Case Report - Interventional Cardiology (2011) Volume 3, Issue 1
Hemodynamics of cardiogenic shock in a Broken Heart Syndrome patient: paradoxical effect of ionotropic agents in apical ballooning
- Corresponding Author:
- Jamal Hussain
Banner Good Samaritan Medical Center, AZ, USA
E-mail: heart7446@gmail.com
Abstract
Keywords
Broken Heart Syndrome,cardiomyopathy,shock,Takotsubo
Case History
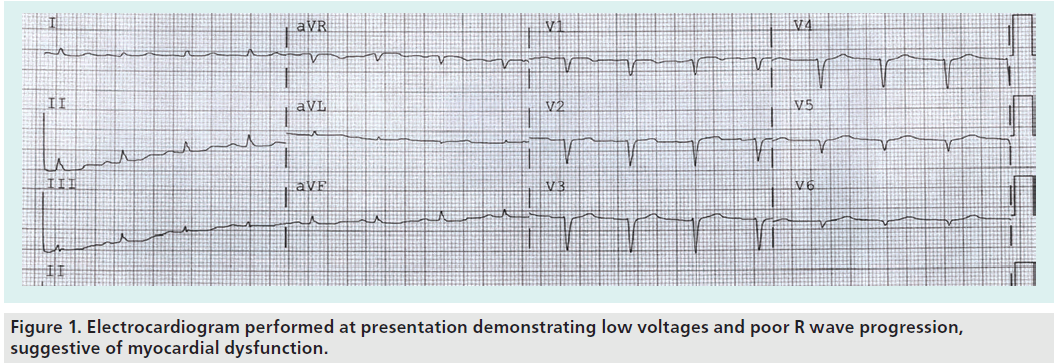
A 56-year-old lady presented to a remote hospital within a few hours of experiencing sudden chest pain while at home, which she described as pressure across her chest associated with shortness of breath. She admitted to suffering recent financial stress. Upon examination at a local emergency room, the patient was found to have nonspecific electrocardiogram abnormality with reduced QRS voltages (Figure 1). In addition, her troponin level was elevated and her blood pressure had deteriorated. Treatment began immediately with intravenous ionotropic drugs. Her initial systolic blood pressure was 60 systolic mmHg and the patient had persistent dyspnea and reduce urinary output. She was transferred to our facility for further management with suspected cardiogenic shock due to acute coronary syndrome.
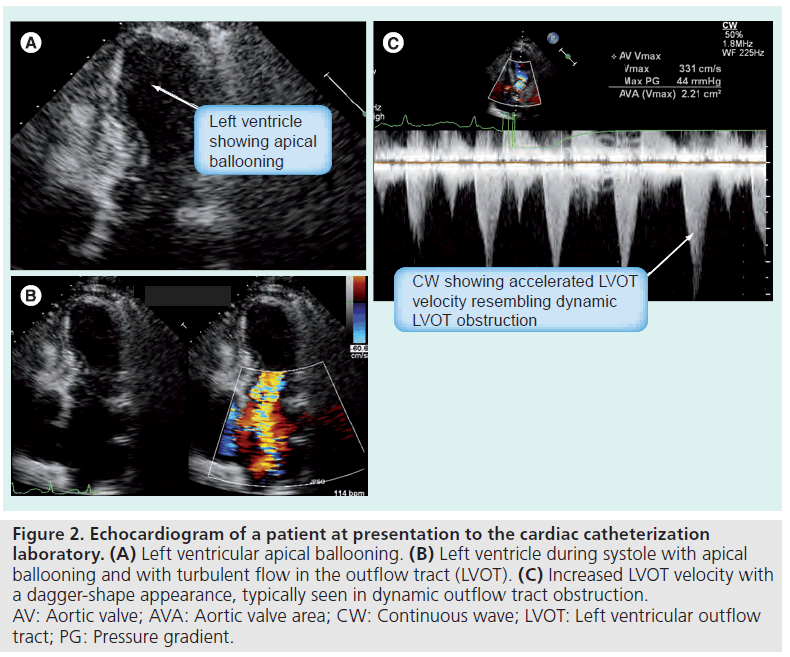
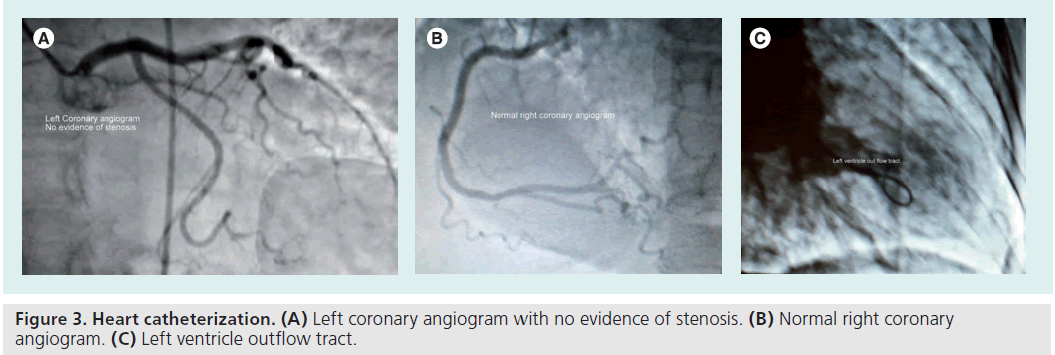
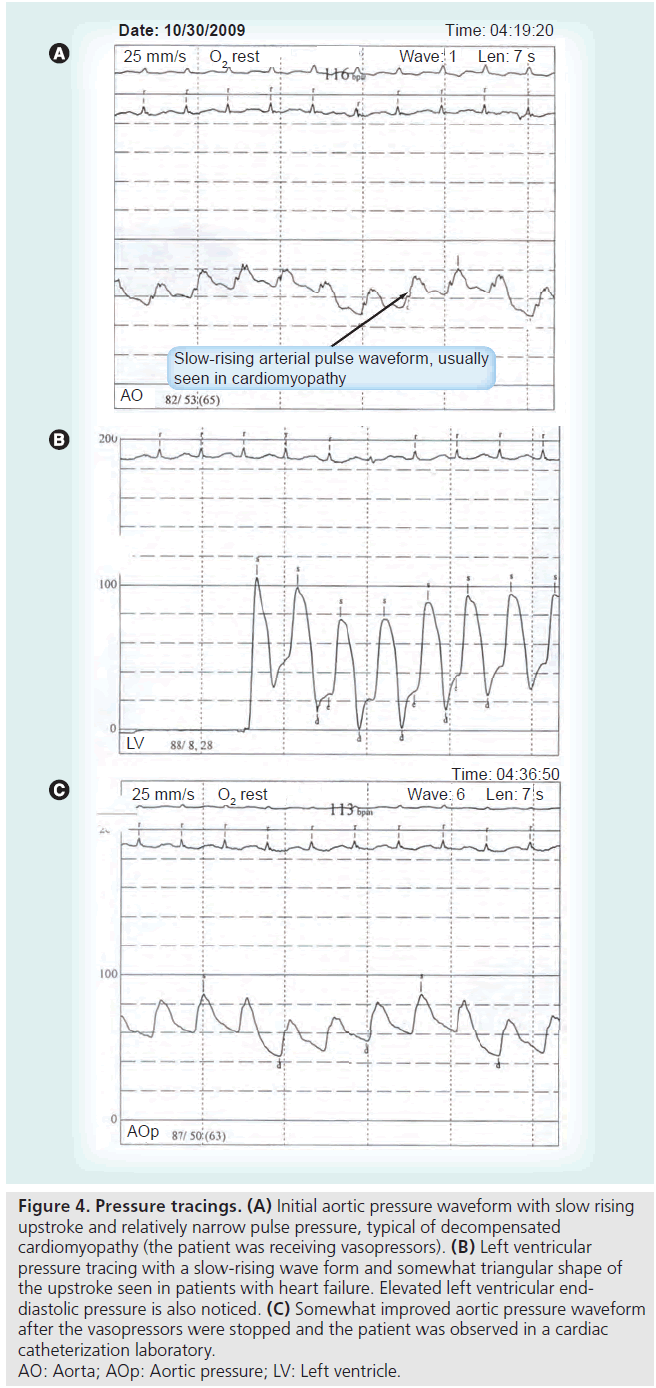
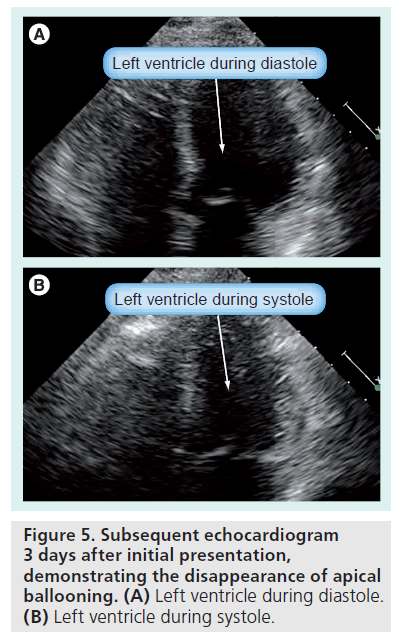
