Case Report - Interventional Cardiology (2023) Volume 15, Issue 5
Iatrogenic coronary intrastent dissection treated with a drug-eluting balloon: Case report
- Corresponding Author:
- Marek M. Rogowski
Department of Cardiology, Agaplesion General Hospital, Cardiology Clinic, Hagen, Germany,
E-mail: marcorogowski@gmail.com
Received date: 30-Oct-2023, Manuscript No. FMIC-23-118860; Editor assigned: 02-Nov-2023, PreQC No. FMIC-23-118860 (PQ); Reviewed date: 16-Nov-2023, QC No. FMIC-23-118860; Revised date: 23-Nov-2023, Manuscript No. FMIC-23-118860 (R); Published date: 30-Nov-2023, DOI: 10.37532/1755-5310.2023.15(5).772
Abstract
Introduction: Intrastent dissection is a unique and rare form of coronary dissection and can occur in both bare metal and drug-eluting stents. The literature data regarding prevalence, treatment, and patients’ outcomes are limited to case reports and report series. Case presentation: This paper illustrates a rare case of iatrogenic intrastent dissection (type B according to The National Heart, Lung, and Blood Institute) that occurred during a percutaneous coronary intervention. Intravascular ultrasound revealed a tear of the drug-eluting stent neointima. This was treated safely with a prolonged dilatation with a drug-eluting balloon. The primary result was excellent. During the intervention, the patient remained asymptomatic and was discharged the next day for dual anti-platelet therapy. The invasive follow-up three months later showed a very good result, both angiographically and in intravascular ultrasound. Conclusion: This case demonstrates the usefulness and clinical safety of drug eluting balloons in coronary intrastent dissection.
Keywords
Intrastent dissection • Coronary intervention • Intra Vascular Ultra Sound (IVUS) • Drug-eluting balloon
Abbreviations
BMS: Bare Metal Stent; CCS: Canadian Cardiovascular Society; DEB: Drug-Eluting Balloon; DES: drug-eluting stent; IVUS: Intra Vascular Ultra Sound; NCB: Non-Compliant Balloon; NHLBI: National Heart, Lung, and Blood Institute; PCI: Percutaneous Coronary Intervention; RCA: Right Coronary Artery; TIMI: Thrombolysis in Myocardial Infarction
Introduction
In the era of modern interventional cardiology, performed mainly via transradial access, overall complications have decreased significantly. Still, coronary dissection, due to either manipulation of the guiding catheter or associated with the guidewire, occurs in up to 10% of coronary interventions [1]. Based on the NHLBI classification, various dissection types exist and may influence the immediate interventional outcome and overall prognosis [2,3]. Depending on the dissection class and flow limitation, different management strategies have been suggested including conservative, medical, and interventional treatment, the last usually with prolonged balloon dilation and implantation of a drug-eluting stent [4].
Intrastent dissection is a unique and rare form of coronary dissection and can occur in both bare metal and drug-eluting stents [5,6]. The literature data regarding prevalence, treatment, and patients’ outcomes are limited to case reports and report series. No large high-quality data has ever been collected [7].
This paper describes a rare case of catheter-induced dissection of the neotima in the old drug-eluting stent treated successfully with a drug-eluting balloon.
Case Presentation
A female patient, aged 67, was referred to our institution to perform a diagnostic coronary angiography. The lady complained of typical angina pectoris (Canadian Cardiovascular Society grading 2) for 3 months. The referring cardiologist diagnosed an unlimited left ventricular ejection fraction on echocardiography and no relevant abnormalities were seen on her ECG. The stress treadmill testing was negative (up to 100 Watt). Due to inconclusive stress-testing, myocardial scintigraphy was performed and revealed large ischemia of the posterior wall (>10%).
The medical history encompassed a coronary artery disease with prior Percutaneous Coronary Intervention (PCI) (with two DES) of the proximal Right Coronary Artery (RCA) 2018, well- controlled arterial hypertension, no diabetes, and high LDL values despite statin treatment (LDL 120 mg/dl, 20 mg simvastatin).
