Research Article - Interventional Cardiology (2022) Volume 14, Issue 6
Implantation of pacemaker to monitor ventricular function and dyssynchrony
- Corresponding Author:
- Samir Rafla
Department of Cardiology,
Alexandria University,
Alexandria,
Egypt,
E-mail: smrafla@yahoo.com
Received date: 09-Nov-2022, Manuscript No. FMIC-22-79395; Editor assigned: 11-Nov-2022, PreQC No. FMIC-22-79395 (PQ); Reviewed date: 25-Nov-2022, QC No. FMIC-22-79395;Revised date: 02-Dec-2022, Manuscript No. FMIC-22-79395 (R);Published date: 12-Dec-2022, DOI: 10.37532/1755-5310.2022.14 (6). 606
Abstract
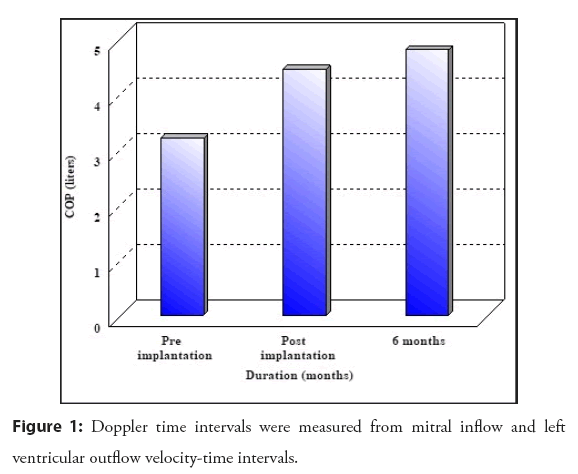
Background: Pacing from the apex of the RV is not optimal. This study aimed to assess and compare RV and LV pacing of LV function and dyssynchrony. Methods: Thirty-six patients who presented with indications for pacemakers were divided into three groups. 12 had LV pacing (lead was inserted from coronary sinus to lateral vein, the same procedure used in resynchronization pacing). Twelve had RV pacing group (apical pacing only, not septal or outflow). Twelve had Dual-chamber pacing. Twelve healthy participants were included in this study as Control group. Results: During the post-implantation period, the distance of the 6-MWT improved significantly, P=0.006. Cardiac Output (COP) during the preimplantation period and at the six-month follow-up (P=0.003). The IVT (Isovolumic Time) variables at six months’ pre- and post-implantation periods (P=0.005) (LV pacing group). The comparison of the 6-MWT distance and the Quality of Life (QOL) score in the post-implantation period and at six months revealed a highly significant difference (improvement) as well as in the median values of the PAP (RAP: Right Atrial Pressure), COP, MPI (MPI: Myocardial Performance Index), IVT, and Z (Z ratio: sum of the left ventricular ejection and filling times divided by RR interval) (P=0.000). Conclusions: RVP seems to have fewer detrimental effects on LV synchrony and LV function. For those patients indicated for conventional pacemaker indications with normal or mildly impaired LV function with EF>35%, RVA (right ventricular apical) pacing is still the gold standard pacing site.
Keywords
Pacemakers • Cardiac resynchronization therapy • RV dysfunction • Heart failure • RV apical pacing
Abbreviations
6-MWT: 6-MInute Walk Test; AVB: Atrioventricular Block; AVD: AV Delay; BiV: Biventricular; CRT: Cardiac Resynchronization Therapy; DDD: Dual-Chamber Pacing; EMD: Electromechanical Delay; ESD: End-Systolic Dimension; ESV: End-Systolic Volume; CO: Cardiac Output; VTI × area × heart rate; DT is the Deceleration Time of early diastolic mitral flow; EF: Ejection Fraction; ET: Ejection Time; FT: Filling Time; ICT: Isovolumetric Contraction Time; IRT: Isovolumetric Relaxation Time; IVMD: Interventricular Mechanical Delay, difference between LV electromechanical delay LVEMD and RV electromechanical delay; LVEDD: Left Ventricular End-Diastolic Diameter; LVESD: Left Ventricular End-Systolic Diameter; MPAP: Mean Pulmonary Artery Pressure; MPI: Myocardial Performance Index; PWP: Pulmonary Capillary Wedge Pressure; RAP: Right Atrial Pressure; RVA: Right Ventricular Apical; TDI: Tissue Doppler Imaging; IVT: Total Isovolumic Time: 60- (Total Ejection Time+Total Filling Time) ; VTI: Velocity-Time Integral of aortic flow velocity; Z ratio: Sum of the left ventricular ejection and filling times divided by RR interval
Introduction
RVA (RV apical) pacing causes significant intraventricular conduction delay. The left and right ventricle segment at different times and the interventricular septal wall contracts abnormally. This phenomenon results in decreased contractility, diastolic filling, and Mitral Regurgitation (MR). Abnormal activation of the ventricle via RVA pacing may result in multiple abnormalities in cardiac function, which may ultimately affect clinical outcomes [1-12].
Conception and rationale of the study
This study aimed to assess and compare right ventricular and left ventricular pacing in terms of left ventricular function and dyssynchrony in patients indicated for permanent pacemaker implantation using echocardiography and tissue Doppler imaging.