Upon arrival in the cardiac catheterization laboratory, an echocardiogram was performed, which revealed mid–distal inferior anterior wall and apical hypokinesia (Figure 2A–C). A coronary angiogram revealed normal coronary arteries (Figure 3A & B) and the left ventriculogram revealed hypercontractile basal segments and apical ballooning. Consequently, a diagnosis of Takotsubo cardiomyopathy was made.The patient was still hypotensive with a systolic blood pressure of 65 mmHg (Figure 4A & B). Hypotension was suspected to be due to left ventricular outflow tract obstruction, in addition to myocardial dysfunction. A decision was made to stop ionotropic agents and monitor the patient for blood pressure improvement. The patient’s blood pressure improved to approximately 70–80 systolic mmHg after approximately 10 min of stopping ionotropic agents (Figure 4C). At that point, an intra-aortic balloon pump (IABP) was inserted for hemodynamic support and the patient was transferred to an intensive care unit. Her urinary output improved dramatically, her chest resolved and she was monitored clinically and by simple cardiopulmonary monitoring of her symptoms, heart rhythm and blood pressure. Over the next 24–48 h her situation improved, maintaining adequate perfusion of her vital organs. The IABP was removed and on the following day, pharmacological treatment with ACE inhibitors was started, and a small dose of b-blocker was administered the day following that. Routine ambulation was without any symptoms. To our surprise, a follow-up echocardiogram revealed completely normal left ventricular systolic function (Figure 5A & B), and the patient was discharged in a stable condition.
Figure 2: Echocardiogram of a patient at presentation to the cardiac catheterization laboratory. (A) Left ventricular apical ballooning. (B) Left ventricle during systole with apical ballooning and with turbulent flow in the outflow tract (LVOT). (C) Increased LVOT velocity with a dagger-shape appearance, typically seen in dynamic outflow tract obstruction. AV: Aortic valve; AVA: Aortic valve area; CW: Continuous wave; LVOT: Left ventricular outflow tract; PG: Pressure gradient.
Figure 3: Heart catheterization. (A) Left coronary angiogram with no evidence of stenosis. (B) Normal right coronary angiogram. (C) Left ventricle outflow tract.
Figure 4: Pressure tracings. (A) Initial aortic pressure waveform with slow rising
upstroke and relatively narrow pulse pressure, typical of decompensated
cardiomyopathy (the patient was receiving vasopressors). (B) Left ventricular
pressure tracing with a slow-rising wave form and somewhat triangular shape of
the upstroke seen in patients with heart failure. Elevated left ventricular enddiastolic
pressure is also noticed. (C) Somewhat improved aortic pressure waveform
after the vasopressors were stopped and the patient was observed in a cardiac
catheterization laboratory.
