with regard to epidemiology, etiology and outcomes of patients suffering from AF. Its incidence increases after the age of 50 years in males and after 60 years in females and at an age of 90 years the lifetime risk is similar for both genders [2]. Women with AF tend to have a higher incidence of hypertension, heart failure with preserved ejection fraction and valvular heart disease, whereas ischemic heart disease is more prevalent in men [3].
About 20%-30% of ischemic strokes are caused by cardio-embolic events from the Left Atrial Appendage (LAA) due to AF [1]. In this context, females are at increased risk for stroke and AF-related strokes tend to be especially severe in women. Smaller diameters of intracranial arteries in females are considered a major reason for this observation. Cardiac emboli usually lead to more proximal vessel occlusions in women [4].
To prevent LAA thrombi with subsequent cardio-embolic stroke, OAC is the standard of care. In selected patients, LAAC is non-inferior to OAC for with regard to stroke prevention. By obviating OAC, it additionally reduces bleeding events, resulting in a superiority regarding cardiovascular and overall mortality.
In cases of percutaneous coronary intervention or transcatheter aortic valve implantation, higher rates of severe procedural complications were observed in women [5,6]. Only recently, several studies have compared clinical outcomes between male and female gender in patients undergoing LAAC (Table 1) [7-12]. The present concise review will highlight the principal findings of the contemporary studies in the field.
| Study | No. of pts | Female gender | Age (years, females vs. males) | CHA2DS2-VASc score (points, female vs. males) | Device | Successful device implantation (females vs. males) | Periprocedural adverse events (females vs. males) | Length of hospital stay (days, females vs. males) | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| Single registry-Coburg hospital (Mahnkopf, et al. [7]) | 209 | 43% | 79.6 ± 6.4 vs. 77.0 ± 7.9, p=0.01 | 4.7 vs. 4.1, p=0.001 | Watchman | 98.8% vs. 96.2, n.s. | 16.4% vs. 12.7, n.s. | Not reported | Quality of life 3 months after LACC: Significant improvement in health state, mobility, self-care and usual activities in females |
| LAARGE registry (Kleinecke, et al. [8]) | 641 | 39% | 76.4 ± 8.2 vs. 75.6 ± 7.7, p=0.42 | 4.9 ± 1.5 vs. 4.3 ± 1.5, p<0.001 | Watchman Amplatzer Occlutech | 98.4% vs. 97.2%, p=0.33 | 6.9% vs. 3.1%, p=0.03 | Not reported | 1-year follow-up: All-cause stroke 0.5% vs. 1.3%, p=0.65 Severe bleeding: 0.0% vs. 1.0%, p=0.29 All-cause mortality: 9.2% vs. 13.1%, p=0.14 |
| Amplatzer Amulet Observational Study (de Caterina, et al. [9]) | 1,088 | 35% | 76.2 ± 7.9 vs. 74.6 ± 8.7, p=0.01 | 4.7 ± 1.5 vs. 3.9 ± 1.6, p<0.0001 | Amplatzer Amulet | 99.5% vs. 99.2, p=0.65 | 6.5% vs. 5.4%, p=0.50 | 3.0 ± 5.5 vs. 2.1 0 ± 2.7, p=0.03 | 2-year follow-up: Combined endpoint of ischemic stroke, systemic embolism, or cardiovascular death: 12.5% vs 12.0%, p=0.82 Device-related thrombus: 1.6% vs 1.6%, p=0.96 Major bleeding: 7.6% vs 7.1, p=0.69 |
| US National Inpatient Sample (Ranka, et al. [10]) | 3,210 | 38% | Not reported | Not reported | Not reported | Not reported | Not significant (incl. death, bleeding, acute kidney injury, cardiogenic shock, and respiratory failure) | Not reported | Not reported |
| US readmission database (Osman, et al. [11]) | 9,281 | 39% | 77 (72-82) vs. 76 (71-81), p<0.01 | 5 (4-6) vs. 4 (3-5), p<0.01 | Not reported | Not reported | 2.9% vs. 1.7%, p<0.01 | Non-home discharge: 11.4% vs. 6.7%, p<0.01 | 30-day readmission rate: 10% vs. 8.6%, p=0.03 |
| US National Cardiovascular Data Registry (Darden, et al. [12]) | 49,357 | 41% | 76.5 ± 7.9 vs.75.8 ± 8.2, p<0.001 | 5.3 ± 1.5 vs. 4.5 ± 1.4, p<0.001 | Watchman | Canceled procedure 3.0 vs. 2.0, p=0.66 | 4.1% vs. 2.0%, p<0.001 | Hospital stay>1 day: 16% vs. 1.6%, p<0.001 | Not reported |
Abbreviations: LAAC: Left Atrial Appendage Closure; US: United States
Table 1: Registries comparing gender differences in patients undergoing LAAC.