Materials and Methods
The study was approved by and conducted according to the instructions of the author’s institutional Human Investigations or Ethics Committee.
All patients subjected to pacemaker implantation (LVP and RVP) included in this study were subjected to the following:
• History taking and complete clinical examination emphasizing the indication for pacemaker implantation, new NYHA functional class, and blood pressure.
• Standard twelve lead resting Electrocardiogram (ECG).
• Quality of life was evaluated with Minnesota living with Heart failure Questionnaire (QOL).
• The Minnesota Living with Heart failure (LIh FE) questionnaire.The patient groups of pacemaker implantation for more than six months were subjected to the following:
• History taking and complete clinical examination emphasizing the NYHA functional class, the pacemaker implantation indication, and the implantation duration.
• Standard twelve leads resting Electrocardiogram (ECG).
• Echocardiographic study.
• Systolic and diastolic blood pressure.
• The 6-minute walk distance.
• Quality of life evaluation with Minnesota living with heart failure questionnaire.
The control group was subjected to the same echocardiographic study as the patient group.
Indication of pacing was complete heart block in some, sick sinus syndrome in some (Sinus rate was consistently below 45 beats per minute, so the pacemaker was active in RV pacing more than 90% of the time).
Exclusion criteria
Patients having the following diseases were excluded from the study,
• Valvular heart diseases (stenotic and severe regurgitant lesions).
• Cardiac failure crises or dependency on intravenous inotropes.
• Unstable angina, acute myocardial infarction, CABG, or PCI within 30 days before study enrollment.
• Chronic obstructive pulmonary diseases.
• Restrictive heart diseases.
• Hypertrophic obstructive cardiomyopathy.
Baseline clinical characteristics
Sinus node dysfunction: Sinus bradycardia is any stable sinus rate below 50 bpm. P waves have a normal contour and occur before each QRS complex, usually with a constant PR interval greater than 120 ms. Only those with persistent bradycardia with syncope were paced.
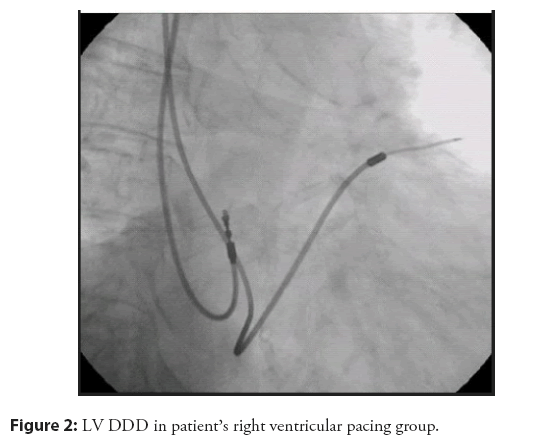
The difference in pacing sites along the right ventricle: All were RV apical pacing, none septal pacing. LV pacing was done through lead specific for the resynchronization system, inserted in the coronary sinus (Figure 1).
Echocardiographic measurements and calculations
I-M-mode and two-dimensional examination: M-mode echocardiography measurements were made according to the American Society of Echocardiography guidelines. Left Ventricular End-Diastolic Diameter (LVEDD) and Left Ventricular End-Systolic Diameter (LVESD) were evaluated.
Left ventricular ejection fraction EF was assessed using the modified biplane Simpson’s rule using the apical four-chamber and two-chamber views, where the length of the ventricular image was maximized.
LVEDV: Left Ventricular End-Diastolic Volume.
LVESV: Left Ventricular End-Systolic Volume.
II-Pulsed wave Doppler measurements
Measurements were performed for the estimation of the following hemodynamics;
Pulmonary Wedge Pressure (PWP): Pulmonary Wedge Pressure (PWP)=51-(0.26 × DT)
DT is the deceleration time of early diastolic mitral flow.
Mitral flow velocity was assessed from a standard apical 4-chamber view by placing a 3 mm sample volume adjacent to the tip of the mitral leaflets in diastole, as shown in Figure 2.
Deceleration time was measured as the interval between peak early diastolic velocity and the point where the steepest deceleration slope was extrapolated to the baseline in ms.
Right Atrial Pressure (RAP): Right Atrial Pressure (RAP)= -1.263+(0.01116 × AR)
AR is the acceleration rate of diastolic tricuspid flow.
Mean Pulmonary Artery Pressure (MPAP): Mean Pulmonary Artery Pressure (MPAP)=90-(0.62 × AT)
Cardiac Output (COP): Cardiac Output (COP)=VTI × area × heart rate
The area is calculated from the left ventricular outflow tract diameter.
