Research Article - Interventional Cardiology (2022) Volume 14, Issue 6
In patients with acute ST elevation myocardial infarction treated with primary percutaneous coronary intervention :Does the QT- Dispersion correlate with myocardial perfusion?
- Corresponding Author:
- Hatem Helmy Abdelrahman
Department of Cardiology, Assiut University, Asyut, Egypt,
E-mail: hatem19652007@yahoo.com
Received date: 05-Dec-2022, Manuscript No. FMIC-22-82231; Editor assigned: 07-Dec-2022, PreQC No. FMIC-22-82231 (PQ); Reviewed date: 21-Dec-2022, QC No. FMIC-22-82231;Revised date: 28-Dec-2022, Manuscript No. FMIC-22-82231 (R);Published date: 07-Jan-2023, DOI: 10.37532/1755-5310.2022.14(6). 598
Abstract
Abstract Background: Improvement of QT dispersion has been shown after thrombolytic therapy in the treatment of ST elevation myocardial infarction. Change in QT dispersion and myocardial reperfusion after Primary Percutaneous Coronary Intervention was not well studied before as well as its relationship with myocardial blush grade after PPCI and the occurrence of major adverse cardiac events. Aim: The current study aimed to evaluate the relationship between QT dispersion and degree of myocardial reperfusion in patients with STEMI treated by PPCI as well as its relationship with the occurrence of MACE. Patients and Methods: A prospective, study included 200 patients admitted to Assiut University Heart Hospital with STEMI underwent PPCI. Myocardial reperfusion was assessed by Thrombolysis in myocardial infarction flow grade, myocardial blush grade and corrected TIMI frame count as well as QT parameters before and after PPCI in ECG. Patients were followed up for one-year after discharge for development of MACE. Results: Out of 200 patients; 125/200 had LAD culprit and 75/200 had non-LAD culprit. There was significant decrease after revascularization in minimum QTc, maximum QT and QT dispersion, patients with LAD as culprit lesion had significantly higher maximum QTc and QT dispersion after PCI in comparison to those with non-LAD culprit lesion; 52 /200 (22.5%) developed MACE. It was noticed that QT dispersion after PPCI was higher in those who developed MACE. Conclusion: Shortening of corrected QT and QT dispersion can help as simple electrocardiographic markers in predicting successful myocardial revascularization. Changes in maximum QT are better in predicting optimum revascularization as assessed by TIMI flow grade 3 and MBG than the changes in QT dispersion. These changes can also help in predicting lower MACE after one year in STEMI patients treated by PPCI.
Keywords
STIMI • TIMI flow • MBG • QT dispersion • TIMI frame count and MACE
Abbreviations
CA: Coronary Angiography; CAD: Coronary Artery Disease; CI: Confidence Interval; cTFC: corrected TIMI Frame Count; DM: Diabetes Mellitus; ECG: Electrocardiogram; HF: Heart Failure; HTN: Hypertension; MACE: Major Adverse Cardiovascular Events; MI: Myocardial Infarction; MBG: Myocardial Blush Grade; OR: Odds Ratio; PPCI: Primary Percutaneous Coronary Intervention; QTd QT dispersion; STEMI: ST-Elevation Myocardial Infarction; SPSS: Statistical Product and Service Solutions; TIMI: Thrombolysis in Myocardial Infarction
Introduction
Worldwide, Coronary Artery Disease (CAD) is the single most frequent cause of death [1]. The main goal of therapy in ST Elevation Myocardial Infarction (STEMI) is to restore the microvascular flow and sustain the myocardial perfusion [2]. Percutaneous Coronary Intervention (PCI) increased the rate of successful recanalization of Infarct-Related Arteries (IRAs) to >90% [3]. A variety of markers including ECG and coronary angiography have been utilized to assess myocardial reperfusion [4]. Myocardial Blush Grade (MBG) is a validated measurement of myocardial perfusion [5]. The MBG was used to assess the washout of myocardial blush during angiography.
Moreover, QT-interval parameters were proposed as available non- invasive markers for assessing ventricular homogeneity as well as for predicting electrical instability. Prolongation of QT dispersion (QT-d) was utilized as the main predictor for fatal arrhythmia in patients with Myocardial Infarction (MI) [6]. QTd increases in ischemia and is affected by severity of ischemia [7]. Improvement of QT-d has been shown after thrombolytic therapy in the treatment of STEMI. Change in QT dispersion and myocardial reperfusion after PPCI was not well assessed before as well as its relationship with myocardial blush grade after PPCI as well as with the occurrence of Major Acute Cardiac Events (MACE) after PPCI [8].
Materials and Methods
This study was a prospective cohort study performed during the period from the 1st of January 2019 to the 30th of June 2019, included 200 patients presented to the emergency department at Assuit university Heart hospital with STEMI and underwent primary PCI and referred to the catheter-lab for PPCI.