AO: Aorta; AOp: Aortic pressure; LV: Left ventricle.
Conclusion
Conclusion Takotsubo cardiomyopathy is an increasingly recognized acute coronary syndrome, and arises mostly in temporal relation to a stressful situation. Correct diagnosis is important for proper management and subsequent follow-up. Different morphologic patterns of left ventricular dysfunction have been noticed, with the apical ballooning and hypercontracting basal segments being the most common, observed in 60% of patients. Ionotropic agents are the mainstay of treatment in most forms of cardiogenic shocks due to cardiomyopathic processes. However, in apical ballooning syndrome, owing to already existing hypercontracting basal myocardium, ionotropic agents can further reduce cardiac output by causing left ventricular outflow tract obstruction, resulting in further hypotension and hemodynamic deterioration. Once this phenomenon is recognized, ionotropic agents should be stopped or replaced with vasopressor agents with minimal ionotropic effects, and hemodynamic support with an intra-aortic balloon pump can stabilize the patient’s condition. Ionotropic management depends on the type of Takotsubo, since in atypical Takotsubo, where basal segments are hypokinetic and where predominantly apical hypercontraction exists, ionotropic agents will be better tolerated than the apical ballooning type of Takotsubo. In refractory cardiogenic shock patients, extracorporeal life support may be required temporarily, since most of these patients hemodynamically improve and stabilize rapidly over the course of a few days after initial presentation. In our patient, discontinuation of ionotropes and the institution of IABP support resulted in the progressive improvement of her clinical condition and return to normal function. This case is also somewhat unique, compared with previously observed cases at our center and those already published in the literature with regards to the patient’s left ventricular systolic function which returned to normal in a very short period of time, in a matter of approximately 3 days.
Information resources
▪▪ Dote K, Sato H, Tateishi H et al.: Myocardial stunning due to simultaneous multivessel coronary spasm: a review of 5 cases. J. Cardiol. 21, 203–214 (1991).
▪▪ Kurowski V, Kaiser A, von Hof K et al.: Apical and midventricular transient left ventricular dysfunction syndrome (Tako-Tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest 132, 809–816 (2007).
▪▪ Bybee K, Prasad A: Stress-related cardiomyopathy syndromes. Circulation 118, 397–409 (2008).
▪▪ Desmet WJ, Adriaenssens BF, Dens JA: Apical ballooning of the left ventricle: first series in white patients. Heart 89(9), 1027–1031 (2003).
▪▪ Mahmoud R, Mansencal N, Pilliere R et al.: Prevalence and characteristic of left ventricular outflow tract obstruction in Tako-tsubo syndrome. Am. Heart J. 156(3), 543–548 (2008).
▪▪ Bonacchi M, Maiani M, Harmelin M, Sani G: Intractable cardiogenic shock in stress cardiomyopathy with left ventricular outflow tract obstruction: is extra-corporeal life support the best treatment? Eur. J. Heart Failure 11(7), 721–727 (2009).
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪▪ Takotsubo cardiomyopathy is an increasingly recognized syndrome, most commonly seen in female patients usually arising after a known stressful event.
▪▪ Patients with Takotsubo cardiomyopathy can also present with cardiogenic shock. One must be fully informed to enable proper management of this condition. Conventional treatment with vasopressors may not be beneficial, and may worsen outflow tract obstruction.
▪▪ Hemodynamic support with an intra-aortic balloon pump and supportive treatment in the intensive care unit appears to be beneficial in stabilizing these patients.
▪▪ Prognosis is usually favorable and left ventricular systolic function recovers in many patients.
▪▪ With evolving awareness of this condition, formal management guidelines may be proposed by heart failure societies. Management during the acute stage requires consideration of the potential worsening of outflow tract obstruction and worsening hemodynamics associated with vasopressor therapy.
▪▪ One must also be conscious of other infrequent hemodynamic subsets in this condition, in which the apical segments are hypercontractile and akinetic basal segments of left ventricle or the so called ‘reverse Takotsubo syndrome’ are present.