Review Article - Interventional Cardiology (2011) Volume 3, Issue 6
Importance of invasive interventional strategies in resuscitated patients following sudden cardiac arrest
- Corresponding Author:
- Karl B Kern
Sarver Heart Center, University of Arizona, 1501 N Campbell Avenue,Tucson, AZ, USA
Tel: +1 520 626 2477
Fax: +1 520 626 0200
E-mail: kernk@email.arizona.edu
Abstract
Keywords
asystole,cardiac arrest,cardiopulmonary resuscitation.coronary angiography,pulseless electrical activity,therapeutic hypothermia,ventricular fibrillation
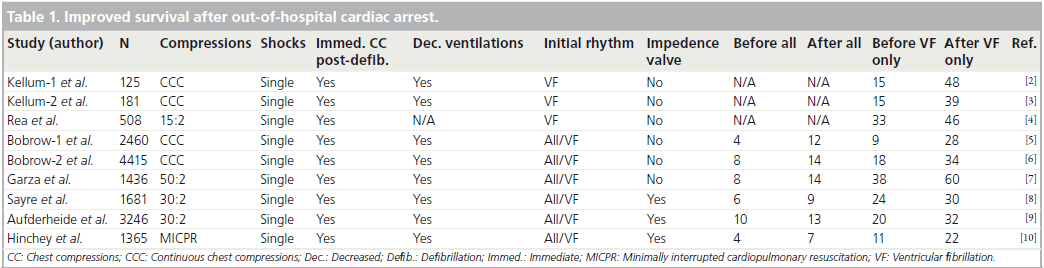
Sudden cardiac arrest continues to be a major public health problem in the industrialized world. An estimated 300,000 such deaths occur in the USA each year alone. Remarkable improvements in survival have finally begun to occur in the last decade after nearly 40 years of consistently poor rates of only 2–5% survival [1]. New emphasis on uninterrupted chest compressions, timely defibrillation, immediate chest compressions post-defibrillation, delayed endotracheal intubation and avoiding hyperventilation has improved resuscitation from out-of-hospital cardiac arrest in a number of communities [2–10]. Although all of these reports were historically controlled rather than randomized, the consistent improvement in outcome is striking (Table 1).
Post-resuscitation care
With increasing numbers of patients being resuscitated and admitted to the hospital, the opportunity for improving neurologically favorable long-term survival has focused increased attention on post-resuscitation care.
Post-resuscitation care went from an interesting but nebulous concept, to a more formalized pragmatic approach in 2007 after the report of Sunde et al. [11]. These resuscitation researchers from Oslo, Norway, noted a wide variation in regional hospital survival-to-discharge rates after successful out-of-hospital resuscitation. In response, they implemented a new standard operating procedure for in-hospital post-resuscitation treatment. This procedure required that each post-cardiac arrest patient be considered for therapeutic hypothermia, emergent coronary angiography, percutaneous coronary intervention (PCI), hemodynamic support, aggressive control of hyperglycemia and early weaning from mechanical ventilation [11]. They compared survival at 1 year, both before and after instituting this new approach to post-resuscitation care. Survival doubled with the new approach. Of all the components in their new operating procedure, early coronary angiography with PCI was the factor most associated with improved longterm survival (OR: 4.5; CI: 1.6–12.5). Recently, this same group has published an update of its experience and report identical results after 5 years [12]. They expanded their original report to include a total of 248 patients resuscitated during the period of 2003 to 2009. The good news is that aggressive post-resuscitation care continued to produce better long-term neurologically intact survival-to-discharge. A survival rate of 56% observed in their original report, was found again after 5 years of their program. This provides convincing evidence that, although this study was neither randomized nor prospectively controlled, their original experience of clinical improvements were not merely Hawthorne effect, but rather were real and sustainable. Most importantly, of those who survived, 93% had favorable neurological function, giving re-assurance that such improvements in survival are not at the expense of patient independence or cognitive function.
Feasibility & safety of performing coronary angiography post-resuscitation
Can coronary angiography and PCI be accomplished in the newly resuscitated victim of outof- hospital cardiac arrest? In this critical and sometimes unstable peri-arrest period, is an invasive cardiac evaluation strategy important enough to take priority over other potential therapies and evaluations? That it can be done is clear, but whether it should be done remains more controversial. Some believe that an invasive interventional strategy is too costly for wide application and will not be effective, since the major source of poor outcomes post-resuscitation is neurological injury [13].
Kahn et al. published in 1995 the first report of primary angioplasty for patients with out-ofhospital cardiac arrest who survived to emergency room admission with ECG evidence of an ST elevation myocardial infarction (STEMI) [14]. This small series of 11 patients showed that acute coronary angiography and percutaneous transluminal coronary angioplasty (PTCA) were feasible post-resuscitation. Six of 11 patients survived long-term and all six survivors had favorable neurological outcomes. Scant details are provided, but the authors do not comment on any undue delays or interference with other post-resuscitation treatments. Spaulding et al. published their moderately large experience in 84 consecutive patients resuscitated from outof- hospital cardiac arrest where there was ‘no obvious noncardiac’ etiology [15]. They performed immediate coronary angiography in all 84 patients and attempted angioplasty in 37 of them. A total of 60 out of 84 patients had clinically significant coronary disease found at angiography, nearly 50% (40/84) having a total occlusion. No specific comment of immediate coronary angiography displacing other pressing therapies is mentioned, but rather the advantages of acutely identifying unstable coronary lesions is extolled. From these early reports, the feasibility and acute safety of immediate coronary angiography and potential PTCA seems reasonable. Continued experience has proven these earlier assumptions to be true and valid.
Identifying a culprit lesion responsible for triggering sudden cardiac arrest is the primary reason for considering urgent coronary angiography after resuscitation. Such lesions, particularly acute thrombotic occlusions, require emergent revascularization to preserve myocardial function and to provide optimal long-term outcome. Urgent coronary angiography can reveal other important clinical information, including the extent of chronic stable coronary disease, current status of left ventricular function and other nonatherosclerotic potential causes of cardiac arrest. We published a series of cardiac catheterization findings in resuscitated patients that included one patient with a previously unknown nonischemic cardiomyopathy and another patient with a congenitally absent left main coronary artery [16]. Other important data can be obtained during urgent cardiac catheterization postresuscitation. Invasive hemodynamic monitoring can reveal the need for inotropic therapy. Insertion of an intra-aortic counterpulsation balloon pump can be accomplished during this time in the catheterization suite. Likewise, the placement of an intravascular temperature management catheter can be performed and post-resuscitation therapeutic hypothermia commenced.
However, some have remained concerned about an invasive interventional strategy displacing other important issues in timely treatment of the post-cardiac arrest victim; for example, the need to perform an emergent head CT scan to rule out subarachnoid bleeding as a cause of cardiac arrest. However, Mitsuma et al. have found that certain clinical and cardiac characteristics can help identify the subgroup of out-of-hospital cardiac arrest victims who may need head CT scans to rule out subarachnoid hemorrhage [17]. Their experience suggests that those suffering cardiac arrest, secondary to a subarachnoid hemorrhage, always had a nonventricular fibrillation (non-VF) initial cardiac arrest rhythm with either some ST abnormality or QT prolongation on their post-resuscitation 12-lead ECG. Hence, others without these features do not need any serious consideration for CT scanning post-resuscitation. Indeed, some believe that the Japanese experience, with subarachnoid bleeding as a common cause of cardiac arrest, is unique and not reproduced in other countries and cultures.