Trial registration was prospectively obtained (NCT code no: 03269838). The study was conducted according to the guidelines of the Helsinki Declaration and fulfilling the CONSORT protocol. Every patient was asked to sign the consent form prior to the study commencement. All data was confidential and was used for the purpose of scientific research only. Participants had given the right and freedom to participate/withdraw at any time without any consequences.
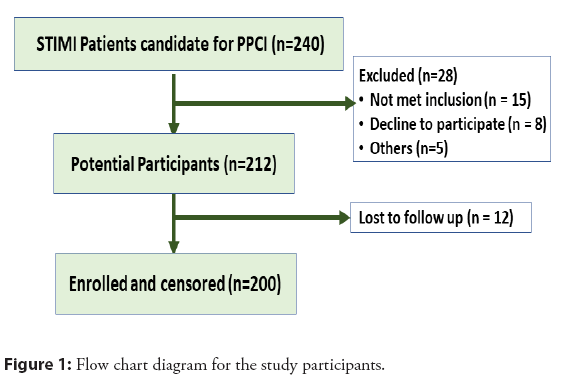
The power analysis of this study using G-Power 3.1.9.7 calculator suggested that 198 participants was sufficient to demonstrate relevant differences of 0.1 between the two groups, as regard comparing the mean QT-d for myocardial perfusion in STIMI patients underwent PCI with α error of 0.05 and power of the study of 80%. The sample was raised by 20% to compensate for dropouts and attritions shown in the Figure 1.
All patients presented to the emergency unit, Cardiology Department with STIMI and candidate for PPCI during the study period were included. On the other hand, those with prior history of MI/surgical revascularization, AF/flutter, BBB/any other intraventricular conduction abnormalities, pre-excitation on ECG, ventricular pacing rhythm, need urgent CABG or repeat PCI during a 24-hour period after the procedure, electrolyte disturbance, history of medications that may affect and QT interval could not be reliably measured in at least nine leads were excluded.
All patients were subjected to full history taking: Including age, sex, history of DM (was defined as a fasting plasma glycemic level ≥126 mg/dl [9], or treatment with oral hypoglycemic drugs or insulin injections), HTN (Hypertension was defined as a systolic BP ≥ 140 mmHg, diastolic BP ≥ 90 mmHg/on treatment with antihypertensive) as implemented by a joint task force from the European Society of Cardiology (ESC) guidelines [10], obesity (a BMI of more than or equal 30 kg/m2) [11], family history of IHD, smoking (A current smoker was defined as one who smoked at the time of PCI or had quit smoking within 1 year before MI), addiction and type of addiction, Chronic Kidney Disease (CKD) Glomerular Filtration Rate (GFR) of <60 mL/min/1.73 m2 for <3 months as stated by National Kidney Foundation [12], vascular disease, history of psychic trauma before chest pain.
Also, to assess the onset of maximum intensity of chest pain, time to first medical contact, time to balloon defined as time from chest pain onset to time of balloon inflation). The type of delay responsible for critical time loss was determined (either patient or system delays). All standard 12-lead ECGs were recorded at a paper speed of 25 mm/sec and 10 mm/mV gain [13]. Measurements of QT and RR intervals were manually performed. QT interval was measured from the beginning of the Q wave to the end of the T wave [14].
All patients had a minimum of eight ECG leads that is measurable, at least four precordial leads required for inclusion of the patient. Each patient had at least one ECG before PPCI and one after PPCI; we mainly used ECG after 48 hours after PPCI to calculate QT and QT-d. To exclude the effect of heart rates on QT intervals, QT intervals were corrected (QTc) according to Bazett’s formula (QTc=QT/square root of the RR interval in seconds) [15]. QT and QTc dispersions were defined as the difference between the maximum and minimum QT, and the maximum and minimum QTc interval measurements, respectively.
General examination including intra-procedural blood pressure and heart rate assessment. Cardiac examination to detect signs of heart failure. Chest examination: To define Killip score [16]. Echocardiography, laboratory investigations included renal functions: Serum Creatinine and urea, electrolytes (sodium, potassium, and magnesium) and cardiac enzymes Total CK, CK- MB and troponin.
Statistical analysis
Data was collected and analyzed using SPSS (Statistical Package for the Social Science, version 20, IBM, and Armonk, New York). Continuous data was expressed as mean ± SD/median (range) while nominal data was expressed as frequency (%). Χ2;-test was used to compare the nominal data of different groups while continuous data of two groups were compared with student t test while ANOVA test was used in case of more than two groups. Correlation between QTc dispersion and TIMI frame count was assessed by Pearson correlation. Level of confidence was kept at 95% and hence, p-value was considered significant if <0.05.