Literature Review
Coburg left atrial appendage occlusion registry
The Coburg Left Atrial Appendage Occlusion (COLA) registry enrolled 201 (43% females) consecutive patients from October 2016 to March 2018. Quality of life was assessed with the EQ- 5D questionnaire in all patients before and three months after the procedure. Before LAAC, females had a higher score for anxiety/ depression, while other parameters of the EQ-5D were comparable between the groups. Three months after the intervention, women had a significant improvement in health state, mobility, selfcare and daily activities. In contrast, in men all scores remained unchanged [7].
Left atrial appendage occlusion registry Germany
The prospective, multicenter Left Atrial Appendage Occlusion Registry (LAARGE) included 638 patients (39% females) who underwent LAAC from July 2014 to January 2016 in 38 hospitals in Germany. Females were older and had a higher stroke risk. Conversely, males suffered more often from coronary artery and vascular disease. Technical success was high and similar for both genders (98.4%: Females vs. 97.2%: Males, p=0.33). Severe periprocedural complications (6.9% vs. 3.1%, p=0.032) occurred more often in females due to a higher rate of severe bleedings and pericardial effusion or cardiac tamponade in this group. After one year, the rates of all-cause stroke (0.5% vs. 1.3%, p=0.65), severe bleeding (0.0% vs. 1.0%, p=0.29) and one-year all-cause mortality (9.2% vs. 13.1%, p=0.14) were comparable between both genders [8].
Amplatzer amulet observational study
1,088 (35% females) AF patients were enrolled in the prospective, multicenter, Amplatzer Amulet Observational Study and followed for 2 years. Implant success was similar between women and men (99.5%: Females vs. 98.9%: Males, p=0.58). At 2 years, the primary outcome of ischemic stroke, systemic embolism, or cardiovascular death (12.5% vs. 12.0%, p=0.82) was comparable between the groups. However, compared to the CHA2DS2-VASc score predicted rates, a numerically greater absolute risk reduction of ischemic stroke was observed in women (from 7.6 to 2.1%/ year) than men (from 6.2 to 2.2%/year). The rates of devicerelated thrombus were equal (1.6% vs. 1.6%, p=0.96) between the groups. Finally, no differences in terms of periprocedural or long-term (7.1 vs. 7.6%/year) major bleeding were observed [9].
United States national inpatient sample registry
Ranka, et al. identified 3,210 patients (38% females) from the US National Inpatient Sample (NIS), who underwent LAAC between January 2012 and September 2015. The rates of periprocedural adverse events, including blood transfusion, post-operative bleeding, acute kidney injury, acute respiratory failure and mechanical ventilation, multiorgan failure, cardiogenic shock and arrest, cardiac complications, as well as periprocedural mortality were comparable between women and men [10].
United States national readmission database
In the US National Readmission Database (NRD) a total of 9,281 patients (39% females) underwent LAAC from October 2015 to December 2017. In this cohort, women were older and had a lower prevalence of diabetes mellitus, heart failure, vascular disease, as well as renal failure. Furthermore, they had a higher prevalence of obesity and history of stroke and their stroke risk was higher. After propensity-score matching for all relevant baseline criteria, a higher rate of major in-hospital adverse events (2.8%: Females vs. 1.9%: Males, p<0.001) was observed in females, which was driven by pericardial (1.8% vs. 1.0%, p<0.001) and vascular complications (1.6% vs. 1.0%, p<0.001). In the logistic regression analysis, female sex and chronic heart failure were independent predictors for worse major in-hospital adverse events. Additionally, surrogates of severe disability (mechanical ventilation (1% vs. 0.4%, p<0.001) and non-home discharges (11.3% vs. 6.9%, p<0.01)) were more often documented in women. Also, the median costs of hospitalization were higher in this group (25,208$ vs. 24,845$, p<0.001). Finally, 30-day readmission rate was higher among women (10% vs. 8.6%, p=0.03) [11].