Area (cm2)= π (d/2)2
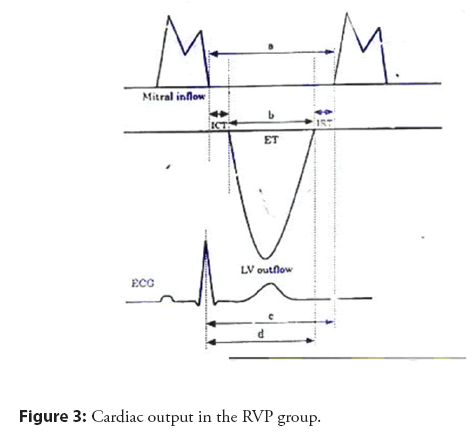
Myocardial Performance Index (MPI): Myocardial Performance Index (MPI) = The sum of the isovolumic contraction time and the isovolumic relaxation time divided by the ejection time.
Doppler measurements
Mitral inflow and LV outflow velocity-time intervals were used to measure Doppler time intervals: Isovolumic Contraction (IVCT), Relaxation Time (IVRT), and Ejection Time (ET), as demonstrated. The sum of the IVCT and IVRT was derived from the interval from the end of mitral inflow to the onset of the next mitral inflow signal minus the LV outflow ejection time. The interval “a” from the cessation to the onset of mitral inflow was equal to the sum of IVCT, ET, and IVRT. Left ventricular ET “b” was the duration of the left ventricular velocity profile, measured as the interval between the onsets of forward aortic flow to the onset of the aortic closure artifact in seconds. IVRT was calculated by subtracting the interval “d” between the R wave and the cessation of left ventricular outflow from the interval “c” between the R wave and the onset of mitral inflow. IVCT was calculated by subtracting IVRT from “a”-”b.”
Total Isovolumic Time (IVT): Total Isovolumic Time (IVT): 60-(total ejection time+total filling time).
Z ratio: Sum of the left ventricular ejection and filling times divided by RR interval.
Interventricular Mechanical Delay (IVMD): Interventricular Mechanical Delay (IVMD)= Difference between left ventricular electromechanical delay LVEMD and right ventricular electromechanical delay.
III-Tissue Doppler imaging TDI
Pulsed wave tissue Doppler: Tissue Doppler imaging analysis was performed in Pulsed Wave (PW) Doppler modality from the apical view to assess the longitudinal myocardial regional function by analyzing, respectively, the Interventricular Septum (IVS), inferior, lateral, and the anterior left ventricular wall. The myocardial velocity profiles of each division were recorded with a 5 mm sample volume placed in the middle of the basal segment of each myocardial wall. In addition, the basal segment of the right ventricular free wall was also sampled for its myocardial velocity.
Regional time intervals
The following systolic and diastolic time interval was identified for each region,
• The regional COM interval (Cessation to the Onset of Mitral Flow) (COMF) lengthening from the end of the last blue component of the preceding cycle to the beginning of the first homogenous diastolic component decoded in blue.
• The regional E-A interval (E-AR) is detected from the end of the third systolic red component to the end of the blue diastolic component.
• The regional Isovolumic Contraction (ICTR) lengthens from the beginning of the first systolic red component to the beginning of the second systolic red component.
• The regional Isovolumic Relaxation Time (IRTR) lengthens from the end of the second systolic red component to the end of the third red component.
• The regional LV Ejection Time (LVETR) results from the difference between the COMR interval and the interval resulting from the sum of ICTR+IRTR intervals, that is, (COMR-(ICTR+IRTR).
M-Mode color TDI was used as a map reference in the qualitative Analysis of all regional time intervals.
Echocardiographic measurements and calculations: We measured Left Ventricular End-Diastolic Diameter (LVEDD), Left Ventricular End-Systolic Diameter (LVESD), and ejection fraction EF. DT is the deceleration time of early diastolic mitral flow. Right Atrial Pressure (RAP)=-1.263+(0.01116 × AcR). AcR is the acceleration rate of diastolic tricuspid flow. Mean Pulmonary Artery Pressure (MPAP)=73-(0.42 × AT). Cardiac output (COP)=VTI × area × heart rate. VTI is the Velocity-Time Integral of aortic flow velocity. Myocardial Performance Index (MPI). The sum of the isovolumic contraction time and the isovolumic relaxation time is divided by the ejection time. Total isovolumic time (IVT)=60-(total ejection time+total filling time). Z ratio=Sum of the left ventricular ejection and filling times divided by RR interval. Interventricular Mechanical Delay (IVMD)=Difference between left ventricular electromechanical delay LVEMD and right ventricular electromechanical delay. An IVMD ≥ 40 ms, 2 SD above the mean of normal controls, represents interventricular dyssynchrony. Intraventricular mechanical delay: LPEI represents a complex interaction between ventricular contraction, preload, and afterload.
A delay of 140 ms is considered indicative of intraventricular dyssynchrony.
The relevant guidelines and regulations
Follow-up: Patients were followed up at one three and six months post implant by the following evaluating parameters: The 6-minute walk test and quality of life.
The pacing burden: All the patients had pacing dependency at least 90% of the time. Follow-up was up to six months. The conclusions may have been different if the follow-up was two years, for example, but this was one of the study’s limitations; nevertheless, the findings of six months follow-up are still valuable.
Clinical characteristics of pacing: No major complication happened in all our studies. Pocket hematoma in 5% managed conservatively. Lead dislodgment in none, cardiac perforation in none, inadvertent puncture of subclavian artery instead of the vein in one, managed conservatively. The duration of implantation of the lead and pacemaker was 15 to 45 minutes maximum.
