Commentary - Imaging in Medicine (2016) Volume 8, Issue 1
Iatrogenic post-catheterization radial arteriovenous fistula in 64-old male patient
Róbert Novotný*, Jaroslav Hlubocký, Petr Mitáš, Ján Hrubý, Miroslav Špaček, Rudolf Špunda, Ján Tošovský & Jaroslav LindnerGeneral University Hospital, 2nd Department of Cardiovacular Surgery, U nemocnice 2, Prague, Czech Republic
- Corresponding Author:
- Róbert Novotný
General University Hospital
2nd Department of Cardiovacular Surgery
U nemocnice 2, Prague, Czech Republic
Tel: +420773679206
E-mail: novotny_robert@hotmail.com
Abstract
Background: We are presenting a case report of an iatrogenic left radial post-catheterization arteriovenous fistula. A 64-year-old male patient one year after percutaneous coronary intervention (PCI) with coronary stent implants was admitted with a pulsatile, palpable mass with bruit and intermittent pain in the region of the left radial artery. Finding: Ultrasonography of the left radial artery was performed, confirming a radial arteriovenous fistula (AVF) in the place of PCI. Method: Percutaneous embolization (PE) with thrombin was chosen as a treatment of choice based on the anatomical localization and characteristics of the AVF. The PE treatment was repeated twice with suboptimal post-procedural result. One day after the PE an ultrasonographic check-up was performed, confirming a suboptimal result of PE with a light palpable bruit present in the place of the AVF. Patient was indicated for surgical resection. After the surgical resection, patient was immediately relieved of all accompanying symptoms and was discharged two days after the procedure. Conclusion: The preferred treatment of choice for post-catheterization arteriovenous fistulas is percutaneous embolization. Surgical resection of post-catheterization AVF is used only when all percutaneous treatments fail.
Keywords
Catheterization; arteriovenous fistula; radial artery; resection
Learning Objective
We have presented a rare case of iatrogenic radial AVF after PCI which was unsuccessfully treated with thrombin PE, followed by a surgical resection. Radial artery is an effective access site for coronary catheterization and PCI with additional benefits of lower incidence of postprocedural complications, shorter length of hospital stay and reduced patient costs when compared to TFI access.
Introduction
In the recent decade we have noticed a dramatic shift from transfemoral (TFI) to transradial (TRI) access for a coronary catheterization and percutaneous coronary intervention (PCI) [1]. Major reasons for this dramatic shift are the decrease of major access site complications, shorter hospital stay and cost effectiveness [2,3]. Due to the rise of TRI access use, it is important to understand the potential major and minor complications of TRI catheterization and PCI. Post-catheterization radial arteriovenous fistula (AVF) is a very rare complication that requires an attention. The treatment options consist of either conservative, endovascular of surgical treatments based on the AVR anatomical characteristics [4].
Case report
A 64-year-old male patient with ischemic heart disease, New York Heart Association (NYHA: ll) Functional Classification, Arterial hypertension (WHO: ll st.) and type 2 Diabetes mellitus underwent a diagnostic coronary catheterization trough the left radial artery. During the coronary catheterization a 75% hemodynamically significant stenosis was found on the right posterolateral branch of the right coronary artery and the right posterior descending coronary artery. Drug eluted stents were implanted into the stenotic coronary arteries with an excellent hemodynamic result, with no sign of residual stenosis. One year after the PCI patient noticed a palpable mass with bruit and intermittent pain localized at the site of PCI.