United States national cardiovascular data registry
A total of 49,357 patients (41% females), who underwent Watchman (Boston Scientific, Marlborough, MS, USA) implantation between January 2016 and December 2018, were enrolled in the US National Cardiovascular Data Registry (NCDR). Women were older and had a greater stroke risk. Furthermore, they had a higher prevalence of paroxysmal AF, prior stroke and uncontrolled hypertension. Conversely, but consistent with other studies, the prevalence of congestive heart failure, diabetes, and coronary artery disease was higher in men. The rate of aborted or cancelled procedures was comparable between the groups. After multivariable adjustment, women were more likely to experience any complication (6.3%: Females vs. 3.9%: Males, p<0.001) and major adverse events (4.1% vs. 2.0%, p<0.001) due to pericardial effusion requiring drainage (1.2% vs. 0.5%, p<0.001) or major bleeding (1.7% vs. 0.8%, p<0.001). Although death was rare and absolute differences were minimal, women had an increase in the risk of in-hospital death (0.3% vs. 0.1%, p<0.001). Finally, women were hospitalized longer than men (stay longer than 1 day: 16.0% vs. 11.6%, p<0.00) [12].
Discussion
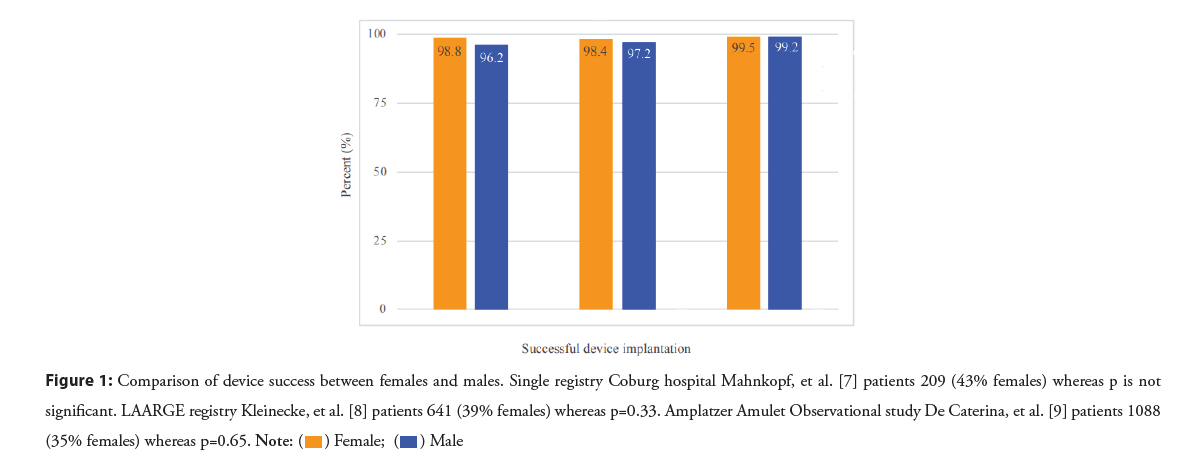
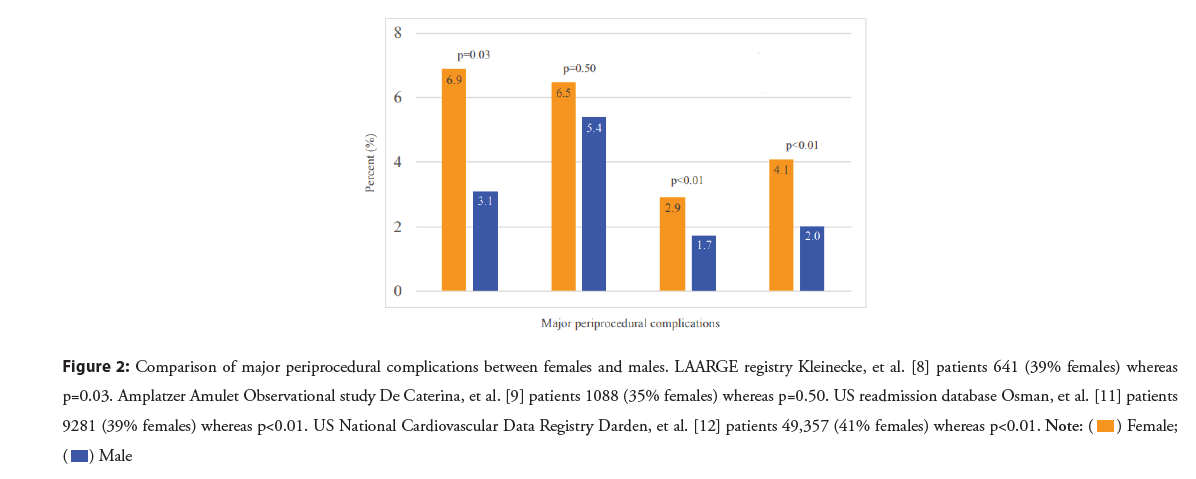
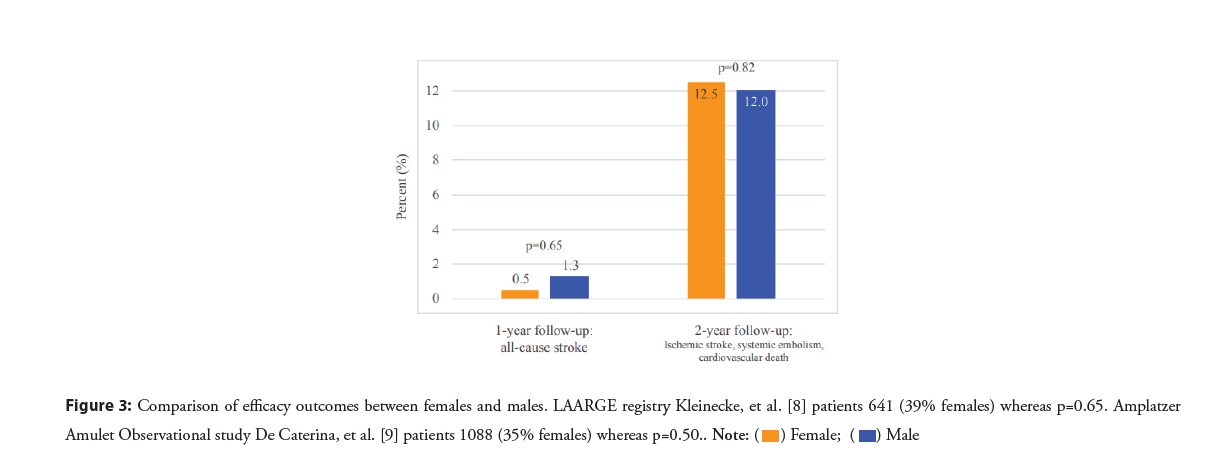
LAAC is an effective and safe option for stroke prevention in both genders. Observations of a single center registry indicate a higher quality of life in women after LAAC compared to their male counterparts. However, LAAC seems to be performed less often in females. The