Statistical analysis: This was performed using SpSS Ver.11.5.
• Description of qualitative variables was done using the percent.
• The median two range described quantitative variables, and non-parametric statistical tests were used in the Analysis due to the variables’ non-normality. (K-S<0.05).
• The Mann-Whitney test compared the pacing groups (LVP and RVP groups) regarding the quantitative variables. In contrast, comparisons between the different groups (LVP, RVP, RVP more than six months, and control groups) were made using the Kruskal-Wallis test.
• Comparisons between the different groups regarding the qualitative variables were made using the X2 test. In the case of invalid X2, the exact tests were used. All tests were 2-sided. The significance level was set at 0.05.
• Using Friedman’s test, intragroup comparisons during the pre and post-implant periods and the follow-up period at 1, 3, and 6 months for quantitative variables. In addition, significantly different time points were compared using the Wilcoxon Signed ranks tests. Regarding qualitative variables, an intragroup comparison was made using the Cochran test, and significantly different time points were compared using McNemar’s test.
• Correlations between different variables were done using Spearman’s rank correlation coefficient.
Results
Right ventricular pacing group
The indication for permanent pacemaker implantation in six patients (50%) was sick sinus syndrome (sinus rate was consistently below 45 beats per minute, so the pacemaker was active in RV pacing more than 90% of the time). In comparison, in three patients (25%), the indication was acquired AV block. In two patients (16.7%), the indication was post-operative AV block; in one patient (8.3%), the indication was congenital third-degree AV block.
During the post-implantation period, the distance of the 6-MWT ranged from 329 to 705 m with a median of 493.5 m. During the following period, at one month, it ranged from 376 m to 705 m with a median of 493.5 m; at three and six months, it went from 423 m to 705 m with a median of 540.5 m.
After pacing, the QOL score ranged from 0 to 39, with a median of 0 during the study period. During the follow-up period of one, three, and six months, QOL scores ranged from 0 to 20, from 0 to 8, and from 0 to 5, respectively. During the preimplantation period, nine patients (75%) had no dyspnea, or other symptoms of heart failure, the other three patients (25%) were in NYHA class II. Ten patients (83.3%) had no dyspnea in a six-month follow-up period, and two (16.7%) became in NYHA class I.
Twelve lead resting electrocardiogram
As regards the QRS width, all patients had QRS width <120 ms before pacemaker implantation. During the post-implantation and follow-up periods, five patients (41.6%) had a QRS width of 120 ms, five patients (41.6%) had a QRS width >120- ≤ 140 ms and two patients (16.7%) had a QRS width >140 ms. Seven patients (58.3%) had complete left bundle branch blocks, and five patients (41.6%) had incomplete left bundle branch blocks after pacemaker implantation and during the follow-up period.
By comparing the RVP group and the LVP group, a significant difference in the 6-MWT distance in favor of the RVP group, i.e., a more extended length during the post-implant and the follow-up periods. In our study, the female gender was 25% in the RVP group and 50% in the LVP group. The prevalence of the female gender was the predictor of poor 6-MWT performance in the LVP group.
By comparing patients in the same group during the pre and post-implantation periods and at six months follow-up, a significant difference was found in the 6-MWT between the post-implantation period and at six months follow-up in the RVP and LVP groups which indicates that pacing improves the physical fitness and activity of patients, p=0.01.
Echocardiographic study
Conventional echo-Doppler: Two-dimensional and M-mode measurements: The LV dimensions and ejection fraction are shown in Table 1.
| RVP | LVP | P-value | ||
|---|---|---|---|---|
| EDD | Post | 49.0 (33.0-68.0) | 49.5 (38.0-76.0) | 0.931 |
| 6 | 46.5 (34.0-67.0) | 51.0 (38.0-75.0) | 0.297 | |
| ESD | Post | 29.5 (19.0-55.0) | 31.5 (25.0-57.0) | 0.885 |
| 6 | 29.0 (17.0-56.0) | 32.5 (24.0-56.0) | 0.685 | |
| EF | Post | 62.0 (40.0-73.0) | 57.0 (41.0-64.0) | 0.099 |
| 6 | 60.5 (47.0-70.0) | 56.5 (46.0-69.0) | 0.203 | |
Note*: Significant P-value<0.05
Table 1: Echo Doppler data: Left ventricular dimensions and ejection fraction.
This shows that there was no deterioration of RV or LV function from RV or LV pacing.