Results
Baseline characteristics were shown in Table 1. The mean patients’ age was 56.3 ± 11.8 years. The majority (75.5%) were males. The major risk factors were smoking (42%), DM (31.5%) and HTN (25%). Moreover, the time for pain onset ranged between 1-48 hours, time for FMC ranged between 1-240 minutes and the door to balloon was 37.1 minutes. For the clinical data, DBP ranged between 40-100 mmHg, DBP from 70 to 210 mmHg and pulse ranged between 50-140 beats/minute. The majority of cases (95.5%) were classified as Killip I (n=191) and only eight cases were Killip II-IV (4.5%). Further, the most frequent type of MI was anterior MI (62.5%) followed by inferior MI (35.5%) and posterior MI (9.5%). The mean EF% was 48.9 ± 9.4% and about half of cases (n=106) had LVSD shown in Table 2.
| Parameter | n=200 |
|---|---|
| Age (years) (mean ± SD) (Range) | 56.33 ± 11.80(22-90) |
| Male gender | 151(75.5%) |
| Cardiovascular risk factor | |
|
50(25%) |
|
63(31.5%) |
|
84(42%) |
| Onset of pain (hours) | 6.33 ± 6.16, (1-48) |
| Time to FMC (minute) | 32.09 ± 30.19, (1-240) |
| Door to balloon (minutes) | 37.1 |
| Diastolic blood pressure (mmHg) | 76.95 ± 101.3, (40-100) |
| Systolic blood pressure (mmHg) | 123.75 ± 21.67, (70-210) |
| Pulse (beat/minute) | 84.77 ± 15.78, (50-140) |
| KILLIP class | |
|
191(95.5%) |
|
1(0.5%) |
|
1(0.5%) |
|
7(3.5%) |
| Location of MI | |
|
125(62.5%) |
|
71(35.5%) |
|
19(9.5%) |
| Ejection fraction (%) | 48.87 ± 9.37 |
| Left ventricular systolic dysfunction | 106(53%) |
Table 1: Patients’ Characteristics of both study groups.
| Parameter | N=200 |
|---|---|
| TIMI flow | |
|
4(2%) |
|
11(5.5%) |
|
46(23%) |
|
139(69.5%) |
| Myocardial blush | |
|
14(7%) |
|
11(5.5%) |
|
51(25.5%) |
|
124(62%) |
| TIMI frame count | 20.28 ± 11.24 |
| Presence of other lesion | 99(49.5%) |
| Pre-dilatation | 129(64.5%) |
| Use of GPIIB/IIIA | 66(33%) |
Table 2: PPCI associated data among enrolled patients.
The effect of PPCI on the level of QT interval was presented in Table 3.
| Before PCI | After PCI | P value* | |
| Minimum QTc (ms) | 48.34 ± 1.58 | 45.75 ± 1.88 | <0.001 |
| Maximum QTc (ms) | 51.94 ± 1.52 | 47.67 ± 4.01 | <0.001 |
| QTc dispersion (ms) | 3.58 ± 1.32 | 2.15 ± 0.95 | <0.001 |
Note: *Paired sample t-test was used to compare the difference in means
Table 3: QT interval among enrolled patients before and after revascularization.
Also, QTc dispersion after PCI was significantly lower among patients TIMI flow grade 3 (1.88 ± 0.59 ms) in comparison to those with grade 2 (2.36 ± 1.02 ms), grade 1 (3.81 ± 1.07 ms) and grade 0 (4.50 ± 1.91 ms).There was significant (p<0.001) decrease in the three QT interval parameters: Minimum QTc (2.6 ms), maximum QTc (4.3 ms) and QTc dispersion (1.4 ms).
Patients with TIMI flow grade 3 had significantly lower minimum QTc after PCI (44.97 ± 1.17 ms) in comparison to grade 2 (47.13 ± 2 ms), grade 1 (48.90 ± 1.37 ms) and grade 0 (48 ± 2.30 ms). Also, maximum QTc after PCI was significantly lower among patients with TIMI flow grade 3 (46.86 ± 1.18 ms) in comparison to grade 2 (48.50 ± 7.46 ms), grade 1 (52.72 ± 1 ms) and grade 0 (52.50 ± 1 ms) as presented in Table 4.
| Before PCI | After PCI | |
|---|---|---|
| Minimum QTc (ms) | ||
|
48 ± 2.30 | 48 ± 2.30 |
|
48.90 ± 1.37 | 48.90 ± 1.37 |
|
48.32 ± 1.63 | 47.13 ± 2 |
|
48.31 ± 1.56 | 44.97 ± 1.17 |
| P value | 0.65 | <0.001 |
| Maximum QTc (ms) | ||
|
52.50 ± 1 | 52.50 ± 1 |
|
52.72 ± 1 | 52.72 ± 1 |
|
52.04 ± 1.65 | 48.50 ± 7.46 |
|
51.82 ± 1.51 | 46.86 ± 1.18 |
| P value | 0.21 | <0.001 |
| QTc dispersion (ms) | ||
|
4.50 ± 1.91 | 4.50 ± 1.91 |
|
3.81 ± 1.07 | 3.81 ± 1.07 |
|
3.71 ± 1.03 | 2.36 ± 1.02 |
|
3.49 ± 1.36 | 1.88 ± 0.59 |
| P value | 0.34 | <0.001 |
Table 4: QT interval among enrolled patients based on TIMI flow.