reasons for this observation remain unclear and should be addressed in future research. Women undergoing LAAC are typically older and have a higher stroke risk. In contrast, men suffer more often from diabetes mellitus, coronary artery disease, and heart and renal failure. Successful device implantation is achieved equally in both genders (Figure 1). However, periprocedural complications occur more often in females (Figure 2), mainly due to pericardial effusion or cardiac tamponade, vascular complications as well as severe bleedings. This may be due to inappropriate device sizing and the stiffness of dedicated sheaths and devices in combination with thinner and more fragile LAAs of women. As a consequence, both delivery sheaths as well as occluder devices should be adapted to the smaller body size, smaller vessel diameter and fragile tissue of left atrial appendages in women. A higher percentage of periprocedural complications leads to longer hospital stays and increased costs. However, in the long-term the rates of all-cause stroke, systemic embolism, bleeding events, and cardiovascular/unexplained death do not differ (Figure 3). Also, the rate of device-related thrombus seems to be comparable between the genders.
Figure 1: Comparison of device success between females and males. Single registry Coburg hospital Mahnkopf, et al. [7] patients 209 (43% females) whereas p is not significant. LAARGE registry Kleinecke, et al. [8] patients 641 (39% females) whereas p=0.33. Amplatzer Amulet Observational study De Caterina, et al. [9] patients 1088 (35% females) whereas p=0.65. 
