Editorial - Imaging in Medicine (2010) Volume 2, Issue 2
Imaging swine flu: is it ever necessary?
Prachi P Agarwal1, Ella A Kazerooni*1Division of Cardiothoracic Radiology, University of Michigan Health System, Cardiovascular Center 5383, 1500 East Medical Center Drive, Ann Arbor, MI 48109-5868, USA
- Corresponding Author:
- Ella A Kazerooni
Division of Cardiothoracic Radiology
University of Michigan Health System
Cardiovascular Center 5482, 1500 East Medical Center Drive
Ann Arbor, MI 48109-5868, USA
Tel: +1 734 936 4366
Fax: +1 734 232 5055
E-mail: ellakaz@med.umich.edu
Abstract
From the time of emergence of the novel influenza A (H1N1) infection in April 2009, the disease has spread widely, leading the WHO to declare the emergence of a global pandemic by raising the worldwide pandemic alert level to Phase 6 [1].
According to the WHO, as of 17 January 2010, more than 209 countries and overseas territories or communities have reported laboratory- confirmed cases of pandemic influenza 2009 H1N1, including at least 14,142 deaths [101]. It is worth noting that the 2009 H1N1 influenza virus continues to be the dominant influenza virus in circulation in the world. Between the period 3–9 January 2010, nearly three quarters (74.6%) of influenza-positive specimens were typed as influenza A; the overwhelming majority (97.2%) of which were subtyped to be 2009 H1N1 positive [102].
However, it is important to realize that the figures on disease prevalence are a substantial underestimate of the disease magnitude. To obtain a true estimate of the disease burden is very challenging owing to several factors. Many people with influenza may not seek medical care and even if they do so, not all patients are laboratory tested for disease confirmation. Even for patients who are hospitalized, there may be underreporting owing to inaccurate test results related to the timing and quality of specimens, or attributing hospitalizations and deaths to other causes, such as secondary complications of influenza [2]. Reed et al. used a statistical model to ascertain the disease prevalence in the USA and reported that every case of 2009 H1N1 (from April to July 2009) represented an estimated 79 total cases, and every hospitalized case reported may have represented an average of 2.7 total hospitalized people [2]. Using this methodology, the CDC estimates that between 1 April and 12 December 2009, 39–80 million cases of 2009 H1N1 occurred with 173,000–362,000 2002 H1N1-related hospitalizations and 7880–16,460 2009 H1N1- related deaths [103]. What does this really mean in terms of performing and interpreting imaging studies when facing a disease of this magnitude? Do none, all or some patients need imaging? If imaging is needed, what purpose should it serve?
As we know, H1N1 is a clinical diagnosis that is confirmed with a laboratory test and not based on imaging findings. In fact, a recent retrospective study demonstrated that only 30% (66/222) of patients with confirmed or presumed 2009 H1N1 infection received any form of imaging study [1]. However, this is not an accurate representation of the use of imaging resources. For example, not all patients seek medical treatment and, therefore, would not be reflected in these numbers. At the same time, there are several others who have clinical features of respiratory infection and may receive imaging studies but do not have laboratory testing to confirm 2009 H1N1 status. However, given the retrospective nature of the study [1], it is not possible to infer how patients who received imaging differed in their clinical presentation from those who did not. Chest radiographs serve as the frontline diagnostic examination and are often used by clinicians as a baseline to monitor the progression of disease and get an estimate of disease severity. Use of imaging is often at the discretion of the clinicians and tailored to individual patients. The study results are, however, encouraging and point to the fact that imaging may not be needed in the majority of patients as most cases of 2009 H1N1 infection are mild and self limited.
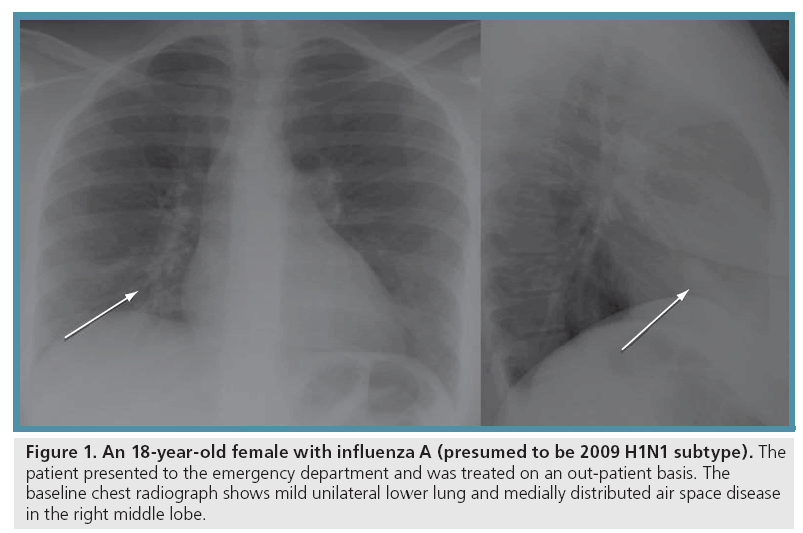
This is also substantiated by the fact that the chest radiographs were normal in more than half (38/66; 58%) of the patients who did go on to receive a diagnostic study [1]. When abnormal, the chest radiographic findings were found to be unilateral or bilateral patchy air space disease (ground glass, consolidation or both) most commonly distributed in the lower (71%) and central (71%) aspects of the lungs (Figure 1) [1].
