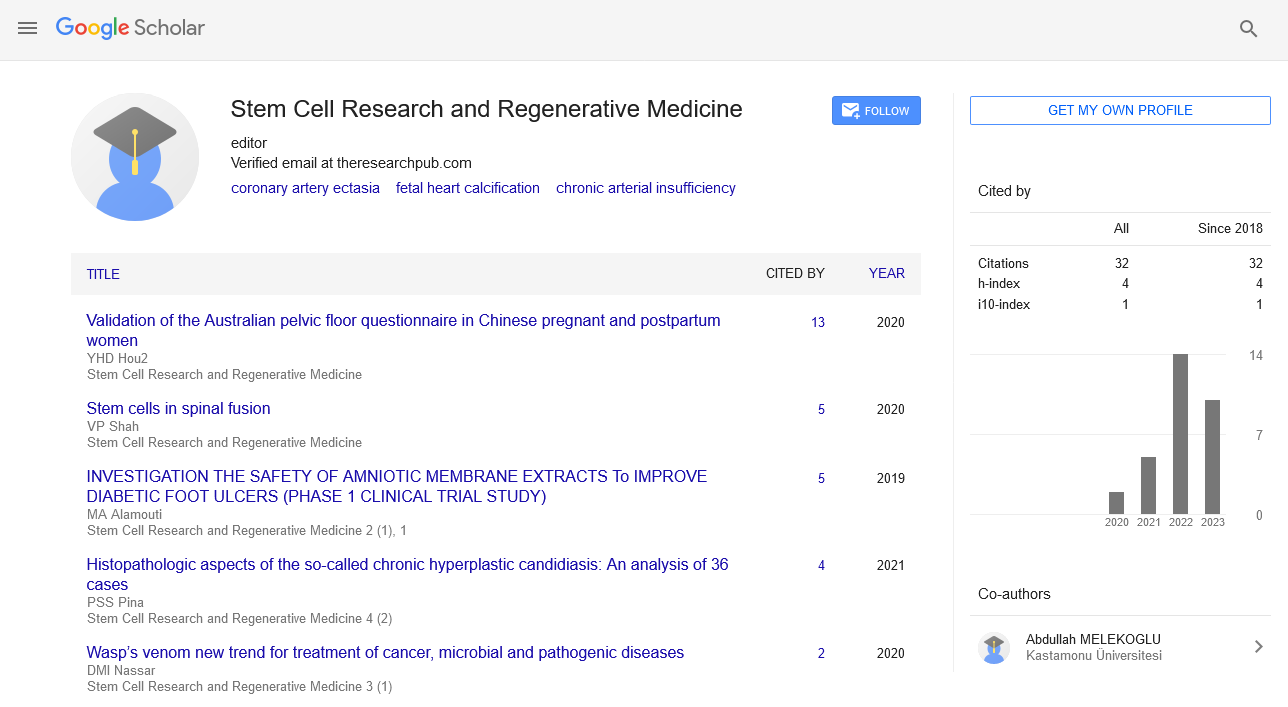
Perspective - Stem Cell Research and Regenerative Medicine (2024) Volume 7, Issue 4
Hematopoietic Stem Cells: The Foundation of Blood Formation
- Corresponding Author:
- Thomas Greb
Department of Stem Cells and Regenerative Medicine Division,
Garvan Institute of Medical Research,
384 Victoria Street,
Darlinghurst,
NSW 2010,
Australia
E-mail: ThomasGreb@ucla.edu
Received: 26-Jul-2024, Manuscript No. SRRM-24-145830; Editor assigned: 29-Jul-2024, Pre QC No. SRRM-24-145830 (PQ); Reviewed: 12-Aug-2024, QC No. SRRM-24- 145830; Revised: 21-Aug-2024, Manuscript No. SRRM-24-145830 (R); Published: 28-Aug-2024, DOI: 10.37532/SRRM.2024.7(4).244-246
Introduction
Hematopoietic Stem Cells (HSCs) are a rare population of cells responsible for the continuous production of all blood cells throughout an individual’s life. They are found primarily in the bone marrow but also circulate in the peripheral blood. HSCs are essential for maintaining the body’s hematopoietic system, which includes red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes). The unique ability of HSCs to self-renew and differentiate into various blood cell lineages makes them a critical focus of research and clinical applications, particularly in the treatment of blood-related diseases. This essay explores the biology of HSCs, their role in health and disease, and their significance in regenerative medicine.
Description
Biology of hematopoietic stem cells
HSCs are multipotent stem cells that can differentiate into all types of blood cells. They are defined by their ability to both self-renew, producing identical copies of themselves, and differentiate into progenitor cells that give rise to the various lineages of blood cells. The balance between selfrenewal and differentiation is tightly regulated by a complex network of intrinsic factors, such as transcription factors and epigenetic modifications, as well as extrinsic factors from the bone marrow microenvironment, or “niche.”
Self-renewal and differentiation
Self-renewal is the process by which HSCs divide to produce more stem cells, ensuring the longterm maintenance of the stem cell pool. This process is crucial for the lifelong production of blood cells. Differentiation, on the other hand, involves the progression of HSCs into committed progenitor cells that eventually become mature blood cells. The first step in differentiation is the division of HSCs into either Common Myeloid Progenitors (CMPs) or Common Lymphoid Progenitors (CLPs). CMPs give rise to erythrocytes, platelets, granulocytes, and monocytes, while CLPs differentiate into lymphocytes, including T cells, B cells, and natural killer cells.