When should an invasive interventional strategy post-cardiac arrest be undertaken?
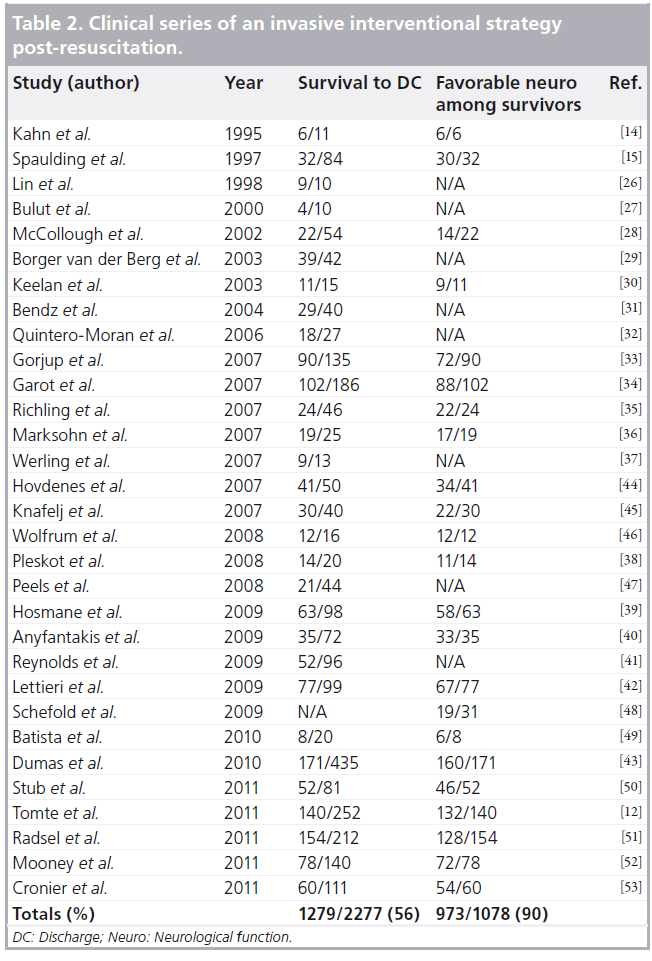
If such an approach is feasible and safe, when should it be performed? Must it be ‘immediate’ and ‘emergent’ or is ‘urgent’ and ‘prior to discharge’ adequate? Should one delay such cardiac-oriented acute therapy until central nervous system prognosis and outcome is more certain? These are all important questions and issues. The premise supporting an ‘immediate’ approach is the importance of identifying and intervening in cases where acute coronary syndromes led to the catastrophic occurrence of outof- hospital cardiac arrest. An acutely occluded major coronary artery should be reperfused in a timely fashion, whether or not it is associated with cardiac arrest. Data is now overwhelming that both long-term outcome and myocardial salvage is improved with timely perfusion of acutely occluded coronaries [18–21]. If helpful in the nonarrested patient, timely reperfusion should be even more so for the patient who has had the additional insult of global ischemia, secondary to total loss of circulation with cardiac arrest. Global myocardial stunning, resulting in depression of systolic and diastolic ventricular dysfunction, is well described after cardiac arrest [22–25]. Add to that global ischemic burden the ongoing regional ischemic insult of an acutely occluded major epicardial coronary and it should not be surprising that cardiogenic shock is frequent in the post-resuscitated. Under such circumstances, the necessity of immediate or emergent coronary angiography and intervention becomes obvious. Waiting until the next morning is not acceptable for the patient with a myocardial infarction (MI) caused by an acutely occluded coronary, regardless of whether they have had cardiac arrest. But what about the concern that fixing the heart without first knowing the neurological prognosis could lead to increased numbers of surviving, but significantly brain-damaged individuals? The data demonstrate just the opposite. A total of 32 clinical series have been reported of utilizing an invasive interventional approach immediately after resuscitation from out-of-hospital cardiac arrest (Table 2) [12,14,15,26–54]. In 2387 post-arrest patients, some awake and some comatose at coronary angiography, 56% survived and 90% of those survivors had neurologically favorable cerebral performance categories 1 or 2 upon hospital discharge. It is recognized that there are two distinct populations in this summary, those who were awake at the time of coronary angiography post-arrest and those who remained comatose after restoration of spontaneous circulation. However, the exact details are rarely given, in order to successfully separate such populations from the current reports. Nevertheless, combining these post-resuscitation patients presents a very high-risk group for an invasive interventional approach (perhaps the highest) and more than 40% will expire, including some who will die from neurological injury. But if they survive, their chance for good neurological recovery is excellent. It is simply not true that an aggressive, invasive interventional approach will simply fill up skilled nursing facilities with significantly brain-damaged post-cardiac arrest patients.
Who among the post-resuscitated should undergo immediate coronary angiography?
It is easier to prospectively identify those who should not have immediate coronary angiography than who should. Patients who have an obvious noncardiac cause for their sudden death need not be immediately taken to the cardiac catheterization suite. Those whose cardiac arrest was associated with drowning, asphyxiation or trauma are not good candidates for an invasive approach. Those whose resuscitation was exceedingly lengthy, requiring numerous shocks and multiple doses of vasoactive medications, are not typically benefited by an invasive interventional strategy. Finally, those who are not candidates for further aggressive therapies should not be taken for emergent coronary angiography or intervention.
Post-resuscitated patients whose cardiac arrest was precipitated by an acute coronary event are the most likely to benefit from an invasive interventional strategy, including emergent coronary angiography and PCI. How to accurately identify that subgroup is the difficulty. In the nonarrested acute coronary syndrome population, the ECG is the gold standard in determining who should undergo emergent invasive evaluation and who can be initially treated medically, with elective coronary angiography at a later time. If ST elevation is present, emergency angiography is recommended. If no ST elevation is present, medical stabilization before cardiac catheterization is appropriate. Acute coronary syndrome patients with ST depression or T-wave inversions, but not ST elevation, generally do not require emergent coronary angiography unless medically refractory symptoms persist. An urgent (within 24 h of admission) rather than emergent time course for coronary angiography seems optimal for these patients [55]. Unfortunately, it is not quite so simple postresuscitation. These acute coronary syndrome guidelines based on clinical symptoms and ECG findings were formulated from randomized trials excluding all cardiac arrest patients. Indeed, prearrest symptoms and post-resuscitation ECG findings have been found not to be as helpful in determining who needs emergent coronary angiography and intervention and who could wait 12–24 h for such studies. Spaulding et al. concluded from their experience in the postcardiac arrest patient, that pre-arrest chest pain and post-arrest ECG ST elevation were poor predictors of angiographically proven acute coronary occlusion. They noted that among the 84 consecutive post-cardiac arrest patients they studied at cardiac catheterization, nine (11%) had no ST elevation or chest pain, but were found to have an acutely occluded coronary artery [15]. The authors concluded that ‘acute coronary-artery occlusion is therefore difficult to predict in survivors of out-of-hospital cardiac arrest on the basis of clinical and ECG data alone. Immediate coronary angiography could therefore be warranted on this basis alone.’