Pulsed-wave Doppler measurements: The DT, the AR, and the AT during the pre and post-implantation periods and the follow-up period are shown in Table 2, shows the ICT and the IRT before and after pacemaker implantation and during the follow-up period.
| RVP | LVP | P-value | ||
| PWP | Post | 17.0 (9.0-20.0) | 13.0 (9.0-25.0) | 0.09 |
| 6 | 17.0 (9.0-25.0) | 12.0 (9.0-18.0) | 0.061 | |
| RAP | Post | 3.0 (1.0-5.0) | 3.0 (1.0-5.0) | 0.179 |
| 6 | 3.0 (1.0-7.0) | 3.0 (2.0-4.0) | 0.809 | |
| MPAP | Post | 18.0 (6.0-28.0) | 18.0 (6.0-22.0) | 0.976 |
| 6 | 14.0 (6.0-22.0) | 14.0 (8.0-22.0) | 0.46 | |
| MPI | Post | 0.365 (0.32-0.38) | 0.365 (0.32-0.38) | 0.7 |
| 6 | 0.370 (0.34-0.39) | 0.365 (0.32-0.38) | 0.459 | |
| t-IVT | Post | 11.30 (10.3-20.1) | 11.60 (11.4-16.2) | 0.271 |
| 3 | 11.75 (10.3-21.1) | 15.00 (10.6-17.3) | 0.052 | |
| 6 | 12.85 (10.3-21.9) | 14.40 (11.6-17.0) | 0.133 | |
| Z ratio | Post | 80.0 (66.0-82.0) | 80.0 (73.0-81.0) | 0.277 |
| 6 | 78.0 (64.0-82.0) | 75.5 (71.0-80.0) | 0.124 | |
Note: MPAP: Mean Pulmonary Artery Pressure; MPI: Myocardial Performance Index; t-IVT: Total Isovolumic Time: 60- (Total ejection time + Total filling time); Z ratio: Sum of the left ventricular ejection and filling times divided by RR interval; *: Significant P value<0.05
Table 2: Echo Doppler Hemodynamics: pulmonary wedge pressure, right atrial pressure, means pulmonary artery pressure, myocardial performance index, total isovolumic time, and Z ratio.
Echo Doppler data: Regional peak systolic velocities by pulsed-wave TDI in the RV pacing group and LV pacing group are shown in Table 3. Again, this indicates no significant dyssynchrony in either RV or LV pacing groups.
| RVP | LVP | p-value | ||
|---|---|---|---|---|
| Lateral | Post | 5.62 (3.75-6.25) | 5.50 (3.90-6.70) | 0.339 |
| 6 | 5.77 (5.00-6.75) | 5.50 (3.90-6.00) | 0.054 | |
| Septum | Post | 5.47 (4.00-6.50) | 5.52 (3.95-6.25) | 0.603 |
| 6 | 5.27 (4.50-6.25) | 5.45 (3.65-6.25) | 0.795 | |
| Anterior | Post | 5.55 (3.25-6.50) | 5.10 (3.90-6.70) | 0.355 |
| 6 | 5.45 (3.60-6.00) | 5.05 (3.75-6.10) | 0.165 | |
| Inferior | Post | 5.47 (3.75-6.20) | 5.35 (3.80-6.75) | 0.247 |
| 6 | 5.47 (3.85-6.20) | 5.15 (2.90-6.10) | 0.157 | |
| Right ventricular free wall | Post | 5.70 (3.75-6.50) | 5.25 (4.40-6.85) | 0.603 |
| 6 | 5.70 (5.15-6.25) | 5.47 (4.30-6.25) | 0.052 | |
Note: *: Significant P value<0.05
Table 3: Echo Doppler data. Regional peak systolic velocities by pulsed-wave TDI.
Comparison between RV pacing group and LV pacing group: Qualitative assessment of intraventricular mechanical dyssynchrony by color M-mode TDI in the four walls of the left ventricle is shown in Table 4. It shows no significant dyssynchrony in either RV or LV pacing groups.
| Color M-mode pattern | RVP | LVP | P-value | ||||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||
| Lateral | Post | I | 4 | 33.3 | 12 | 100 | 0.001* |
| II | 8 | 66.7 | 0 | 0 | |||
| 6 | I | 4 | 33.3 | 12 | 100 | 0.000* | |
| II | 8 | 66.7 | 0 | 0 | |||
| Septum | Post | I | 1 | 8.3 | 12 | 100 | 0.000* |
| II | 11 | 91.7 | 0 | 0 | |||
| 6 | I | 1 | 8.3 | 12 | 100 | 0.000* | |
| II | 11 | 91.7 | 0 | 0 | |||
| Anterior | Post | I | 4 | 33.3 | 12 | 100 | 0.001* |
| II | 8 | 66.7 | 0 | 0 | |||
| 6 | I | 4 | 33.3 | 12 | 100 | 0.000* | |
| II | 8 | 66.7 | 0 | 0 | |||
| Inferior | Post | I | 1 | 8.3 | 12 | 100 | 0.000* |
| II | 11 | 91.7 | 0 | 0 | |||
| 6 | I | 1 | 8.3 | 12 | 100 | 0.000* | |
| II | 11 | 91.7 | 0 | 0 | |||
Note: *: Significant P value<0.05.
Table 4: Echo Doppler data: Qualitative assessment of intraventricular mechanical dyssynchrony by color M-mode TDI in the four walls of the left ventricle.
Clinical data in Table 5: Six-minute walk test and quality of life score are shown in Table 5, which reveals no significant difference in RVP and LVP.