The decision between self-renewal and differentiation is influenced by several signaling pathways, including the Notch, Wnt, and Hedgehog pathways, as well as interactions with the bone marrow niche. The niche consists of various cell types, such as osteoblasts, endothelial cells, and mesenchymal stem cells, which provide signals that regulate HSC behavior. For instance, osteoblasts are known to secrete factors like Thrombopoietin (TPO) and Stem Cell Factor (SCF) that promote HSC maintenance and self-renewal.
Role of hematopoietic stem cells in health
HSCs are essential for the ongoing replenishment of blood cells, which have limited lifespans and must be constantly replaced. Red blood cells, for example, have a lifespan of about 120 days, while neutrophils, a type of white blood cell, survive for only a few days. The ability of HSCs to produce billions of new blood cells daily is vital for maintaining normal physiological functions, including oxygen transport, immune response, and blood clotting.
In addition to their role in normal blood production, HSCs are also involved in the body’s response to injury or infection. During times of stress, such as infection, blood loss, or inflammation, HSCs can increase the production of specific blood cell types needed to address the immediate threat. This process, known as “emergency hematopoiesis,” involves the rapid proliferation and differentiation of HSCs to replenish depleted cell populations.
Hematopoietic stem cells in disease
Dysregulation of HSC function can lead to various hematological disorders. These can be broadly classified into conditions characterized by insufficient blood cell production (cytopenias) or the overproduction of abnormal cells (proliferative disorders).
Hematological malignancies
Hematological malignancies, such as leukemia, lymphoma, and myeloma, arise from mutations in HSCs or their progenitors that lead to uncontrolled cell proliferation and the accumulation of abnormal blood cells. In Acute Myeloid Leukemia (AML), for example, mutations in genes regulating cell differentiation and apoptosis result in the expansion of immature myeloid cells that crowd out normal hematopoiesis, leading to anemia, infection, and bleeding.
Chronic Myeloid Leukemia (CML) is another example where the presence of the BCR-ABL fusion gene, a product of a chromosomal translocation, drives the proliferation of abnormal myeloid cells. Targeted therapies, such as Tyrosine Kinase Inhibitors (TKIs), have revolutionized the treatment of CML by specifically inhibiting the activity of the BCR-ABL protein, allowing for the control of the disease.
Aplastic anemia and bone marrow failure
Aplastic anemia is a condition characterized by the failure of the bone marrow to produce sufficient blood cells, leading to pancytopenia (a reduction in all blood cell types). This can result from the destruction of HSCs by autoimmune mechanisms, exposure to toxic chemicals, radiation, or certain medications. The loss of HSCs in aplastic anemia compromises the body’s ability to maintain normal blood cell levels, leading to severe anemia, increased susceptibility to infections, and bleeding complications.
Bone marrow failure syndromes, such as Fanconi anemia and dyskeratosis congenita, are genetic disorders that impair the function of HSCs. These syndromes often present with pancytopenia and a high risk of developing leukemia, highlighting the critical role of HSCs in maintaining normal hematopoiesis.
Clinical applications of hematopoietic stem cells
The unique properties of HSCs have made them a cornerstone of regenerative medicine, particularly in the context of Hematopoietic Stem Cell Transplantation (HSCT). HSCT is a life-saving procedure used to treat a variety of hematological malignancies, bone marrow failure syndromes, and inherited blood disorders.
Hematopoietic stem cell transplantation
HSCT involves the infusion of healthy HSCs into a patient following high-dose chemotherapy or radiation therapy, which eradicates the diseased bone marrow. The transplanted HSCs then migrate to the bone marrow and reconstitute the patient’s hematopoietic system, producing new, healthy blood cells. There are two main types of HSCT: Autologous and allogeneic transplantation.
Autologous HSCT involves the collection of the patient’s own HSCs prior to treatment, followed by their reinfusion after chemotherapy or radiation. This approach minimizes the risk of Graft-Versus-Host Disease (GVHD), a condition where the transplanted cells attack the recipient’s tissues.
Allogeneic HSCT uses HSCs from a donor, which can be a relative or an unrelated matched donor. This type of transplantation is more commonly used for conditions like leukemia, where the patient’s own HSCs may carry genetic mutations. Allogeneic HSCT carries a higher risk of GVHD but can also offer a “graft-versusleukemia” effect, where the donor immune cells help eliminate residual cancer cells.
Future directions and challenges
While HSCT has been a major therapeutic advance, challenges remain, including finding suitable donors, managing GVHD, and improving outcomes for patients with high-risk diseases. Advances in gene editing technologies, such as CRISPR-Cas9, hold promise for correcting genetic defects in HSCs, potentially expanding the scope of HSCT to treat a broader range of conditions.
Research is also focused on expanding HSCs ex vivo (outside the body) to increase the availability of cells for transplantation and developing safer, more effective conditioning regimens that reduce the toxicity of HSCT.
Conclusion
Hematopoietic stem cells are the foundation of the body’s blood formation system, playing an indispensable role in health by continuously replenishing blood cells and responding to physiological stress. Their dysfunction can lead to a range of hematological diseases, while their unique properties have made them a focal point of regenerative medicine. As research continues to advance, HSCs hold tremendous potential for developing new treatments and improving outcomes for patients with blood-related disorders.