Short Communication - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 9
Hemodynamic Coherence
- *Corresponding Author:
- Maximiliano Soto Estrada
Médico cirujano y partero por la Universidad Autónoma de Chihuahua
E-mail: maxsoes1@icloud.com
Abstract
https://1xbetx.fun https://bahiscom.fun https://casibomagiris.com https://cratosslot.fun https://grandpashabet.fun https://holiganbet.fun https://holiganbet-giris.info https://jojobet.fun https://jojobetgiris.xyz https://kralbet.fun https://meritking.fun https://vdcasino.fun https://onwin.direct https://cypocafe.com https://sahabetgiris.fun
Hemodynamic coherence has its beginnings since 1850, when the need arose to design special rooms to treat serious post-surgical patients. Derived from this, in 1920, specialized post-surgical care areas were created where tools and measuring instruments have been integrated since then for the development of hemodynamic monitoring.
One of the major contributors to hemodynamic monitoring is Dr. Michael R. Pinsky, who proposed 5 principles in hemodynamic monitoring in 2005: Tachycardia is never good, hypotension is always pathological, PVC is only elevated in disease, there is no normal cardiac output and peripheral edema is only of cosmetic importance.
Development
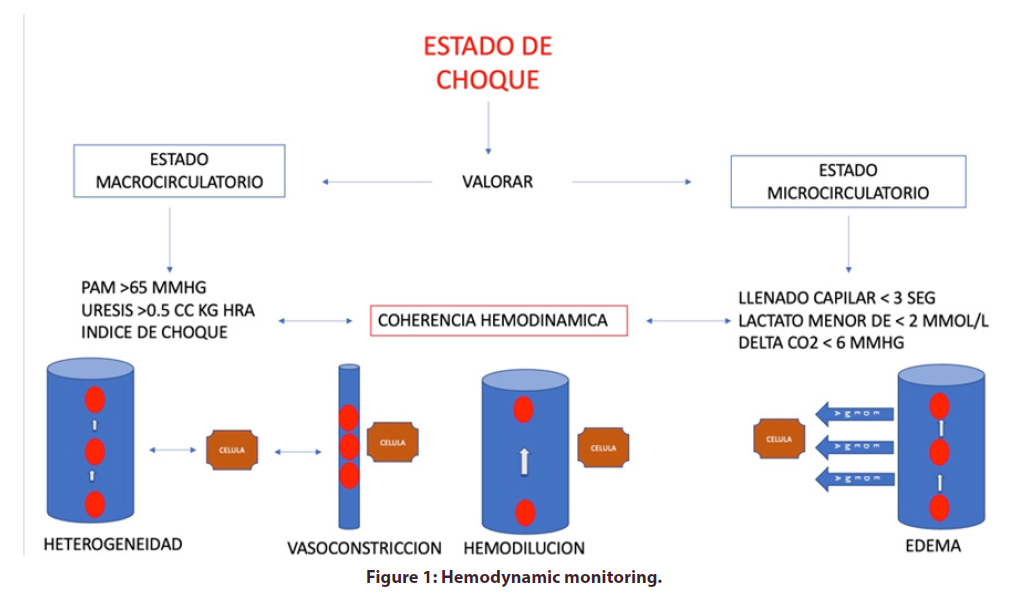
Hemodynamic coherence is a concept that encompasses the balance between the microcirculatory and microcirculatory states. Any measure we take to improve tissue perfusion will also help us to maintain microcirculation, in other words, the goals of resuscitation should be focused on correcting and maintaining both macro circulatory parameters (blood pressure, mean arterial pressure, shock index, pulse pressure, heart rate, neurological status, uresis, tissue perfusion) and microcirculatory (lactate, base deficit, alveolo-arterial carbon dioxide difference, plethysmographic wave) in order to restore normal hemodynamics [1].
The normalization of hemodynamic variables in an incongruent manner and in late stages can have deleterious effects on oxygenation and perfusion of the microcirculation (Table 1 and Figure 1).
| Tissue edema | As a result of inadequate water resuscitation, there is a decrease in O2 diffusion between the erythrocyte (transporting cell) and the O2 molecule receptor cell. |
| Hemodilution | The dilution of the oxygen transporting components promotes the increase of the distance between the erythrocytes and the tissues. |
| Obstruction/ | Local circulatory failure due to microthrombosis in blood capillaries. |
| vasoconstriction | |
| Heterogeneity | It presents a heterogeneous perfusion of tissue due to a set of perfused capillaries and other obstructed ones. |
Table 1: Four mechanisms of loss of haemodynamic coherence have been proposed.
Clinical pearls
• Hemodynamic monitoring should be continuous and easy to interpret, correlating physiological parameters with metabolic parameters, so it is of vital importance to always evaluate patients through clinical perfusion windows and look for loss of hemodynamic coherence through the 4 mechanisms [2].
• Hypotension as a clinical parameter in shock is a late manifestation and should always be correlated with clinical and metabolic variables to determine states of tissue hypoperfusion.
• Tachycardia is never good, and its translation into shock is the need to improve cardiac output. In combination with hypotension and polypnea it forces us to perform immediate interventions to improve macro and microcirculation. Never terminate the work if the patient persists with tachycardia [3].
• Peripheral edema does NOT translate water overload, and the absence of this is NOT indicative to start a generous hydration so we must use tools such as (POCUS) in these patients to guide hydration. On the other hand, peripheral oedema DOES translate acute kidney injury.
Conclusions
Hemodynamic coherence is the balance that must be preserved between macro and microcirculation, so it is vitally important to know the clinical perfusion windows and apply them to any patient we identify in a state of shock. The isolated alteration of parameters that evaluate the macro circulation can translate tissue hypoperfusion so we must always correlate them with metabolic variables such as lactate, base deficit and veno arterial difference of carbon dioxide considered valuable tools that indicate tissue hypoperfusion. Therefore, let us always seek to maintain by means of clinical windows and metabolic variables to preserve hemodynamic coherence.
References
- Pérez Nieto, Zamarrón López, Guerrero Gutiérrez. Clinical hemodynamic monitoring: Back to basics. Intesive. Qare. (2019).
- Ochoa Parra. History and evolution of critical medicine: from intensive care to intensive therapy and critical care. Acta. Colombiana. De. Cuidados. Intensivos. Elsevier. 17(4), 258–268 (2017).
- Carlos Arguelles-Pérez, Oscar Torres-Aguilar, Enrique Monares-Zepeda et al. Dr. Pinsky's 5 principles. Acta. Colombiana. De. Cuidados. Intensivos. Elsevier. 20(1), 45–49 (2020).