Additionally, patients with LAD as culprit lesion had significantly (p=0.042) higher maximum QTc (48.8 ± 2.2) and QTc dispersion (2.3 ± 0.9) after PCI in comparison to those with non-LAD culprit lesion (46.4 ± 5.9) and (2.1 ± 1.1) shown in the Table 5.
| LAD (n=125) | Non-LAD (n=75) | P value* | |
|---|---|---|---|
| Minimum QTc (ms) | |||
|
48.48 ± 1.63 | 48.11 ± 1.46 | 0.091 |
|
45.71 ± 1.85 | 45.81 ± 1.94 | 0.713 |
| Maximum QTc (ms) | |||
|
52.11 ± 1.48 | 51.65 ± 1.55 | 0.172 |
|
48.84 ± 2.20 | 46.38 ± 5.92 | 0.042 |
| QTc dispersion (ms) | |||
|
3.60 ± 1.37 | 3.54 ± 1.252 | 0.354 |
|
2.33 ± 0.88 | 2.08 ± 1.07 | <0.001 |
Note: *Independant t-test was used to compare the difference in means
Table 5: QT interval among studied patients based on culprit lesions.
The correlation between QTc changes after PPCI and the angiographic parameters revealed that patients with better TIMI flow grade and MBG and less c-TFC after PPCI had more change in the minimum QTc, the maximum QTc and the QT-d after PPCI shown in Table 6.
| Variable ( regarding QTc dispersion) | β (95% CI) | T-Statistics | P-value |
|---|---|---|---|
| Constant | 2.052 (1.399-2.705) | 6.19 | <0.001 |
| Age in years | 0.005 (-0.010-0.013) | 0.32 | 0.751 |
| Sex (Male) | -0.443 (-0.748-0.139) | -2.87 | 0.005 |
| Smoker | 0.267 (-0.987-0.536) | 2.04 | 0.049 |
| Pain Onset/hour | 0.018 (-0.003-0.040) | 1.69 | 0.093 |
| TIMI Flow | -0.794 (-0.954-0.633) | -9.76 | <0.001 |
| MBG | -0.563 (-0.693-0.435) | -8.45 | <0.001 |
| Pre-dilatation | 0.240 (-0.037-0.518) | 1.71 | 0.088 |
| Use of GPIIB/IIIA | 0.289 (0.007-0.570) | 2.52 | 0.041 |
| EF% | -0.015 (-0.030: -0.001) | -2.15 | 0.032 |
| Constant | 1.916 (1.057-2.775) | 4.4 | <0.001 |
| Age in years | -0.009 (-0.024-0.006) | -1.14 | 0.256 |
| Sex (Male) | 0.110 (-0.300-0.520) | 0.53 | 0.597 |
| TIMI Flow | 0.557 (0.312-0.803) | 4.48 | <0.001 |
| MBG | 0.410 (0.218-0.602) | 4.21 | <0.001 |
| Door to Balloon/min. | 0.038 (-0.026-0.103) | 1.18 | 0.241 |
| TIMI Frame Count | -0.032 (-0.047-0.017) | -4.19 | <0.001 |
Table 6: Independent predictors of QTc dispersion and change in QTc dispersion after PPCI by Multivariate linear regression analysis.
Change in maximum QTc had high moderate positive correlation with TIMI flow grade and MBG and significant moderate negative correlation with c TFC (r-value=0.634, p-value=<0.001, r-value=0.604, p-value=<0.001 , r-value=- 0.493, p-value=<0.001 respectively).
As regard MACE, following up data after 12 months of discharge for the incidence of MACE revealed that: About one fifth (n=52) of patients developed MACE where 17% (n=34), 8.5% (n=17), and 4% (n=8) patients had recurrent admission due to other cardiac cause was heart failure, non-fatal MI and stroke, respectively. The one-year mortality incidence was 9% (n=18) (Table 7). It was found that patients who developed MACE and those didn’t developed MACE had insignificant (p>0.05)
| Min. QTc Change | Max. QTc Change | QTc Dispersion Change | |
|---|---|---|---|
| r* (P-value**) | |||
| TIMI Flow | 0.556 (<0.001) | 0.634 (<0.001) | 0.304 (<0.001) |
| MBG | 0.526 (<0.001) | 0.604 (<0.001) | 0.287 (<0.001) |
| TIMI-frame | -0.423 (<0.001) | -0.493 (<0.001) | -0.285 (<0.001) |
Note: *Pearson correlation coefficient **Based on normal approximation
Table 6: Independent predictors of QTc dispersion and change in QTc dispersion after PPCI by Multivariate linear regression analysis.
| Min. QTc Change | Max. QTc Change | QTc Dispersion Change | |
|---|---|---|---|
| r* (P-value**) | |||
| TIMI Flow | 0.556 (<0.001) | 0.634 (<0.001) | 0.304 (<0.001) |
| MBG | 0.526 (<0.001) | 0.604 (<0.001) | 0.287 (<0.001) |
| TIMI-frame | -0.423 (<0.001) | -0.493 (<0.001) | -0.285 (<0.001) |
Note: *Pearson correlation coefficient **Based on normal approximation
Table 7: Correlation between change in QTc Parameters from before to after PPCI and the angiographic parameters.