Figure 2: Comparison of major periprocedural complications between females and males. LAARGE registry Kleinecke, et al. [8] patients 641 (39% females) whereas p=0.03. Amplatzer Amulet Observational study De Caterina, et al. [9] patients 1088 (35% females) whereas p=0.50. US readmission database Osman, et al. [11] patients 9281 (39% females) whereas p<0.01. US National Cardiovascular Data Registry Darden, et al. [12] patients 49,357 (41% females) whereas p<0.01.

Conclusion
Compared to their male counterparts, women undergoing left atrial appendage closure seem to be at higher risk for periprocedural complications. This leads to prolonged hospital stays and increased costs. However, in the long-term similar efficacy and safety outcomes with reduction of all-cause stroke and bleeding events are observed for both genders.
Funding
N/A
Conflict of Interest
Bernhard Meier is a consultant to Abbott. Steffen Gloekler has received grants to the Institution from Abbott and has received a grant from the Swiss Heart Foundation.
References
- Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 42(5): 373-498 (2021).
[Crossref] [Google Scholar] (All versions) [Pubmed]
- Magnussen C, Niiranen TJ, Ojeda FM, et al. Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts: Results from the BiomarCaRE consortium (Biomarker for cardiovascular risk assessment in Europe). Circulation. 136(17): 1588-1597 (2017).
[Crossref] [Google Scholar] [Pubmed]
- Lip GY, Laroche C, Boriani G, et al. Sex-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: A report from the Euro Observational Research Programme Pilot survey on Atrial Fibrillation. Europace. 17(1): 24-31 (2015).
[Crossref] [Google Scholar] (All versions) [Pubmed]
- Lang C, Seyfang L, Ferrari J, et al. Do women with atrial fibrillation experience more severe strokes? Results from the Austrian stroke unit registry. Stroke. 48(3): 778-780 (2017).
[Crossref] [Google Scholar] [Pubmed]
- Potts J, Sirker A, Martinez SC, et al. Persistent sex disparities in clinical outcomes with percutaneous coronary intervention: Insights from 6.6 million PCI procedures in the United States. PLoS One. 13(9): e0203325 (2018).
[Crossref] [Google Scholar] [Pubmed]
- Chandrasekhar J, Dangas G, Yu J, et al. Sex-based differences in outcomes with transcatheter aortic valve therapy: TVT Registry From 2011 to 2014. J Am Coll Cardiol. 68(25): 2733-2744 (2016).
[Crossref] [Google Scholar] [Pubmed]
- Mahnkopf MC, Marcel M, Johannes B, et al. Left atrial appendage closure: Are men and women equal? Results from the Coburg LAA occlusion register. J Am Coll Cardiol. 73(S9): (2015).
- Kleinecke C, Lewalter T, Sievert H, et al. Interventional occlusion of left atrial appendage in patients with atrial fibrillation. Gender-related outcomes in the German LAARGE Registry. J Cardiovasc Electrophysiol. 32(10): 2636-2644 (2021).
[Crossref] [Google Scholar] [Pubmed]
- de Caterina AR, Nielsen-Kudsk JE, Schmidt B, et al. Gender difference in left atrial appendage occlusion outcomes: Results from the Amplatzer amulet observational study. Int J Cardiol Heart Vasc. 35: 100848 (2021).
[Crossref] [Google Scholar] [Pubmed]
- Ranka S, Acharya P, Sami F, et al. Effect of sex and race on outcomes after left atrial appendage occlusion: A report from national inpatient sample. J Am Coll Cardiol. 75(S11): 529 (2020).
- Osman M, Patel B, Munir MB, et al. Sex-stratified analysis of the safety of percutaneous left atrial appendage occlusion. Catheter Cardiovasc Interv. 97(5): 885-892 (2021).
[Crossref] [Google Scholar] (All versions) [Pubmed]
- Darden D, Duong T, Du C, et al. Sex differences in procedural outcomes among patients undergoing left atrial appendage occlusion: Insights from the NCDR LAAO registry. JAMA Cardiol. 6(11): 1275-1284 (2021).
[Crossref] [Google Scholar] [Pubmed]