B-Tissue Doppler imaging: The regional EMD in the lateral, septum, anterior, inferior, and right ventricular free walls are shown in Table 5.
| RVP | LVP | RVP>6 months | P-value | |
|---|---|---|---|---|
| 6-MWT | 540.5 (423-705) | 446.5 (329-564) | 552 (188-634) | 0.015* |
| QOL Score | 0.0 (0.0-5) | 0.0 (0.0-5) | 0.0 (0.0-10) | 0.404 |
| NYHA functional class--I | 10 (83.3%) | 12 (100%) | 10 (83.3%) | 0.519 |
| NYHA functional class--I | 2 (16.7%) | 0 | 2 (16.7%) |
Note: *: Significant P value<0.05
Table 5: Clinical data: 6-minute walk test and quality of life score.
The interventricular mechanical dyssynchrony assessed by conventional pulsed-wave and Tissue Doppler imaging is shown in Table 6.
| Variable | Preimplantation | Post- implantation | Six months | P-value |
|---|---|---|---|---|
| PWP | 16.1 (9.0-22.0) | 17 (9.0-20.0) | 17 (9.0-25.0) | 0.472 |
| RAP | 3 (1-5) | 3 (1.0-5.0) | 3 (1.0-7.0) | 0.639 |
| MPAP | 19 (6.-28) | 18 (6-28) | 14 (6-22) | 0.264 |
| COP | 3.2 (1.7-6.3) | 4.45 (2.8-7.1) | 4.8 (3.3-6.3) | 0.000* |
| MPI | 0.35 (0.31-0.4) | 0.365 (0.32-0.38) | 0.37 (0.29-0.39) | 0.469 |
| t-IVT | 27.9 (12-37) | 11.30 (10-20) | 12.85 (10-21) | 0.003* |
| Z ratio | 55 (40-79) | 80(66-82) | 78 (64-82) | 0.004* |
Note: MPI: Myocardial performance index; t-IVT: Total isovolumic time: 60-(total ejection time + total filling time); Z ratio: sum of the left ventricular ejection and filling times divided by RR interval; *: Significant P value<0.05.
Table 6: Echocardiographic data: Comparison of hemodynamics in the RV pacing group at the preimplantation period, post-implantation period, and six-month follow-up.
Comparison of intraventricular and interventricular mechanical dyssynchrony in the right ventricular pacing group during the preimplantation period, post-implantation period, and six-month follow-up are shown in Table 7.
| Variable | Preimplantation | Post- implantation | Six months | P-value |
|---|---|---|---|---|
| LVPEI (conventional) | 90 (80-110) | 107.5 (93-135) | 127.5 (115-130) | 0.001* |
| RVPEI | 67.0 (60-85) | 87.3 (70-100) | 93.5 (90-95) | 0.01* |
| EMD-4 (TDI) | 7.5 (2-20) | 10 (0.0-40) | 14 (4-25 | 0.042* |
| IVMD (conventional) | 20.0 (10-30) | 18.5 (10-35) | 31 (20-35) | 0.146 |
| Difference between EMD of the lateral wall and right ventricular free wall (TDI) | 10 (2-20) | 11.5 (5-30) | 10 (2-30) | 0.976 |
| Difference between EMD of septum and right ventricular free wall (TDI) | 9 (2-25) | 10 (2.0-25) | 6.5 (50-15) | 0.766 |
Note: *: Significant P value<0.05
Table 7: Echocardiographic data. Comparison of intraventricular and interventricular mechanical dyssynchrony in the right ventricular pacing group at the preimplantation period, post-implantation period, and six-month follow-up.
In the critical evaluation, by comparing RVP to LVP in group A, no significant difference was found between the groups for all the variables, including left ventricular dimensions and EF, Isovolumic Relaxation Time (IRT), MR score, aortic Flow-Velocity Integral (FVIAo), maximum protodiastolic Mitral Flow (Emax), Mitral Flow-Velocity Integral (FVIMi), Deceleration Time (DT), Diastolic FIlling Time (DFT) and QRS width except for two variables (ESD and MR score) where LVP was superior to RVP.
Thus these results show that RVP seems to have less detrimental effects on LV synchrony. Right ventricular pacing more than six months group. The duration of pacemaker implantation ranged from 3 to 9 years with a median of 6 years. The 6-MWT, the QOL score, the systolic and diastolic blood pressures, and NYHA functional class all improved.
Intragroup comparison: left ventricular pacing group. Intragroup comparisons were made in the RVP group and the LVP group. In addition, in the same group, a comparison was made between the pre and post-implantation variables and variables during the six-month follow-up period.
This significant difference was detected between the COP during the pre-and post-implantation periods (P=0.002) and the preimplantation period and at the six-month follow-up (P=0.003) (Figure 3).
A highly significant difference was also found between the IVT variables at the pre and post-implantation periods and six months (P=0.003), as shown in Table 2. Furthermore, this significant difference was found between the pre-and post-implantation periods (P=0.005), preimplantation periods, and six-month follow-up (P=0.005).