ST segment elevation post-cardiac arrest
Though the absence of ST elevation post-resuscitation clearly does not rule out an acutely occluded or unstable culprit coronary lesion, the presence of this ECG finding is helpful in indentifying those likely to have such. Though some false-positive issues have been identified with ST elevations, such as a left ventricular aneurysm or pericarditis, these are even less likely to appear as the cause of out-of-hospital cardiac arrest. Most of the clinical series supporting the invasive approach post-cardiac arrest have been in patients with ST elevation on their post-resuscitation ECG.
Gorjup et al. found among 2393 consecutive STEMI patients that 6% suffered cardiac arrest and were resuscitated [33]. Among the 135 STEMI patients suffering cardiac arrest, onethird regained consciousness and two-thirds remained comatose during their initial evaluation including emergent coronary angiography. Characteristics of their cardiac arrest and resuscitation effort associated with awakening before coronary angiography included emergency medical system witnessed arrest, short time to advanced cardiac life support, resuscitation requiring only defibrillation, less use of adrenaline and shorter time to return of spontaneous circulation. Following an invasive intervention strategy for those resuscitated, whether awake or comatose, the survival rate was 69%, with 80% of all survivors being neurologically intact.
Garot et al. from France reported on 186 patients with acute MIs complicated by out-of-hospital cardiac arrest [34]. A total of 54% were alive at 6 months with 86% of survivors having no neurological sequelae. They also found that shorter intervals between the onset of cardiac arrest and the beginning of cardiopulmonary resuscitation (CPR), to defibrillation and to return of spontaneous circulation were associated with improved 6-month outcome.
Hosmane et al. examined outcomes among 98 consecutive STEMI patients resuscitated from cardiac arrest, regardless of time to return of spontaneous circulation and neurological status [39]. Predictors of neurologic recovery included shorter time to return of spontaneous circulation, non-coma post-arrest, and younger age. A total of 96% of those conscious before post-resuscitation coronary angiography survived, as did 93% of those even minimally responsive before angiography, while those remaining comatose at cardiac catheterization had only a 44% survival rate. The good news is that 88% of those who survived had full neurological recovery. The overall survival rate for their group of 98 patients was 64%, with 92% of their survivors being fully independent in daily living activities, suggesting favorable neurological recovery.
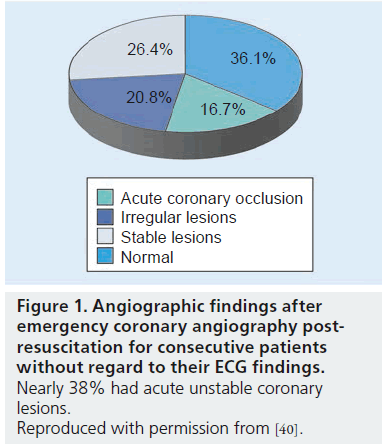
Anyfantakis et al., from France and Greece, performed systematic emergency coronary angiography in 72 consecutive survivors of out-ofhospital cardiac arrest, irrespective of the postarrest ECG [40]. Survival to hospital discharge was achieved in 49%, with 94% of survivors having no neurological sequelae. In total, 39% had ST segment elevation, while 61% did not. Among those without ST elevation, a one-third had ST depression, a quarter had left bundle branch block (BBB), another quarter had nonspecific ST changes and nearly 20% had a normal post-resuscitation ECG. Most interestingly, by performing coronary angiography in all patients, without regard to their ECG findings, they identified acute thrombosis or irregular lesions suggestive of ruptured plaque or thrombus in 38% (Figure 1).
Figure 1: Angiographic findings after emergency coronary angiography postresuscitation for consecutive patients without regard to their ECG findings. Nearly 38% had acute unstable coronary lesions. Reproduced with permission from [40].
Lettieri et al., on behalf of the Lombard IMA study group, prospectively collected data on 2617 consecutive patients with STEMI, of whom 99 were resuscitated after out-of-hospital cardiac arrest [42]. In-hospital mortality was seven-times higher in those resuscitated than those not experiencing cardiac arrest (22 vs 3%; p < 0.0001). Independent predictors of in-hospital mortality included long time from call to emergency medical system and starting CPR, non-VF cardiac arrest, cardiogenic shock and a Glasgow Coma Scale score of 3 on admission. The composite of death, recurrent MI and revascularization at 6 months was not different between those surviving the hospital phase after being resuscitated and those not experiencing cardiac arrest.
Several recurrent themes are apparent from these reports of an invasive interventional strategy in STEMI patients resuscitated from out-ofhospital cardiac arrest. First, a long-term survival rate of over 50% can be achieved in such patients undergoing immediate coronary angiography upon admission and subsequent PCI, if needed. Second, consistent predictors of poor outcome, even with an aggressive invasive approach to post-resuscitation care, include lengthy times from cardiac arrest to definitive treatments and restoration of a spontaneous circulation, non-VF cardiac arrest and coma at the time of angiography. Finally, if the post-resuscitated survive to hospital discharge, their long-term neurological status is excellent in nearly 90% of cases. This is the exact opposite of the common fear that with an aggressive cardiac treatment, particularly among those with persistent coma upon admission, ‘hearts will be saved but not brains.’ The data simply do not support this viewpoint and fear.
Invasive interventional approach combined with therapeutic hypothermia for STEMI patients resuscitated from out-of-hospital cardiac arrest
Combining systemic mild therapeutic hypothermia with an invasive interventional approach to the successfully resuscitated STEMI patient makes good sense if it can be logistically accomplished. With minimum effort, both can be performed without undue delays or safety concerns. Initial concerns that hypothermia might worsen those with cardiogenic shock now seem resolved. Some worried the technique for hypothermia induction, specifically rapid intravenous infusion of ice cold saline (30 ml/kg or ~1–2 l for most patients), might be an issue for STEMI patients resuscitated from cardiac arrest. Preliminary data suggest that such volume loading during hypothermia induction does not increase pulmonary edema or other harmful side effects, even during a STEMI, though most in this study did not receive the full 2 l of cold saline as initially planned [56]. The advantage of combining both of these potent post-resuscitation therapies is that together they optimize the recovery of both the CNS and the myocardium. Though preliminary at best, there are accumulating data suggesting that mild hypothermia not only improves neurological function, but also post-resuscitation myocardial function [57–59]. Likewise, it is possible that reperfusing an acutely occluded coronary artery not only salvages myocardium, but the resultant improved left ventricular function may help an injured CNS as well.
There are numerous reports over the last year of combining an invasive interventional strategy with induction of systemic therapeutic hypothermia for those resuscitated from out-of-hospital cardiac arrest, but who remain comatose upon arrival at the hospital.