Differences as regard baseline minimum QTc, maximum QTc and QTc dispersion but all these findings were significantly (p<0.001) higher after PPCI among patients who developed MACE shown in the Table 8.
| MACE | No-MACE | P value* | |
|---|---|---|---|
| (n= 45) | (n= 155) | ||
| Minimum QTc (ms) | |||
| Before PCI | 48.57 ± 1.63 | 48.27 ± 1.56 | 0.26 |
| After PCI | 48.06 ± 2.00 | 45.07 ± 1.18 | <0.001 |
| Min.QTc change | 0.5 ± 1.6 | 3.2 ± 1.6 | <0.001 |
| Maximum QTc (ms) | |||
| Before PCI | 52.31 ± 1.53 | 51.83 ± 1.51 | 0.06 |
| After PCI | 49.95 ± 7.76 | 47.01 ± 1.28 | <0.001 |
| Max. QTc change | 1.4 ± 2.1 | 4.8 ± 1.7 | <0.001 |
| QTc dispersion (ms) | |||
| Before PCI | 3.73 ± 1.32 | 3.54 ± 1.33 | 0.396 |
| After PCI | 2.91 ± 1.39 | 1.93 ± 0.6 | <0.001 |
| QTc dispersion change | 0.8 ± 1.09 | 1.6 ± 1.2 | <0.001 |
*Independant t-test was used to compare the difference in means
Table 8: QT interval among studied patients based on occurrence of one year MACE.
There is significant mild negative correlation between change in QTdispersion and occurrence of MACE (r-value=-0.2), high moderate negative correlation between change in minimum and maximum QT and occurrence of MACE (r-value=0.5, 0.6 respectively) and moderate positive correlation between QT dispersion after PPCI and occurrence of MACE (r-value=0.465). Also it was noticed that there is significant high negative correlation between TIMI flow grade and myocardial blush grade and occurrence of MACE (r-value=-0.6, -0.6 respectively). And significant high moderate positive correlation between TFC and occurrence of MACE (r-value=0.5) shown in the Table 9.
| MACE | ||
|---|---|---|
| Variable | R value | P value |
| Min QTc before PPCI | 0.08 | 0.2 |
| Max. QTc before PPCI | 0.1 | 0.06 |
| QTd before PPCI | 0.06 | 0.3 |
| Min. QTc after PPCI | 0.6 | <0.001 |
| Max. QTc after PPCI | 3 | <0.001 |
| QTd after PPCI | 0.4 | <0.001 |
| Min. QT change | -0.5 | <0.001 |
| Max. QT change | -0.6 | <0.001 |
| QTd change | -0.2 | <0.001 |
| TIMI flow grade | -0.6 | <0.001 |
| MBG | -0.6 | <0.001 |
| cTFC | 0.5 | <0.001 |
Table 9: Correlation between electrocardiographic and angiographic parameters with occurrence of one year MACE.
As illustrated in Table 10, it was noticed that patients who died had significantly higher minimum QTc, maximum QTc and QTc dispersion after PCI in comparison to survivors.Also we found that patients who died had significantly lower minimum QTc change, maximum QTc change and QTc dispersion change after PCI in comparison to survivors. Also we found that patients who died had significantly lower TIMI flow grade, MBG but significantly higher TFC after PCI in comparison to survivors.
| ECG and angiographic parameters | Death group (N=18) | Survivor group (N=182) | P-Value |
|---|---|---|---|
| Minimum QTc(ms) | |||
| Before PCI | 48.66 ± 1.53 | 48.31 ± 1.58 | 0.367 |
| After PCI | 48.22 ± 1.92 | 45.5 ± 1.69 | <0.001 |
| Maximum QTc (ms) | |||
| Before PCI | 52.22 ± 1.35 | 51.91 ± 1.54 | 0.412 |
| After PCI | 51.00 ± 2.61 | 47.34 ± 3.98 | <0.001 |
| QTc dispersion(ms) | |||
| Before PCI | 3.55 ± 1.46 | 3.58 ± 1.31 | 0.922 |
| After PCI | 2.77 ± 1.35 | 2.09 ± 0.89 | 0.004 |
| Min. QT change | 0.44 ± 1.61 | 2.80 ± 1.91 | <0.001 |
| Max. QT change | 1.22 ± 2.04 | 4.33 ± 2.15 | <0.001 |
| QTd change | 0.77 ± 1.06 | 1.51 ± 1.26 | 0.02 |
| TIMI flow grade | 2.00 ± 0.722 | 2.67 ± 0.653 | <0.001 |
| MBG | 1.6 ± 0.796 | 2.53 ± 0.838 | <0.001 |
| TFC | 32.94 ± 11.67 | 19.02 ± 10.4 | <0.001 |
Table 10: ECG and angiographic parameters and mortality.