A highly significant difference was demonstrated between the Z ratio at the pre and post-implantation periods and six months (P=0.004). This significant difference was found between the pre-and post-implantation periods (P=0.005), the preimplantation period, and the six-month follow-up (P=0.006). For all the other hemodynamics, no significant difference was found between variables during the pre and post-implantation periods or six-month follow-up.
By comparing RVP, LVP, RVP>six months, and the control group, no significant difference was found in all variables except for 6-MWT, LVPEI, IVMD, and color M-mode TDI patterns.
By comparing patients in the same group, in the RVP group, a significant difference was found in 6-MWT, COP, IVT, Z ratio, LVPEI, EMD-4, and color M-mode TDI patterns.
On the other hand, in the LVP group, a significant difference was found in the 6-MWT, QOL, NYHA functional class, COP, IVT, Z ratio, LVPEI, and EMD-4.
Regarding the intragroup comparison, in the RVP, a significant improvement was shown in only four variables: EF, FVIAo, DFT, and QRS width. On the other hand, in the LVP, the considerable improvement was nearly in the same variables. Therefore, by comparing LVP versus RVP, the significant difference was demonstrated only in the EF, MR score, and QRS width.
Left ventricular pacing group: The comparison of the 6-MWT distance and the QOL score in the post-implantation period and at six months revealed a highly significant difference in the median values (P=0.004, P=0.026, respectively).
Echo Doppler data: Comparison of the left ventricular dimensions and ejection fraction. An insignificant difference was found between the LV dimensions and EF during the pre and post-implantation periods and between the pre and six-month follow-up.
Intragroup comparison (LV pacing group): A highly significant difference between the median values of the mean PAP, COP, MPI, IVT, and Z ratio was found during the pre and post-implantation periods and at six months (P=0.003, P=0.000, P=0.000, P=0.000 and P=0.000 respectively).
Discussion
RV pacing may have deleterious short-term effects based on the propagation of the RV impulse through the myocardium (LV dyssynchrony) and long-term harmful effects of myocardial remodeling that may ultimately lead to myocardial dysfunction [13].
Clinical data
The predictive value of the 6-MWT has been reported previously in patients with CHF [14,15]. In our study, all our patients from all groups had normal or mild LVSD. No significant difference was found in the RVP group by comparing patients in the same group. In contrast, we detected a significant difference in the LVP group, denoting that the LVP improves the functional status and the physical activity of patients with normal and mildly impaired LV function by treating symptomatic bradycardia.
No significant difference was found in the RVP group by comparing patients in the same group. In contrast, a significant improvement was noticed in the NYHA functional class in the LVP group.
Regarding the intragroup comparison, in the RVP, a significant improvement was shown in only four variables: EF, FVIAo, DFT, and QRS width. On the other hand, in the LVP, the considerable improvement was nearly in the same variables. Therefore, by comparing LVP versus RVP, the significant difference was demonstrated only in the EF, MR score, and QRS width.
By comparing LVP and RVP, no significant difference was found in all variables except for 6-MWT, LVPEI, IVMD, and color M-mode TDI patterns at six months.
By comparing RVP, LVP, RVP>six months, and the control group, no significant difference was found in all variables except for 6-MWT, LVPEI, IVMD, and color M-mode TDI patterns.
By comparing patients in the same group, in the RVP group, a significant difference was found in 6-MWT, COP, IVT, Z ratio, LVPEI, EMD-4, and color M-mode TDI patterns.
On the other hand, in the LVP group, a significant difference was found in the 6-MWT, QOL, NYHA functional class, COP, IVT, Z ratio, LVPEI, and EMD-4.
Our results agreed with Varma et al., who demonstrated that RVP’s effects were similar in patients with LBBB and RBBB. Moreover, when baseline conduction system disease was present, RVP’s effects were exaggerated versus RVP in normal QRS cases [14].
Ebrille et al. [16], in a review article, discussed the mechanisms by which ventricular pacing itself can induce dyssynchrony; and whether or not various pacing locations can decrease the deleterious effects caused by ventricular pacing. We think our results will add an alternative view to the literature.
Conclusions
• RV apical pacing seems to have less detrimental effects on LV synchrony.
• For those patients indicated for conventional pacemaker indications with normal or mildly impaired LV function with EF>35%, RV-A (DDD) pacing is still the gold standard pacing site.
• LVP is possible with conventional lead (introduced in coronary sinus) without a significant rise in threshold or reduction of battery longevity.
Limitations
This echocardiographic study did not utilize the current techniques of speckle tracking.
The number in the main three groups is only 36 patients, which is small.
What is of value in this study? First, it revealed that RV apical pacing is not harmful as the usual impression, especially in patients with normal or slightly reduced EF.
Manuscript contribution to the field
• RV apical pacing seems less detrimental to LV synchrony.
• For those patients indicated for conventional pacemaker indications with normal or mildly impaired LV function with EF>35%, RV-A (DDD) pacing is still the gold standard pacing site.
• LVP is possible with conventional lead (introduced in coronary sinus) without a significant rise in threshold or reduction of battery longevity
Role of Authors
This was the doctoral thesis of Dr. D.K.
MA, and MN, were supervisors, and MN was the primary pacemaker operator. SR and all authors participated in writing and revising the manuscript.