Dumas and Spaulding recently published their updated experience with this approach [43]. A coronary angiogram was performed on admission in 435 out-of-hospital cardiac arrest patients with no obvious extracardiac cause for their arrest. Approximately 30% (n = 134) had ST elevation on their post-resuscitation ECG; the other 70% (n = 301) had a variety of non- ST elevation patterns. If not contraindicated, mild therapeutic hypothermia was implemented at hospital admission, with more than 80% receiving hypothermia. Hospital survival was 40%, with 94% of survivors having favorable long-term neurological function.
Stub et al. performed a single-center review of 125 patients resuscitated from 2002–2003 (controls) and 2007–2009 (contemporary cohort receiving both therapeutic hypothermia and early coronary intervention) [50]. Their contemporary combination of hypothermia and early coronary intervention resulted in significantly better survival to discharge (64 vs 39%; p = 0.01) and more intact neurological function among survivors (88 vs 76%; p < 0.01). They concluded that contemporary post-resuscitation management, including therapeutic hypothermia and early coronary intervention, is associated with significant increases in survival to hospital discharge and intact neurological function among survivors.
Mooney et al. at Minneapolis Heart Institute (MN, USA) utilized their established regional STEMI network to provide coordinated postresuscitation care, including therapeutic hypothermia, for any resuscitated patient remaining unresponsive after restoration of spontaneous circulation [52]. They reported on 140 out-ofhospital cardiac arrest patients, three-quarters (n = 107) of whom were transferred to the therapeutic hypothermia-capable hospital from the referring network hospitals. Patients with non- VF cardiac arrest or cardiogenic shock were included. Patients with concurrent STEMI (n = 68) received emergent coronary angiography and intervention while being cooled. Overall survival to hospital discharge was 56%, with 92% of survivors having good neurological function. No differences in outcomes were noted between transferred and nontransferred patients. Delaying the initiation of hypothermia resulted in worse outcomes, such that for every hour of delay the risk of death increased by 20%. These authors noted that an established system of care, in this case a regional STEMI network of 33 hospitals, can be further developed into a post-resuscitation care network, extending lifesaving therapeutic hypothermia to many additional cardiac arrest victims. They noted that the application of simple ice packs in the prehospital setting was incrementally life-saving for those requiring transfer to the therapeutic hypothermia-capable receiving medical center. Among those with STEMI receiving both hypothermia and coronary angiography ± PCI, the overall survival rate was 65%.
Cronier et al. from France recently reported their experience with 111 consecutive patients resuscitated following out-of-hospital cardiac arrest [53]. All had VF as their initial rhythm, 45% had an ST elevation on their ECG, while 55% did not. Mild hypothermia was provided to 86% of the patients. A total of 54% survived to hospital discharge, with 90% of survivors having good neurological outcomes. Approximately half of all patients had PCI for an angiographically identified culprit lesion suspected of causing their cardiac arrest. Subdividing their study population by age, they found no significant differences in outcomes among those less than 75 years of age. The number of patients older than 75 years was too small for meaningful comparison.
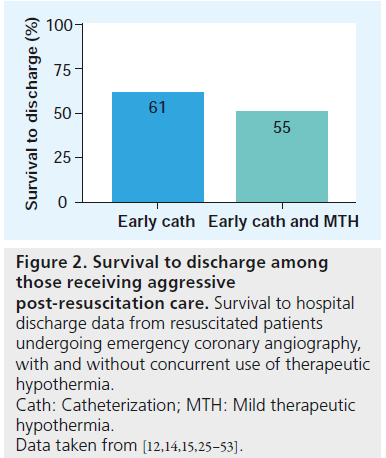
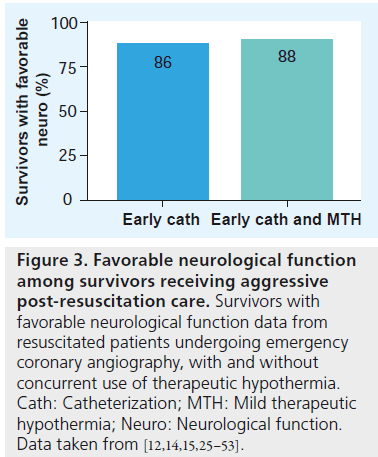
These most recent reports of combining therapeutic hypothermia and an invasive interventional approach to early post-resuscitation care show good outcomes, similar to the previous experience before the use of hypothermia. Overall survival rates were 54%, with 91% of survivors having good neurological function (Figure 2). At first glance, these results might seem disappointing since they are not different from the era before the use of hypothermia (overall survival of 59%, with 88% of survivors neurologically intact) (Figure 3). Why is the combination not better? Remember that only those who remain comatose receive hypothermia, so any patient receiving both must have been unresponsive at the time of admission and at coronary angiography. Those who are responsive at admission have a much better prognosis than those who are comatose. Achieving the same outcomes in these higher risk comatose patients with the combination of hypothermia and intervention suggests real improvement for the patient subgroup most likely not to do well.
Figure 2: Survival to discharge among those receiving aggressive post-resuscitation care. Survival to hospital discharge data from resuscitated patients undergoing emergency coronary angiography, with and without concurrent use of therapeutic hypothermia. Cath: Catheterization; MTH: Mild therapeutic hypothermia. Data taken from [12,14,15,25–53].
Figure 3: Favorable neurological function among survivors receiving aggressive post-resuscitation care. Survivors with favorable neurological function data from resuscitated patients undergoing emergency coronary angiography, with and without concurrent use of therapeutic hypothermia. Cath: Catheterization; MTH: Mild therapeutic hypothermia; Neuro: Neurological function. Data taken from [12,14,15,25–53].
Invasive interventional approach for the post-resuscitated without ST elevation MI
The data are convincing that optimal care of the STEMI patient resuscitated from cardiac arrest includes emergent coronary angiography and therapeutic hypothermia if neurologically unresponsive. But what if there is no ST elevation on the post-resuscitation ECG? It is well understood that the absence of ST elevation on the post-resuscitation ECG does not guarantee a normal, disease-free coronary system [15]. Therefore, should patients without ST elevation also be treated with both hypothermia and emergent cardiac catheterization, and possibly PCI? Certainly such patients should be considered for therapeutic hypothermia if they are comatose after restoration of spontaneous circulation. However, could they also benefit from emergent coronary angiography and potential PCI?
The report by Dumas on 435 cardiac arrests taken directly to coronary angiography upon resuscitation (from the PROCAT registry), found no differences in age, initial rhythm, or other common risk factors between those with ST elevation (n = 134) and those without ST elevation (n = 301) [43]. Those without ST elevation had a variety of ECG findings including ST depression (29%), conduction abnormalities (20%), nonspecific changes (9%) and no abnormalities (11%). Significant coronary lesions were found in 58% of those without ST elevation and nearly half of these had PCI (78/176). Hospital survival was significantly higher in patients with successful PCI versus those having no or unsuccessful PCI. This was true for patients with and without ST elevation. Multivariable analysis showed successful PCI to be an independent predictor of good outcome, regardless of the initial post-cardiac arrest ECG pattern. These investigators concluded that immediate PCI (combined with therapeutic hypothermia) results in improved survival for out-of-hospital cardiac arrest patients with no obvious noncardiac cause, regardless of whether their ECG manifests ST elevation.