Discussion
It was found that subgroups of minimum and maximum QT either before or after PCI had insignificant differences as regards the age of patients. Also, male patients had significantly lower corrected QT dispersion after PCI in comparison to female patients, this may be explained by the impairment of coronary flow owing to functional (i.e., impaired dilation or increased constriction of coronary microvessels) and/or structural abnormalities of the microcirculation can be sustained by several mechanisms Recently, it has been proposed that Coronary microvascular dysfunction in women plays a central role in the genesis of symptoms and myocardial ischemia, specifically in the case of MINOCA [17].
There was a significant decrease after revascularization in minimum QTc, maximum QTc, and corrected QT dispersion in the study population. Moreover, there was a significant correlation of improved QTc, QT-d, and change in QTc and QT-d with the degree of revascularization including TIMI flow, MBG, and c-TFC. This indicated that the better the revascularization by PPCI the more the myocardial electrical stability this being explained by Cardio-myocytes necrosis and slippage, disturbed inter-cellular connections, altered ventricular geometry and dilatation, and reactive hypertrophy, are all part of the ventricular remodeling process after acute myocardial infarction. All these factors are liable to influence the heterogeneity of ventricular repolarization affecting QT and QT-d but early successful revascularization and restoration of blood flow including macro and microcirculation has a great role in myocardial salvage and so restoring myocardial electrical stability. The current study was in agreement with Eslami, et al. [18], who found a significant reduction in QT-d after PCI. Therefore, a significant decrease in QT-d may be used as an electrocardiographic marker of successful reperfusion. As well, Bei, et al. [19], studied the effect of the percutaneous coronary intervention on QT-d and its clinical implication in patients with AMI and found that QT-d and QT-cd were remarkably decreased after PCI. On the other hand, there was a point of difference from this study as Eslami, et al. [18], stated that no significant difference in QTc could be explained by the smaller number of patients enrolled in their study. Also, another possible explanation of this difference was the timing of ECG obtained after the reperfusion because it is known that QT is prolonged during ischemia but the timing of normalization of QT after reperfusion is not immediate and usually occurs within days post-reperfusion. In Eslami et al. [18], ECGs were obtained 24 hours after PPCI but in this study, ECGs were conducted 48 hours after PPCI hence this may explain the difference and suggested that it is better to use QT-d in later ECGs as a marker of successful reperfusion..
Furthermore, it was concluded that patients with TIMI flow grade 3 had significantly lower minimum QTc, maximum QTc, and QTc dispersion after PCI in comparison to grade 2, grade 1, and grade 0. This was in agreement with Nikiforos, et al. [20], who compared the effects of reperfusion by primary Percutaneous Trans luminal Coronary Angioplasty (PTCA) and by thrombolysis on QT-d and correlation of these results with the degree of reperfusion and found a significant decrease in QT dispersion may provide an additional electrocardiographic index for successful (TIMI 2/3) reperfusion. Added to this we had a larger number of patients enrolled in our study showed a significant difference of QT-d in patients with TIMI 3 flow from those with TIMI 2 flow indicating that QT-d is a sensitive indicator of the degree of myocardial reperfusion and its effect on myocardial electrical stability. This was also in line with Karagounis, et al. [21], who found that there were significant differences in QT-d and QT- cd between TIMI grades 0, 1 versus 2/3, and between TIMI grades 0/1/2 and 3. These findings suggested that successful and sustained restoration of blood flow leads to reduced dispersion of repolarization. Moreover, patients with myocardial blush grades 3 or 2 had significantly lower minimum and maximum QTc after PCI in comparison to those with grade 1 or 0.
It was also found that cQT-d was significantly lower among patients with myocardial blush grade 3 after PCI in comparison to those with grade 2, grade 1 and grade 0. This was in agreement with Fukushima, et al. [22], who found that QT-d decreased in patients with MBG3 but not in patients with MBG0-1 or MBG2 and this adds to the point that cQTd is more sensitive than the minimum and maximum cQT as a marker of the degree of myocardial reperfusion and electrical stability. It was also noticed that the TIMI frame count resulted in a moderate positive significant correlation with QTc dispersion after PCI in agreement with Atak, et al. [23], who found a significant correlation between QT-d and TIMI frame counts.
This study reported that patients with LAD as culprit lesion had significantly higher maximum QTc and QTc dispersion after PCI compared to those with non-LAD culprit lesions, one possible reason for this is the larger area of myocardium involved in cases with LAD as culprit artery versus those with the non-LAD culprit. This was also in agreement with Kilic, et al., [24], who found that during PTCA the greatest QT-d was observable in the LAD lesions.