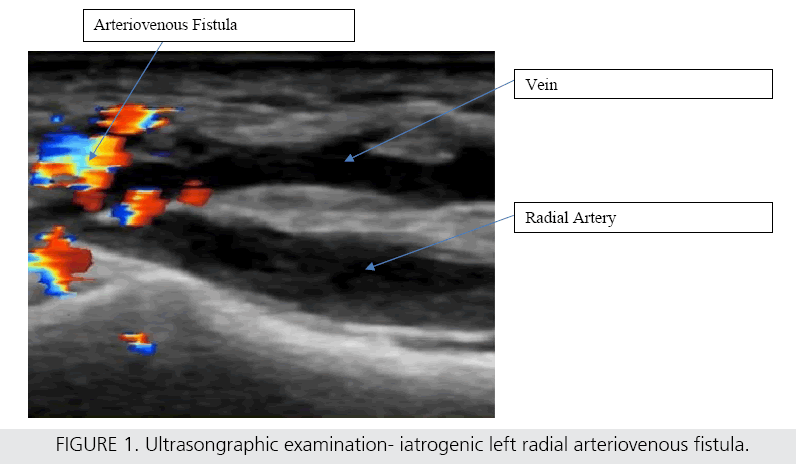
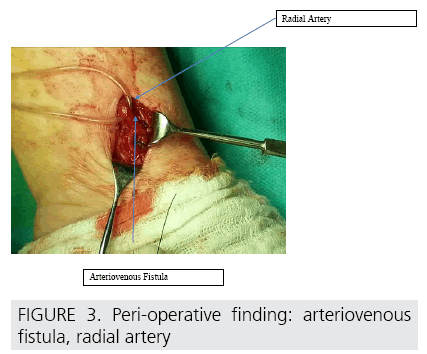
Patient was admitted into our center where he underwent a physical and an ultrasonographic examination of the left radial artery with a finding of an AVF (FIGURE 1). Percutaneous embolization (PE) with thrombin was chosen as a treatment of choice based on the anatomical localization and characteristics of the AVF (“tunnel” like shape of the AVF, AVF dimensions and depth of AVF arising measured by Doppler’s ultrasonography) [5], with suboptimal postprocedural result. PE intervention was repeated once more due to the unsatisfying result. After the PE, an ultrasonographic check-up was performed, confirming a suboptimal result of PE with a light palpable bruit still present in the place of the AVF. Patient was indicated for surgical resection of the AVF. Longitudinal, 3 cm long incision was made in the place of AVF previously marked on the untrasonographic examination (FIGURE 2). The left radial artery and AVF were carefully dissected (FIGURE 3).
The AVF was resected at the point of entrance into the left radial artery, and both ends of the fistula were ligated with a nylon suture. Radial artery remained intact with visible and palpable pulsations. After the surgical resection, patient was immediately relieved from all accompanying symptoms and was discharged two days after the procedure without any complications.
Discussion
The gold standard in diagnosing and treating cardiac disease is a cardiac catheterization. The most frequent complications of cardiac catheterization are associated with access site complications: bleeding, hematoma formation, pseudoaneurysm, AVF [6]. Various factors such as patient’s characteristics, interventional cardiologist technique, access site selection, medication used before, during and after catheterization can greatly affect and minimise vascular complications [7,8].
Ongoing bleeding from the arterial puncture site may decompress into the adjacent venous puncture site, leading to the formation of an arteriovenous fistula [9]. Several trials examined TRI versus TFI access site for coronary catheterization and PCI. Meta-analysis of this trial had shown better procedural efficacy of TRI vs. TFI access [10]. With better cost effectives, shorter hospital stay, lower incidence of major access site complications in elderly and obese patients, lower incidence of bleeding in patients receiving glycoprotein llb/llla inhibitors and without compromising the success and range of possibilities associated with modern day PCI. These are clearly the main reasons why it is becoming a preferred access site not only for coronary intervention [2,3,11]. Even though the unquestionable advantages of TRI vs. TFI access are well documented, there are still many avenues for further research. Improving patient safety, refining of the technique and clarifying discrepancies concerning alternative techniques [12]. It is essential to gain a better understanding of potential major and minor complications of TRI catheterization and PCI [13]. The most common complication of TRI access is radial artery occlusion. Radial artery occlusion is mostly asymptomatic due to the collateral flow from the ulnar artery with the exception of five cases where patients were presented with forearm pain, loss of strength and paresthesia [14]. Iatrogenic post-catheterization radial AVF is a very rare complication with an incidence of 0, 04% [15]. Tatli et al. suggests that majority of post-catheterization AVF can be managed conservatively. Nonetheless this applies only for a small percentage of AVF. In most cases a conservative treatment is insufficient due to the high blood flow through the arteriovenous fistula. The standard treatment of AVF is thrombin embolization, however new endovascular treatments are emerging with an excellent results as an alternative treatment minimising patient’s hospital stay and hospital costs [4]. If all percutaneous and endovascular treatments fail, patients are indicated for a surgical resection.