Radsel et al. in Slovenia studied 335 consecutive patients resuscitated from out-of-hospital cardiac arrest [51]. Approximately 53% had ST elevation, while 47% had no ST elevation on the post-resuscitation ECG. Approximately onethird of those without ST elevation underwent urgent coronary angiography, based on clinical suspicion of an acute coronary event. Patients with obvious nonischemic causes for cardiac arrest and those judged to have no realistic hope for neurologic recovery did not undergo coronary angiography. Obstructive coronary lesions considered to be acute were found in 89% of those with ST elevation on their ECG and in 24% in those without ST elevation. They concluded that although ST elevation on the post-resuscitation ECG was more likely to have an acute culprit lesion, that nearly 25% of all patients without ST elevation had the same; hence, urgent coronary angiography and PCI is reasonable for all post-resuscitated patients deemed to have a likely cardiac etiology for their arrest.
In a report from Cronier et al. 50 patients had ST elevation and 61 patients did not [53]. Survival was similar for both groups (54 vs 56%). More patients with ST elevation underwent emergency coronary angiography (94 vs 72%) and more received PCI (79 vs 20%). Though no specific angiographic details are provided, they found that one out of five resuscitated patients without ST elevation had a culprit lesion requiring acute PCI.
How to best select those for an invasive interventional approach
The incidence of acute thrombotic occlusion is higher in patients with ST elevation than in those without ST elevation on their post-cardiac arrest ECG. However, a reasonable number of patients without ST elevation have similarly unstable lesions, including some with an acute coronary occlusion. The major issue is the following: what proportion of post-arrest patients having an acutely occluded coronary, but without ST elevation, are sufficient to proceed with coronary angiography, for all to avoid missing those needing emergent PCI? Is 20–30% enough to submit all to emergent coronary angiography? That is in fact the percentage the post-resuscitation literature suggests, namely one-fourth to one-third of those without ST elevation will have an occluded vessel or an unstable high-grade culprit coronary lesion. A growing number of interventional cardiologists think this is too many to leave without timely reperfusion and are therefore committed to performing emergent coronary angiography for anyone successfully resuscitated from out-of-hospital arrest thought to be cardiac in etiology. However, others are still looking for a more specific way to identify those post-cardiac arrest patients most likely to have an unstable or thrombotic coronary.
Recently, another group in France has suggested that any ST elevation, ST depression, or conduction abnormality (wide QRS complex such as a left BBB, right BBB or nonspecific BBB) is better at identifying post-cardiac arrest patients with culprit coronary lesions [60]. In a series of 165 consecutive patients with sustained return of spontaneous circulation after out-of-hospital cardiac arrest (84 with shockable rhythms, 73 with nonshockable rhythms), ECG abnormalities were tracked for predicting acute coronary lesions with thrombus or ruptured plaques. The best predictive value resulted from combining all three of these ECG findings. The combined criterion of either ST elevation, ST depression or wide QRS provided a sensitivity of 100%, while specificity was 46%. In this series, all patients with acute ischemic unstable culprit coronary lesions were successfully predicted by using this combined ECG criteria. They noted that if these combined ECG criteria were used to decide who should have emergent coronary angiography, 30% of their population would not have undergone the procedure, yet none of them had an identifiable culprit lesion. This approach is promising, but our own experience suggests there are some acute lesions, even acute coronary occlusions, that are associated with normal 12-lead ECGs post-resuscitation.
Our experience at the University of Arizona Sarver Heart Center (AZ, USA) [16] differs somewhat from that of Siderais et al. We are convinced of the importance of early coronary angiography and potential PCI in almost all patients resuscitated from out-of-hospital cardiac arrest, regardless of whether their post-arrest ECG is abnormal or not. We published a small series of cases from our experience at the Sarver Heart Center, where no ST elevation was present on the postcardiac arrest ECG [16]. None of the five patients had evidence of ST elevation on the ECG postresuscitation. Two of the five had totally normal ECGs post-resuscitation, but evidence for sinus tachycardia. All were thought to have a likely cardiac cause for their arrest. Important information was obtained at cardiac catheterization for each patient’s clinical care. Two patients showed acute thrombotic occlusion of a major coronary vessel, though they were both electrically ‘silent’, with no ST elevation whatsoever. One case was a significant congenital coronary anomaly, with an absent left main coronary artery; the left anterior descending artery and circumflex artery filling by small right-sided anomalous acute marginal vessel. This patient underwent successful coronary artery bypass surgery with a good result. One case involved a patient with a high-grade, unstable mid-left anterior descending artery lesion. The final patient had normal coronaries, but a significant, though previously unknown, hypertensive cardiomyopathy was diagnosed. These five cases illustrate the importance of early coronary angiography in successfully resuscitated victims of out-of-hospital cardiac arrest, even if no ST elevation or other ST abnormalities are seen on their post-resuscitation 12-lead ECG.
Why aren’t more adopting an invasive interventional strategy for the post-resuscitated?
Some simply are not yet convinced the data supports such an approach. They argue that the initial studies were small and highly selective, thereby failing to be representative of the usual post-cardiac arrest population [13]. However, since the first early reports the accumulation of additional supportive data is impressive, with nearly 2400 patients now reported in the literature. Although the data to date are not randomized, the consistency of the survival benefits and the excellent neurological function of such survivors is astounding, especially given the different countries and healthcare systems finding similar positive results.
The current 2010 CPR and Emergency Cardiovascular Care (ECC) guidelines, including those of the American Heart Association and the European Resuscitation Council, recommend emergent coronary angiography in all STEMI patients (conscious or comatose postcardiac arrest) and specifically note that similar angiography may be reasonable even in the absence of STEMI, due to the high incidence of acute coronary ischemia as a trigger of cardiac arrest [61]. The ERC guidelines specifically state that, ‘an invasive coronary intervention should be considered in all post-cardiac arrest patients who are suspected of having coronary artery disease [62]. The importance of these recommendations is highlighted by the advice that emergency medical services may bypass a nearby hospital without PCI facilities if the delay seems acceptable (<20–30 min). Hence, the current guidelines clearly emphasize an early invasive/ interventional strategy for the post-resuscitated is the appropriate and preferred approach.
A second significant reason many have been reluctant to begin using an invasive interventional post-resuscitation strategy, at least in the USA, involves the concern about public reporting of specific outcomes data. Some interventional cardiologists and their respective medical centers are afraid of being maligned if their PCI survival rates drop from including these very sick postcardiac arrest patients. Although a 55% overall survival rate among those resuscitated from out-ofhospital cardiac arrest is twice the historical rate, nearly half of such patients still die. Currently accepted definitions used in public reporting of outcomes for comparing medical centers and individual providers would count such deaths in their data on PCIs. These deaths, even if secondary to multiorgan or CNS failure, are tabulated as PCI deaths, since the patient had a PCI during that hospitalization. It is crucial that such patients are recognized for what they are – the sickest of the sick and an extremely high-risk group. Maynard et al. compared outcomes among 16,000 consecutive PCI patients in the entire state of Washington [63]. Those PCI patients who had suffered out-of-hospital cardiac arrest prior to their PCI, were 19-times more likely to die than the standard elective PCI patient.