On the other hand, this disagreed with Hassan, et al. [25], who found that there were a lower value of QT maximum and QT minimum after reperfusion in those presented with anterior MI when compared with those presented with inferior MI). This difference could be explained in Hassan, et al. [25], who found that there was a significant reduction in HR after reperfusion in patients presented with inferior MI when compared with those presented with anterior MI (p=0.030) while in this study there was no significant difference in heart rate. Also, the current results were contradicted with Alasti, et al. [26], who found that the QTc dispersion values were higher in the RCA group (a small group with only 14 patients) mostly due to the smaller number of patients enrolled in their study.
It was noticed that patients who developed MACE and those who didn’t develop MACE had insignificant differences as regard baseline minimum QTc, maximum QTc, and QTc dispersion before PPCI but all these findings were significantly higher after PCI among patients who developed MACE. In agreement with Pan, et al. [27], who found that cQTd at 24 hours after primary PCI was significantly shorter in patients without MACE than in patients with MACE. But the current study was different from another study that found that cQTd before primary PCI was significantly longer in patients without MACE than in patients with MACE. One possible reason for this difference was the relatively small number of patients with MACE enrolled in their study [27]. Also, this was concordant with Civan, et al. [28], who found that the mean QT-d of the non-MACE group was significantly lower than that of the MACE group. As the most serious parameter of MACE was death. The current study found that patients who died had significantly higher minimum QTc, maximum QTc, and QTc dispersion after PCI in comparison to survivors. Also, they had significantly lower minimum QTc change, maximum QTc change, and QTc dispersion change after PCI in comparison to survivors. Likewise, they had significantly lower TIMI flow grade, MBG but significantly higher TFC after PCI in comparison to survivors. So better ECG parameters and angiographic parameters suggest less incidence of CV one-year mortality after MI.
Overall, it was noticed that the value of QT dispersion after PPCI and the value of change in maximum and minimum QT had showed a stronger correlation with angiographic parameters and occurrence of MACE compared to the value of the change in QT dispersion, this is explained by the narrow range of the change occurred in QT dispersion our cases.
Conclusion and Recommendations
Shortening of the corrected QT and QT dispersion is associated with successful myocardial revascularization. Also, changes in maximum QT were better in predicting optimum revascularization as assessed by TIMI flow grade and MBG than the changes in QT dispersion. These changes can also help in predicting lower MACE after a one-year follow-up in STEMI patients treated by PPCI. It was also concluded that the QT-d after PPCI and the change in maximum and minimum QT had a stronger correlation with angiographic parameters and occurrence of MACE compared to the value of the change in QT-d.
Limitations
The current study was exposed to several limitations: Lack of some important laboratory data as lipid profile for every patient.
Ethical Approval and Consent to Participate
This study was approved by committee of medical ethics of faculty of medicine; Assiut University in 2017 , informed consent was obtained from all participants.
Availability of Data and Materials
All data generated and / or analyzed during this study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
No funding received for this study.
Authors' Contributions
MSRT has contributed to concept, design, literature search, clinical studies, statistical analysis, manuscript preparation, editing and review. HHA contributed to design, literature search, manuscript preparation and review. HHA contributed to literature search, clinical studies, manuscript editing and final draft.All authors have read , revised and approved the final manuscript.
References
- Steg P, James S, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 33(20): 2569-2619 (2012).
[Cross ref] [Google scholar] [PubMed]
- Roe M, Ohman E, Maas A, et al. Shifting the open-artery hypothesis downstream: the quest for optimal reperfusion. J Am Coll Cardiol. 37(1): 9-18 (2001).
[Cross ref] [Google scholar] [PubMed]
- Gibson C, Dotani M, Murphy S, et al. Correlates of coronary blood flow before and after percutaneous coronary intervention and their relationship to angiographic and clinical outcomes in the RESTORE trial. Am Heart J. 144(1): 130-135 (2002).
[Cross ref] [Google scholar] [PubMed]
- Marra M, Corbetti F, Cacciavillani L, et al. Relationship between myocardial blush grades, staining, and severe microvascular damage after primary percutaneous coronary intervention: a study performed with contrast-enhanced magnetic resonance in a large consecutive series of patients. Am Heart J. 159(6): 1124-1132 (2010).
[Cross ref] [Google scholar] [PubMed]
- Henriques J, Zijlstra F, Van ‘T Hof A, et al. Angiographic assessment of reperfusion in acute myocardial infarction by myocardial blush grade. Circulation. 107(16): 2115-2119 (2003).
[Cross ref] [Google scholar] [PubMed]
- Foroughi M, Yousefi Z, Tehrani M, et al. Prolonged QT interval and coronary artery bypass mortality due to heart failure. Asian Cardiovasc Thorac Ann. 17(6): 604-607 (2009).