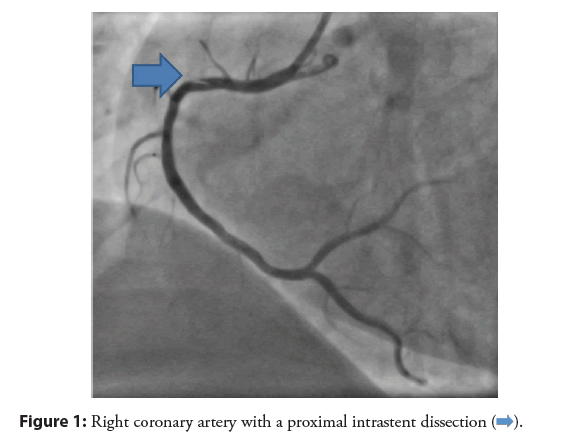
On physical examination, no significant abnormalities were found. On the diagnostic coronary angiogram, a relevant De novo stenosis directly after the old stents of the RCA was revealed. The other coronary vessels were without significant abnormalities. The stenosis was treated with direct implantation of a drug-eluting stent (3.0 × 12 mm, 18 atm) after wiring the distal part of the vessel with 2 guiding wires (to enhance the backup). During the extraction of the jailed wire, some resistance appeared, and the guiding catheter (JR 4.0 6F) dived deeply into the proximal part of the RCA. The immediate angiography demonstrated a good primary result after PCI/DES and an acute type B dissection of the proximal RCA (in the old stent), without any flow limitation (Figure 1).
Figure 1: Right coronary artery with a proximal intrastent dissection
Due to normal coronary flow, normal ECG, and only a few symptoms, further evaluation with Intravascular Ultrasound (IVUS) was performed. IVUS confirmed a dissection flap in the old stent, or more precisely a tear of the neointima with an acute separation of the neotissue from the old stent struts (Figure 2). The stents were well expanded and no malapposition could be seen.
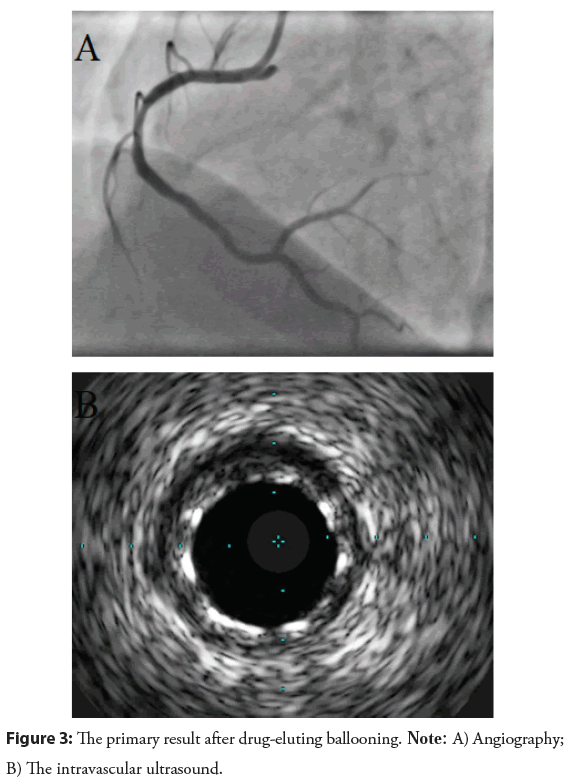
Given the Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow (i.e. complete perfusion) and the detected neointimal tear of the well-implanted stents, a prolonged balloon dilatation was performed (NC 3,0 × 20 mm, 16 atm, 60 s), followed by dilatation with a drug-eluting balloon (3.0 × 20 mm, 12 atm, 90 s). The primary result, both angiographically and in IVUS, was excellent (Figure 3).
Post-PCI the patient stayed one night in the intermediate care unit and was discharged the next day on the dual antiplatelet therapy (for 6 months).
During the regular follow-up, three months later, the patient remained asymptomatic. The control coronary angiography showed a very good interventional result, both angiographically and in IVUS.
Results and Discussion
Spontaneous intrastent coronary dissection is extremely rare and occurs usually as a classical plaque rupture due to progressive neoatherosclerosis. Iatrogenic cases of intrastent dissection, on the contrary, are typically caused by a guiding catheter due to aggressive manipulation and deep intubation. Keeping the catheter in the coaxial position may be a reasonable preventive step [8-10].
Drug-eluting balloons enable local drug delivery without traditional stenting. This approach has many potential benefits, among them an immediate and steady drug release to the vessel wall without the use of a polymer matrix, short antiplatelet therapy, no metal object remaining in the vessel, and perhaps lower restenosis rate. In case of an in-stent restenosis, European Society of Cardiology gives the strongest 1A recommendation for DEB based on data from randomized clinical trials [3]. In De novo coronary lesions, DEB-only strategy may become a reasonable option in small vessel disease, long lesions, or bifurcations.