Ellis et al. recently published a new, enhanced STEMI risk adjustment algorithm that better accounts for noncardiac causes of mortality after primary percutaneous intervention [64]. The authors note that more than 50% of postprocedural deaths result from these noncardiac comorbidities. They argued that current risk assessment for patients undergoing PCI would be greatly enhanced by incorporating certain noncardiac comorbidities into our current algorithms. This is a crucial and much needed step if the present systems for public disclosure of quality and outcome data are to be accurate, and to allow meaningful comparisons.
The authors specifically highlighted STEMI patients resuscitated from sudden cardiac death as a subgroup whose post-PCI mortality is high, but is greatly influenced by noncardiac factors, not the PCI procedure itself. Appropriate risk adjustment of expected mortality for such post-cardiac arrest patients undergoing emergent primary PCI is a crucial step whose time has clearly arrived.
These authors state that current public reporting of mortality data for PCI does not adequately adjust for this highest risk subgroup. Interventionalists willing to provide the best possible outcomes for those suffering cardiac arrest with their STEMI are penalized with higher than expected mortality rates, while their peers who avoid intervention in such high-risk patients are ‘rewarded’ statistically for withholding potentially beneficial care. This is counterproductive to providing optimal patient care. Interventional cardiologists and their medical centers should be able to do what is best for the individual STEMI patient resuscitated from cardiac arrest, without fear of unfair inflation of their overall reported mortality figures.
In an editorial concerning PCI in the postresuscitated, McMullan and White addressed the need for reclassifying this highest risk subgroup receiving coronary angiography and PCI [65]. These authors note that public reporting of procedural outcomes is intended to facilitate informed decisions by patients and families, but can also lead to some physicians and institutions avoiding interventions in the highest risk patients, for fear of bad outcomes and subsequent bad public report cards. Such decisions can deny important therapeutic options to the very population most likely to benefit from these procedures, namely the sickest patients. They note, “the interventional cardiologist, when faced with the care of a patient resuscitated from cardiac arrest, should not be forced to decide between protecting his publically reported reputation and doing what he feels is best for the patient.” They suggest that post-cardiac arrest patients should be categorized separately as ‘compassionate use’ for PCI and not included in overall mortality calculations for hospitals or individual physicians. Hospitals which excel in providing therapeutic hypothermia and early intervention should be highlighted as centers of excellence, not inaccurately labeled by flawed public reporting systems as “poorly performing centers with excessive mortality rates.”
Future perspective
Post-resuscitation care will continue to be more and more emphasized to improve long-term outcomes following cardiac arrest. Anyone fortunate enough to be resuscitated from out-of-hospital cardiac arrest from a likely cardiac complication should be considered for emergent coronary angiography, and if comatose they should receive concurrent therapeutic hypothermia. Such an approach is clearly compatible with the most recent 2010 CPR and ECC guidelines. Immediate neurological status post-resuscitation should not deter the use of emergent coronary intervention, since waiting will result in loss of opportunity to provide timely reperfusion. It seems likely that techniques to provide intra-arrest cooling will be realized, providing the possibility of limiting myocardial infarct size, while at the same time preserving neurological function in those suffering cardiac arrest during an STEMI. Randomized control trials of emergent coronary angiography in those resuscitated without ST elevation could help determine the optimal strategy for this controversial subgroup. Finally, the optimal approach to provide this important care to victims of cardiac arrest will require designation of cardiac arrest centers that are prepared to provide such emergent care 24 h a day/7 days per week.
Financial & competing interests disclosure
The author has received consulting fees as a member of scientific advisory boards from Zoll Inc. and Physio-Control Inc. Both are medical device companies with defibrillation, temperature management and cardiopulmonary resuscitation mechanical devices or systems. He has also received an unrestricted research grant from Laerdal Inc. during the period of 2008–2010. The author has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Post-resuscitation care is an important link in the chain-of-survival
▪▪ Future improvements in long-term neurologically intact survival will result from better post-resuscitation care.
▪▪ Requires a multidisciplinary approach, including the involvement of the interventional cardiologist.
Immediate coronary angiography & intervention post-resuscitation is safe & effective
▪▪ Individuals resuscitated from cardiac arrest of cardiac etiology benefit from timely coronary angiography/intervention.
▪▪ Neurological status immediately post-resuscitation should not deter aggressive cardiac care, including percutaneous coronary intervention (PCI).
▪▪ Combining PCI and mild therapeutic hypothermia in comatose, post-resuscitated, of out-of-hospital cardiac arrest victims, saves lives and preserves cognitive function.
▪▪ Long-term survival rates are doubled with successful PCI after resuscitation.
▪▪ Favorable neurological outcomes are observed in 80–90% of those receiving aggressive post-resuscitation care.
Post-resuscitation 12-lead electrocardiogram
▪▪ ST elevation is helpful in identifying who has a likely acute coronary etiology for the cardiac arrest.
▪▪ However, lack of ST elevation does not rule out a coronary event as cause of arrest.
▪▪ Early coronary angiography should be considered for anyone who do not have an obvious noncardiac cause of their arrest.
PCI for the post-resuscitated should be considered compassionate use & not tabulated with elective PCI outcomes
▪▪ Expected mortality in post-resuscitation PCI is 20- to 40-times that observed with elective PCI.
▪▪ Public reporting systems should not combine elective and post-resuscitation PCI outcomes.
▪▪ Separate outcomes reporting, based on realistic mortality expectations, will encourage more optimal care of the post-resuscitated.
References
Papers of special note have been highlighted as:
▪ of interest
- Valenzuela TD, Kern KB, Clark LL et al. Interruptions of chest compressions during EMS resuscitation. Circulation 112, 1259–1265 (2005).
- Kellum Mj, Kennedy KW, Ewy GA. Cardiocerebral resuscitation improves survival of patients with out-of-hospital cardiac arrest. Am. J. Med. 119, 335–340 (2006).
- Kellum MJ, Kennedy KW, Barney R et al. Cardiocerebral resuscitation improves neurologically intact survival of patients with out-of-hospital cardiac arrest. Ann. Emerg. Med. 52, 244–252 (2008).
- Rea TD, Helbrock M, Perry S et al. Increasing use of cardiopulmonary resuscitation during out-of-hospital ventricular fibrillation arrest: survival implications of guideline changes. Circulation 114, 2760–2765 (2006).
- Bobrow BJ, Clark LL, Ewy GA et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA 299, 1158–1165 (2008).
- Bobrow BJ, Spaite D, Berg RA et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA 304, 1447–1454 (2010).
- Garza AG, Gratton MC, Salmone JA, Lindholm D, McElroy J, Archer R. Improved patient survival using a modified resuscitation protocol for out-of-hospital cardiac arrest. Circulation 119, 2597–2605 (2009).