Funding
None.
Ethics Approval and Consent to Participate
Ethical permission was granted by the Ethics Committee of the Faculty of Medicine at Alexandria University. Consent for participation was obtained from the patient.
Consent for Publication
Informed written consent was obtained from the patient for their anonymized information to be published in this paper.
Competing Interests
The authors declare that they have no competing interests.
Patient Participation Consent
Consent was taken from each patient.
Data Availability
Availability of Data and Materials: Yes, data are on the computer, available when requested by Dr. Doaa Elkholy.
Acknowledgments
The authors thank all nurses, technicians, and residents who worked during the procedures and echocardiography studies.
References
- Ouali S, Neffeti E, Ghoul K, et al. DDD versus VVIR pacing in patients, ages 70 and over, with complete heart block PACE. Pacing Clin Electrophysiol. 33(11): 583-589 (2010).
[Cross ref] [Google scholar] [PubMed]
- Mond HG, Vlay SC. Pacing the right ventricular septum: Time to abandon apical pacing. Pacing Clin Electrophysiol. 33(11): 1293-1297 (2010).
[Cross ref] [Google scholar] [PubMed]
- Duckett SG, Ginks M, Shetty AK, et al. Invasive acute hemodynamic response to guide left ventricular lead implantation predicts chronic remodeling in patients undergoing cardiac resynchronization therapy. J Am Coll Cardiol. 58(11): 1128-1136 (2011).
[Cross ref] [Google scholar] [PubMed]
- Singh JP, Abraham WT. Enhancing the response to cardiac resynchronization therapy. Is it time to individualize the left ventricular pacing site? J Am Coll Cardiol. 55(6): 576-578 (2010).
[Cross ref] [Google scholar] [PubMed]
- Paparella G, Sciarra L, Capulzini L, et al. Long-term effects of upgrading to biventricular pacing: differences with cardiac resynchronization therapy as a primary indication. Pacing Clin Electrophysiol. 33(7): 841-849 (2010).
[Cross ref] [Google scholar] [PubMed]
- Chung BB, Grinstein JS, Imamura T, et al. Biventricular pacing versus right ventricular pacing in patients supported with LVAD. JACC Clin Electrophysiol. 7(8):1003-1009 (2021).
[Cross ref] [Google scholar] [PubMed]
- Kaye GC, Linker NJ, Marwick TH, et al. Protect-pace trial investigators. Effect of right ventricular pacing lead site on left ventricular function in patients with high-grade atrioventricular block: Results of the Protect-Pace study. Eur Heart J. 36(14):856-62 (2015).
[Cross ref] [Google scholar] [PubMed]
- Cristina R, Cinteza M, Vinereanu D. Interventricular septal or standard apical pacing in pacing-dependent patients: still a dilemma? Maedica (Bucur). 5(3): 193-200 (2010). [Cross ref] [Google scholar] [PubMed]
- Gillis AM. Optimal pacing for right ventricular and biventricular devices. Circ Arrhythm Electrophysiol. 7(5): 968-977 (2014).
[Cross ref] [Google scholar] [PubMed]
- Chan JY, Fang F, Zhang Q, et al. Biventricular pacing is superior to right ventricular pacing in bradycardia patients with preserved systolic function: 2-year results of the PACE trial. Eur Heart J. 32: 2533-2540 (2011).
[Cross ref] [Google scholar] [PubMed]
- Curtis AB, Worley SJ, Adamson PB, et al. Biventricular versus right ventricular pacing in heart failure patients with atrioventricular block (block hf) trial investigators. Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 368: 1585–1593 (2013).
[Cross ref] [Google scholar] [PubMed]
- Barsheshet A, Moss AJ, McNitt S, et al. Long-term implications of cumulative right ventricular pacing among patients with an implantable cardioverter-defibrillator. Heart Rhythm. 8: 212-218 (2011).
[Cross ref] [Google scholar] [PubMed]
- Gillis AM, Russo AM, Ellenbogen KA, et al. HRS/ACCF expert consensus statement on pacemaker device and mode selection. Developed in partnership between the Heart Rhythm Society (HRS) and the American College of Cardiology Foundation (ACCF) and in collaboration with the society of thoracic surgeons. Heart Rhythm. 9: 1344–1365 (2012).
[Cross ref] [Google scholar] [PubMed]
- Varma N. Left ventricular conduction delays induced by right ventricular apical pacing: Effect of left ventricular dysfunction and bundle branch block. J Cardiovasc Electrophysiol. 19: 114-122 (2008).
[Cross ref] [Google scholar] [PubMed]
- Kaye GC, Linker NJ, Marwich T, et al. A randomized comparison of the effect of pacing the right ventricular apex and high septum on left ventricular systolic function in patients with high-grade atrioventricular block: The results of Protect-Pace study. Heart Rhythm Sci. 11: S18 (2014).
- Ebrille E, DeSimone CV, Vaidya VR, et al. Ventricular pacing: Electromechanical consequences and valvular function. Indian Pacing Electrophysiol J. 16(1): 19-30 (2016).
[Cross ref] [Google scholar] [PubMed]