References
- Greenberg G, Bental T, Lev EI et al. A Comparative Matched Analysis of Clinical Outcomes between Transradial versus Transfemoral Percutaneous Coronary Intervention. Isr. Med. Assoc. J. 17, 360-4 (2015).
- Dangoisse V, Guédès A, Gabriel L et al. Full conversion from transfemoral to transradial approach for percutaneous coronary interventions results in a similar success rate and rapid reduction of in hospital cardiac and vascular major events. Eurointervention. 9, 345- 352 (2013).
- Plehn G, Örnek A, Gkiouras G et al. Transradial versus transfemoral approach in coronary angiography: a matched pair analysis of cath lab equipment costs. J. Vasc. Access. 16, 413-417 (2015).
- Sugahara T, Azuma M, Nakashima K et al. Postcatheterization radial arteriovenous fistula: balloon-assisted direct percutaneous embolization with N-butyl cyanoacrylate and 50 % glucose solution in two sessions. Jpn. J. Radiol. 31, 505-10 (2013).
- La Perna L, Olin JW, Goines D et al. Ultrasound-guided thrombin injection for the treatment of postcatheterization pseudoaneurysms. Circulation. 102, 2391-2395 (2000).
- Azzalini L, Tosin K, Chabot-Blanchet M et al. The Benefits Conferred by Radial Access for Cardiac Catheterization Are Offset by a Paradoxical Increase in the Rate of Vascular Access Site Complications With Femoral Access: The Campeau Radial Paradox. JACC. Cardiovasc. Interv. Pii, S1936-8798(15)01444- 2 (2015).
- Hoeper MM, Lee SH, Voswinckel R et al. Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J. Am. Coll. Cardiol. 48, 2546-2552 (2006).
- Dumont CJ, Keeling AW, Bourguignon C et al. Predictors of vascular complications post diagnostic cardiac catheterization and percutaneous coronary interventions. Dimens. Crit. Care. Nurs. 25,137-42 (2006).
- Ndrepepa G, Kastrati A Minimising bleeding during percutaneous coronary intervention. BMJ. 350: h1395 (2015).
- Jae-Sik Jang, Han-Young Jin, Jeong-Sook Seo et al. The transradial versus the transfemoral approach for primary percutaneous coronary intervention in patients with acute myocardial infarction: a systematic review and metaanalysis. Eurointervention. 8, 501-10 (2012).
- Hibbert B, Simard T, Wilson KR et al. Transradial versus transfemoral artery approach for coronary angiography and percutaneous coronary intervention in the extremely obese. JACC. Cardiovasc. Interv. 5, 819-826 (2012).
- Sachdeva S, Saha S Transradial approach to cardiovascular interventions: an update. Int. J. Angiol. 23, 77-84 (2014).
- Kassimis G, Channon KM, Hahalis G et al. Transradial arterial access catheter knots: how to stay out of trouble. Minerva. Cardioangiol. 63, 449-456 (2015).
- Bernat I, Bertrand OF, Rokyta R et al. Ef?cacy and safety of transient ulnar artery compression to recanalize acute radial artery occlusion after transradial catheterization. Am. J. Cardiol. 107,1698–1701 (2011).
- Tatli E, Buturak A, Cakar A et al. Unusual Vascular Complications Associated with Transradial Coronary Procedures Among 10,324 Patients: Case Based Experience and Treatment Options. J. Interv. Cardiol. 28, 305- 312 (2015).