- Sayre MR, Cantrell SA, White LJ, Hiestand BC, Keseg DP, Koser S. Impact of the 2005 American Heart Association cardiopulmonary resuscitation and emergency cardiovascular care guidelines on out-of-hospital cardiac arrest survival. Prehosp. Emerg. Care 13, 469–477 (2009).
- Aufderheide TP, Yannopoulos D, Lick CJ et al. Implementing the 2005 AmericanHeart Association guidelines improves outcomes after out-of-hospital cardiac arrest. Heart Rhythm 7, 1357–1362 (2010).
- Hinchey PR, Myers JB, Lewis R et al. Improved out-of-hospital cardiac arrest survival after the sequential implementation of 2005 AHA guidelines for compressions, ventilations, and induced hypothermia: the Wake county experience. Ann. Emerg. Med. 56, 348–357 (2010).
- Sunde K, Pytte M, Jacobsen D et al. Implementation of a standardized treatment protocol for post-resuscitation care after out-of-hospital cardiac arrest. Resuscitation 73, 29–39 (2007).
- Tomte O, Andersen GO, Jacobsen D, Draegni T, Auestad B, Sunde K. Strong and weak aspects of an established post-resuscitation treatment protocol-A five-year observational study. Resuscitation 82, 1186–1193 (2011).
- Skowronski GA. Cardiac arrest survivors need proof of neurological function before percutaneous coronary intervention. Crit. Care Resusc. 9, 297–298 (2007).
- Kahn JK, Glazier S, Swor R, Savas V, O’Neil Primary coronary angioplasty for acute myocardial infarction complicated by out-of-hospital cardiac arrest. Am. J. Cardiol. 75, 1069–1070 (1995).
- Spaulding CM, Joly L-M, Rosenberg A et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N. Engl.Med. 336, 1629–1633 (1997).
- Kern KB, Rahman O. Emergent percutaneous coronary intervention for resuscitated victims of out-of-hospital cardiac arrest. Catheter Cardiovasc. Interv. 75, 616–624 (2010).
- Mitsuma W, Ito M, Kidama M et al. Clinical and cardiac features of patients with subarachnoid hemorrhage presenting with out-of-hospital cardiac arrest. Resuscitation 82, 1294–1297 (2011).
- Grines CL, Browne KF, Marco J et al. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. N. Engl. J. Med. 328, 673–679 (1993).
- Gibbons RJ, Holmes DR, Reeder GS et al. Immediate angioplasty compared with the administration of a thrombolytic agent followed by conservative treatment for myocardial infarction. N. Engl. J. Med. 328, 685–691 (1993).
- Berger PB, Ellis SG, Holmes DR Jr et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction. Circulation 100, 14–20 (1999).
- Cannon CP, Gibson CM, Lambrew CT et al. Relatioship of symptom-onset-to-balloon time and door-to-ballon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 283, 2941–2947 (2000).
- Gazmuri RJ, Weil MH, Bisera J, Tang W, Fukui M, McKee D. Myocardial dysfunction after successful resuscitation from cardiac arrest. Crit. Care Med. 24, 992–1000 (1996).
- Kern KB, Hilwig RW, Rhee KH, Berg RA. Myocardial dysfunction following resuscitation from cardiac arrest: an example of global myocardial stunning. J. Am. Coll. Cardiol. 28, 232–240 (1996).
- Kern KB, Hilwig RW, Berg RA et al. Post-resuscitation left ventricular systolic and diastolic dysfunction; treatment with Dobutamine. Circulation 95, 2610–2613 (1997).
- Laurent I, Monchi M, Chiche JD et al. Reversible myocardial dysfunction in survivors of out-of-hospital cardica arrest. J. Am. Coll. Cardiol. 40, 2110–2116 (2002).
- Lin A C-M, Shyu KG, Cheng JJ, Kuan p-L, Chang H. Safety and efficacy of primary percutaneous transluminal coronary angioplasty for acute myocardial infarction complicated by prolonged cardiopulmonary resuscitation. Chinese Electronic Periodical Services 9, 145–151 (1998).
- Bulut S, Aengevaeren WRM, Luijten HJE, Verheugt FWA. Successful out-of-hospital cardiopulmonary resuscitation: what is the optimal in-hospital treatment strategy? Resuscitation 47, 155–161 (2000).
- McCullough PA, Prakash R, Tobin KJ, O’Neil WW, Thompson RJ. Application of a cardiac arrest score in pagtients with sudden death and ST segment elevation for triage to angiography and intervention. J. Interven Cardiol. 15, 257–261 (2002).
- Borger van der Berg AE, Bax JJ, Boersma E et al. Impact of percutaneous coronaryintervention or coronary artery bypass grafting on outcome after nonfatal cardiac arrest outside the hospital. Am. J. Cardiol. 91, 785–789 (2003).
- Keelan PC, Bunch TJ, White RD, Packer DL, Holmes DR. Early direct coronary angioplasty in survivors of out-of-hospital cardiac arrest. Am. J. Cardiol. 91, 1461–1463 (2003).
- Bendz B, Eritsland J, Nakstad AR et al. Long-term prognosis after out-of-hospital cardiac arrest and primary percutaneous coronary intervention. Resuscitation 63, 49–53 (2004).
- Quintero-Moran B, Moreno R, Villarreal S et al. Percutaneous coronary intervention forcardiac arrest secondary to ST elevation acute myocardial infarction. Influence of immediate paramedical/medical assistance on clinical outcome. J. Invasive Cardiol. 18, 269–272 (2006).
- myocardial infarction. Influence of immediate paramedical/medical assistance on clinical outcome. J. Invasive Cardiol. 18, 269–272 (2006).
- Garot P, Lefevre T, Eltchaninoff H et al. Six-month outcome of emergency percutaneous coronary intervention in resuscitated patients after cardiac arrest complicating ST elevation myocardial infarction. Circulation 115, 1354–1362 (2007).
- Richling N, Herkner H, Holzer M, Riedmueller E, Sterz F, Schreiber W. Thrombolytic therapy vs primary percutaneous intervention after ventricular fibrillation cardiac arrest due to acute ST segment elevation myocardial infaction and its effect on outcome. Am. J. Emerg. Med. 25, 545–550 (2007).
- Markushon E, Roguin A, Sebbag A et al. Primary percutaneous coronary intervention after out-of-hospital cardiac arrest: patients and outcomes. Isr. Med. Assoc. J. 9, 257–259 (2007).
- Werling M, Thoren AB, Axelsson C, Herlitz J. Treatment and outcome in post-resuscitation care after out-of-hospital cardiac arrest when a modern therapeutic approach was introduced. Resuscitation 73, 40–45 (2007).
- Pleskot M, Babu A, Hazukova R et al. Out-of-hospital cardiac arrests in patients with acute ST elevation myocardial infarctions in the east bohemian region over the period 2002–2004. Cardiology 109, 41–51 (2008).