To the author’s knowledge, the illustrated case is one of the very few examples of intrastent dissection treated with a drug-eluting balloon. This strategy seems to be a safe and effective treatment option in such cases. It must be stressed, however, that a stent dysfunction such as malapposition, under expansion, or fracture must be excluded, preferably using optical coherence tomography or intravascular ultrasound. The avoidance of DES-in-DES strategy may bring potential benefits for the patient and influence the overall prognosis as well [11].
Conclusion
Iatrogenic coronary intrastent dissection is a rare peri-interventional complication, caused mainly by aggressive manipulation of a guiding catheter in a non-coaxial fashion. The long-term outcome and its impact on overall prognosis have not been well examined so far but it may be more benign. Like any other coronary dissection, it can be treated conservatively or interventionally, depending on flow limitation, the patient’s symptoms, and ECG changes.
The current case does not only illustrate the usefulness and clinical safety of drug-eluting balloons, but also highlights the importance of intracoronary imaging. As the IVUS clearly showed a dissection flap within a well-apposed and regular expanded stent, it was reasonable to try to avoid a stent sandwich (DES-in-DES) and treat the dissection with a pure balloon dilatation followed by a prolonged dilatation with a paclitaxel-coated balloon. The implementation of paclitaxel may favor and accelerate the healing process. On the other hand, the conservative management of a Type A and B coronary dissection due to actual drug-eluting ballooning was shown to be a safe and effective procedure.
As the follow-up coronary angiography and IVUS demonstrated an excellent middle-term result after three months, it can be concluded that the usage of drug-eluting balloons, combined with proper anatomical imaging guidance, can be a prudent and highly useful option in treating intrastent dissection and could be considered as a potential invasive management strategy.
References
- Gonzalo N, Serruys PW, Okamura T, et al. Optical coherence tomography assessment of the acute effects of stent implantation on the vessel wall: A systematic quantitative approach. Heart. 95(23):1913-1919 (2009).
[CrossRef] [Google Scholar] [PubMed]
- Ohmure K, Yoshino S, Fukumoto D, et al. In-stent catheter-induced neointimal dissection assessed by optical coherence tomography. JACC Cardiovasc Interv. 10(14):1462-1463 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Jeger RV, Eccleshall S, Wan Ahmad WA, et al. International DCB consensus group. Drug-coated balloons for coronary artery disease: Third report of the international DCB consensus group. JACC Cardiovasc Interv. 22;13(12):1391-1402 (2020). doi: 10.1016/j.jcin.2020.02.043. Epub 2020 May 27. PMID: 32473887.
[CrossRef] [Google Scholar] [PubMed]
- Gutiérrez-García H, Amat-Santos IJ, Román-Calvar JAS. Intrastent coronary dissection assessed with optical coherence tomography. Rev Esp Cardiol (Engl Ed). 65(6):570 (2012). doi: 10.1016/j.recesp.2010.09.016
[CrossRef] [Google Scholar] [PubMed]
- Yashima F, Yuasa S, Maekawa Y, et al. In-Stent dissection causes no flow during percutaneous coronary intervention. JACC Cardiovasc Interv. 11;9(1):102-103 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Franke KB, Wong DTL, Baumann A, et al. Current state-of-play in spontaneous coronary artery dissection. Cardiovasc Diagn Ther. 9(3):281-298 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Takenaka K, Murasato Y. A case of iatrogenic intra-stent coronary dissection after Biolimus-eluting stent deployment in the left main coronary artery. J Cardiol Clin Res. 4(8):1086 (2016).
[Google Scholar] (All versions)
- Rivero F, Cuesta J, Benedicto A, et al. Ruptured neoatherosclerosis presenting as a large intrastent neointimal dissection. J Am Coll Cardiol Intv. 7(11):e169-e170 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 7;40(2):87-165 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Yerasi C, Case BC, Forrestal BJ, et al. Drug-coated balloon for de novo coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol. 75(9):1061-1073 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Modaragamage-Dona AC, Abuelgasim E, Abuelgasim B, et al. Dissection of coronary artery: A clinical overview. J Cardiol. 77(4):353-360 (2021).
[CrossRef] [Google Scholar] [PubMed]