[Cross ref] [Google scholar] [PubMed]
- Eltahlawi MA, Sanad AM, Ghazal KH, et al. Can QT dispersion improve the accuracy of stress ECG TMT in detecting myocardial ischemia in chronic stable CAD patients? A stress myocardial perfusion imaging study. Egypt Heart J. 73(1) 5. (2021).
[Cross ref] [Google scholar] [PubMed]
- Ibánez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Rev Esp Cardiol (Engl Ed). 70(12): 1082-1088 (2017).
[Cross ref] [Google scholar] [PubMed]
- WHO. World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate and hyperglycemia. Report of a WHO/IDF consultation. (2006).
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). J Hypertens. 39(33): 3021-3104 (2018).
[Cross ref] [Google scholar] [PubMed]
- WHO. Physical Status: The Use and Interpretation of Anthropometry: Report of a World Health Organization (WHO) Expert Committee. Geneva, Switzerland: World Health Organization. (1995).
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis. 39(5): S1-S2 (2002).
- Goldenberg I, Moss A, Zareba W. Basic principles and patterns. In: Clinical electrocardiography: A simplified approach. J Cardiovasc Electrophysiol. 17(3): 333-336 (2012).
- Malik M, Batchvarov V. Measurement, interpretation, and clinical potential of QT dispersion. J Am Coll Cardiol. 36(6): 1749-1766 (2000).
[Cross ref] [Google scholar] [PubMed]
- Ahnve S. Correction of the QT interval for heart rate: review of different formulas and the use of Bazett's formula in myocardial infarction. Am Heart J. 109(3): 568-574 (1985).
[Cross ref] [Google scholar] [PubMed]
- Killip T, Kimball J. Treatment of myocardial infarction in a coronary care unit: a two-year experience with 250 patients. Am J Cardiol. 20(4): 457-464 (1967).
[Cross ref] [Google scholar] [PubMed]
- Kothawade K, Merz CNB. Microvascular coronary dysfunction in women: pathophysiology, diagnosis, and management. Curr Probl Cardiol. 36(8): 291-318 (2011).
[Cross ref] [Google scholar] [PubMed]
- Eslami V, Rouhani-Esfahani S, Hafezi-Nejad N, et al. Evaluation of QT, QT Dispersion, and T-Wave Peak to End Time Changes After Primary Percutaneous Coronary Intervention in Patients Presenting with Acute ST-Elevation Myocardial Infarction. J Invasive Cardiol. 25(5): 232-234 (2013).
[Google scholar] [PubMed]
- Bei CH, Luo Y, Li GL, et al. Effect of percutaneous coronary intervention on QT dispersion and its clinical implication in patients with acute myocardial infarction. Aca j first med col PLA. 24(9):1055-1057 (2004).
[Google scholar] [PubMed]
- Nikiforos S, Hatzisavvas J, Pavlides G, et al. QT‐interval dispersion in acute myocardial infarction is only shortened by thrombolysis in myocardial infarction grade 2/3 reperfusion. Clin Cardiol. 26(6): 291-295 (2003).
- Karagounis LA, Anderson JL, Moreno FL, et al. Multivariate associates of QT dispersion in patients with acute myocardial infarction: primacy of patency status of the infarct-related artery. Am Heart J. 135(6): 1027-1035 (1998).
[Cross ref] [Google scholar] [PubMed]
- Fukushima N, Tsurumi Y, Jujo K, et al. Impact of myocardial reperfusion status on qt dispersion after successful recanalization of the infarct‐related artery in acute myocardial infarction. J Interv Cardiol. 27(3): 252-259 (2014).
[Cross ref] [Google scholar] [PubMed]
- Atak R, Turhan H, Sezgin A, et al. Effects of slow coronary artery flow on QT interval duration and dispersion. Ann Noninvasive Electrocardiol. 8(2): 107-111 (2003).
[Cross ref] [Google scholar] [PubMed]
- Kilic H, Atalar E, Necla O, et al. QT interval dispersion changes according to the vessel involved during percutaneous coronary angioplasty. J Natl Med Assoc. 99(8): 914-923 (2007).
[Google scholar] [PubMed]
- Hassan T, Abou Omar M, Alarag A. QT dispersion changes following primary percutaneous coronary intervention in acute myocardial infarction comparison between primary pci plus thrombectomy and primary pci without thrombectomy. J Clin Exp Cardiolog. 9(595): 2-8 (2018).
- Alasti M, Adel MH, Torfi E, et al. QT dispersion: does it change after percutaneous coronary intervention? J Tehran Heart Cent. 6(1): 19-23 (2011).
- Pan KL, Hsu JT, Chang ST, et al. Prognostic value of QT dispersion change following primary percutaneous coronary intervention in acute ST elevation myocardial infarction. Int Heart J. 52(4): 207-211 (2011).
[Cross ref] [Google scholar] [PubMed]
- Civan M, Özcan S, Ziyrek M, et al. Relationship between cardiovascular evaluation data on admission and secondary adverse cardiac event rate after acute coronary syndrome. J Exp Clin Med. 31(2): 15-22 (2014).