- Hosmane VR, Mustafa NG, Reddy VK et al. Survival and neurologic recovery inpatients with ST segment elevation myocardial infarction resuscitated from cardiac arrest. J. Am. Coll. Cardiol. 53, 409–415 (2009).
- Anyfantakis ZA, Baron G, Aubry P et al. Acute coronary angiographic findings in survivors of out-of-hospital cardiac arrest. Am. Heart J. 157, 312–318 (2009).
- Reynolds JC, Callaway CW, El Khoudary SR, Moore CG, Alvarez RJ, Rittenberger JC. Coronary angiography predicts improved outcome following cardiac arrest: propensity-adjusted analysis. J. Intensive Care Med. 24, 179–186 (2009).
- Lettieri C, Savoritto S, De Servi S et al. Emergency percutaneous coronary intervention in patients with ST elevation myocardial infarction complicated by out-of-hospital cardiac arrest: early and medium-term outcome. Am. Heart J. 157, 569–575 (2009).
- Dumas F, Cariou A, Manzo-Silberman S et al. Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest. Circ Cardiovasc. Interv. 3, 200–207 (2010).
- Hovdenes J, Laake JH, Aaberge L, Haugaa H, Bugge JF. Therapeutic hypothermia after out-of-hospital cardiac arrest: experiences with patients treated with percutaneous coronary intervention and cardiogenic shock.
- Knafelj R, Radsel P, Ploj T, Noc M. Primary percutaneous coronary intervention and mild induced hypothermia in comatose survivors of ventricular fibrillation with ST elevation acute myocardial infarction. Resuscitation 74, 227–234 (2007).
- Wolfrum S, Pierau C, Radke PW, Schundert H, Kurowski V. Mild therapeutic hypothermia in patients after out-of-hospital cardiac arrest due to acute ST segment elevation myocardial infarction undergoing immediate percutaneous coronary intervention. Crit. Care Med. 36, 1780–1786 (2008).
- Peels HO, Jessurun GA, van der Horst ICC, Arnold AER, Piers LH, Zijlstra F. Outcome in transferred and nontransferred patients after primary percutaneous coronary intervention for ischemic out-of-hospital cardiac arrest. Catheter Cardiovasc. Interv. 71, 147–151 (2008).
- Schefold JC, Storm C, Joerres A, Hasper D. Mild therapeutic hypothermia after cardiac arrest and the risk of bleeding in patients with acute myocardial infarction. International J. Cardiol. 132, 387–391(2009).
- Batista LM, Lima FO, Januzzi Jr. JL, Donahue V, Snydeman C, Greer DM. Feasibility and safety of combined percutaneous coronary intervention and therapeutic hypothermia following cardiac arrest. Resuscitation 81, 398–403 (2010).
- Stub D, Hengel C, Chan W et al. Usefulness of cooling and coronary catheterization to improve survival in out-of-hospital cardiac arrest. Am. J. Cardiol. 107, 522–527 (2011).
- Radsel P, Knafelj R, Kocjancic S, Noc M. Angiographic characteristics of coronary disease and post-resuscitation electrocardiograms in patients with aborted cardiac arrest outside a hospital. Am. J. Cardiol. 108, 634–638 (2011).
- Mooney MR, Unger BT, Boland LL et al. Therapeutic hypothermia after out-of-hosptial cardiac arrest: evaluation of a regional system to increase access to cooling. Circulation 124, 206–214 (2011).
- Cronier P, Vignon P, Bouferranche K et al. Impact of routine percutaneous coronary intervention after out-of-hospital cardiac arrest due to ventricular fibrillation. Crit. Care 15(3), R122 (2011).
- Laish-Farkash A, Matetzky S, Oieru D et al. Usefulness of mild therapeutic hypothermia for hospitalized comatose patients having out-of-hospital cardiac arrest. Am. J. Cardiol. 108, 173–178 (2011).
- Anderson JL, Adams CD, Antman EM et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J. Am. Coll. Cardiol. 50 e1–e157 (2007).
- Kim F, Olsufka M, Longstreth WT et al. Pilot randomized clinical trial of prehospital induction of mild hypothermia in out-of hospital cardiac arrest in patients with a rapid infusion of 4 C normal saline. Circulation 115, 3064–3070 (2007).
- Tsai M-S, Barbut D, Tang W et al. Rapid head cooling initiated coincident with cardiopulmonary resuscitation improves success of defibrillation and post-resuscitation myocardial function in a porcine model of prolonged cardiac arrest. J. Am. Coll. Cardiol. 51, 1988–1992 (2008).
- Hsu C-Y, Huang C-H, Chang W-T et al. Cardioprotective effect of therapeutic hypothermia for post-resuscitation myocardial dysfunction. Shock 32, 210–216 (2009).
- Sorrell VL, Paleru V, Altbach MI et al. Mild hypothermia delays the development of stone heart from untreated sustained ventricular fibrillation-A CMR study. J. Cardiovasc. Magn. Reson. 13, 17–25 (2009).
- Siderais G, Voicu S, Dillinger JG et al. Value of post-resuscitation electrocardiogram in the diagnosis of acute myocardial infarction in out-of-hospital cardiac arrest patients. Resuscitation 82(9), 1148–1153 (2011).
- O’Connor RE, Bossaert L, Arntz H-R et al. Part 9: acute coronary syndromes: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 122(Suppl. 2) S422–S465 (2010).
- Nolan JP, Soar DA, Zideman D et al. European Resuscitation Council Guidelines for Resuscitation 2010. Section 1. Executive Summary. Resuscitation 81, 1219–1276 (2010).
- Maynard C, Rao SV, Gregg M et al. The role of out-of-hospital cardiac arrest in predicting hospital mortality for percutaneous coronary interventions in the clinical outcomes assessment program. J. Invasive Cardiol. 21, 1–5 (2009).
- Ellis SG, Shishehbor MH, Kapadia SR et al. Enhanced prediction of mortality after percutaneous coronary intervention by consideration of general and neurological indicators. J. Am. Coll. Cardiol. Intv.4, 442–448 (2001).
- McMullen PW, White CJ. Doing what’s right for the resuscitated. Catheter Cardiovasc. Interv. 76, 161–163 (2010).
▪ First study to show the importance of combining post-resuscitation coronary angiography and therapeutic hypothermia for improving both survival and neurological function of survivors.
▪ Study showed the feasibility of early coronary angiography post-resuscitation and the lack of sensitivity of ST elevation to determine culprit coronary lesions in post-cardiac arrest victims.
▪ Landmark article showing the difference in outcome after coronary angiography in those awake versus comatose post-resuscitation.
▪ Recent study showing that successful percutaneous coronary intervention, not the presence or absence of ST elevation, determines outcome post-resuscitation.
▪ Study shows that at least one in four patients without ST elevation on their postresuscitation electrocardiogram have an acute unstable coronary lesion as likely culprit.
▪ Study demonstrates that transferred and nontransferred resuscitated patients fare equally well with aggressive post-resuscitation care.
▪ Editorial by prominent interventional cardiologists calling for ‘compassionate use percutaneous coronary intervention’ for the post-resuscitated patient.