Figure 1: An 18-year-old female with influenza A (presumed to be 2009 H1N1 subtype). The patient presented to the emergency department and was treated on an out-patient basis. The baseline chest radiograph shows mild unilateral lower lung and medially distributed air space disease in the right middle lobe.
Enlarged thoracic lymph nodes were not identified on any of the chest radiographs and pleural effusions were seen in only a small percentage (8%) of patients [1].
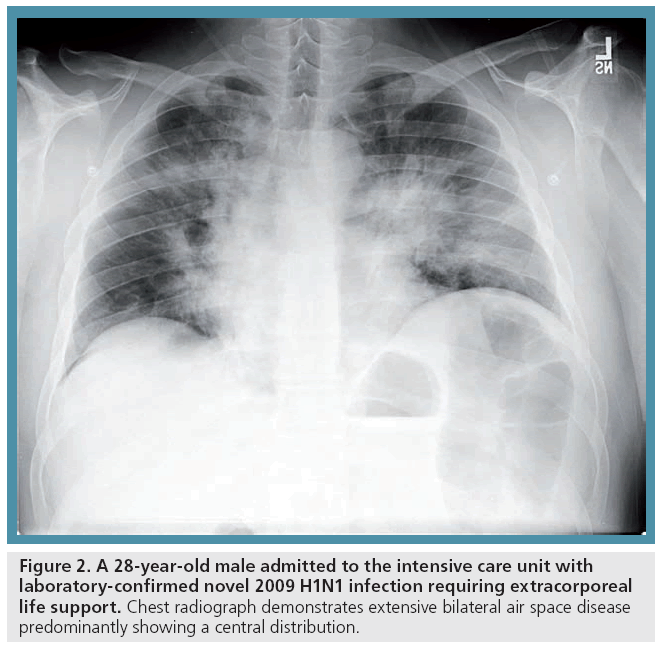
A minority of patients with 2009 H1N1 can, however, progress to severe illness and may even need admission to an intensive care unit (ICU) and advanced mechanical ventilation (Figure 2). This group of patients is distinct and requires close observation. In our experience at the University of Michigan (MI, USA), this number was reported to be approximately 6% (14/222) [1], which is likely to be an overestimate owing to the previously mentioned reasons of underestimating the denominator (the actual sick population) and the quaternary care nature of the institute, where several severely ill patients were directly transferred during the time period of our review for advanced care, including evaluation for extracorporeal life support. It is this group of ICU patients that utilize maximum radiology resources and are followed up by serial radiographs and often CT examinations. A recent study evaluated the utilization of imaging resources during the recent outbreak (1 May–18 July 2009) and found that the ICU group received a mean of 33.5 chest radiographs, 5.1 abdominal radiographs, 1.1 thoracic CT examinations and 4.2 nonthoracic CT examinations, in contrast to an average of less than 1.4 chest radiographic studies and 0.1 thoracic CT examinations for patients who did not require any kind of mechanical ventilation [3]. Additionally, if several of these critically ill patients are in the ICU of a hospital at the same time, they can create an increased demand on radiology departments through the sudden increase in imaging examination utilization.
Figure 2: A 28-year-old male admitted to the intensive care unit with laboratory-confirmed novel 2009 H1N1 infection requiring extracorporeal life support. Chest radiograph demonstrates extensive bilateral air space disease predominantly showing a central distribution.
Patients in the ICU often have comorbidities and complications that dictate the type and frequency of imaging studies. For example, a high incidence of pulmonary emboli was noted in ICU patients (5/14; 36%) [1]. It is not clear if pulmonary embolism is directly related to 2009 H1N1 infection or caused by their associated comorbidities, which may have contributed to the severe course of the primary 2009 H1N1 infection. A CT examination to ‘routinely’ screen for pulmonary embolism in ICU patients (which is a very small fraction of the total 2009 H1N1-infected population) is not advisable and should only be used as an adjunctive management tool for clinical decision-making, for example, in patients who show clinical deterioration that is not otherwise explained.
In conclusion, the use of imaging needs to be tailored to individual patients and this calls for judicious and effective use of available imaging resources.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Agarwal PP, Cinti S, Kazerooni EA: Chest radiographic and CT findings in novel swine-origin influenza A (H1N1) virus (S-OIV) infection. AJR Am. J. Roentgenol. 193, 1488–1493 (2009).
- Reed C, Angulo FJ, Swerdlow DL et al.: Estimates of the prevalence of pandemic (H1N1) 2009, United States, April–July 2009. Emerg. Infect. Dis. 15(12), 2004–2007 (2009).
- Schafer JRA, Agarwal PP, Kazerooni EA: Radiology resource utilization during an H1N1 influenza outbreak. J. Am. Coll. Radiol. 7(1), 28–32 (2010).
-
Websites
WHO: Pandemic (H1N1) 2009 update 84 www.who.int/csr/don/2010_01_22/en/ index.html - WHO: Pandemic (H1N1) 2009 update 84. Weekly virological surveillance update www.who.int/csr/disease/swineflu/ laboratory22_01_2010/en/index.html
- CDC estimates of 2009 H1N1 influenza cases, hospitalizations and deaths in the USA between 1 April–12 December 2009 www.cdc.gov/h1n1flu/estimates_2009_ h1n1.html