Mini Review - Interventional Cardiology (2021) Volume 13, Issue 2
Indication of non-surgical management for acute limb ischemia
- Corresponding Author:
- Ryo Araki
Department of Cardiovascular Medicine, Otemae Hospital, Osaka 540- 0008, Japan,
E-mail: araki24r@otemae.gr.jp
Received date: March 02, 2021 Accepted date: March 16, 2021 Published date: March 23, 2021
Abstract
Acute Limb Ischemia (ALI) is a sudden decrease in limb perfusion that has a potential threat of life and limb viability. Although, surgical thrombectomy using an occlusion catheter (Fogarty catheter) has been traditionally performed as the standard approach for ALI, endovascular treatment (EVT) has recently been developed as an alternative to surgical revascularization. However, its indication remains unclear. We reviewed the indication of conventional treatments and introduced our original technique. There are several non-surgical treatments for ALI such as Percutaneous Aspiration Thrombectomy (PAT), Catheter-Directed Thrombolysis (CDT), angioplasty and stenting. PAT is effective for the patients with ALI in small vessels such as below-the-knee arteries. CDT is recommended for Rutherford grade I patients. Angioplasty and stent implantation, which is a well-established strategy in peripheral arterial disease, is applicable for the ALI patients in any Rutherford grade. We previously reported an endovascular technique using a guide extension catheter in the non-stenting zone for ALI, which is named “Temporary Endoluminal Bypass (TEB) technique”. This technique is based on the concept of a perfusion catheter and applied for a treatment of ALI. This technique is composed of 3 steps. First, we measure the lesion length. Second, we deliver the guide extension catheter to fully cover the lesion. Finally, we confirm the distal blood flow by angiography. Subsequently, urokinase (10,000 U/hr) is selectively administered to the vessel from the sheath. The endpoint of thrombolysis is determined by the achievement of antegrade blood flow after removal of the guide extension catheter. TEB technique is basically recommended for the ALI patients with Rutherford grades IIa and IIb. TEB technique may be an alternative treatment option for ALI although further investigation is needed.
Keywords
Acute limb ischemia • Endovascular treatment•Non-surgical management •Guide extension catheter
Introduction
Acute Limb Ischemia (ALI) is a sudden decrease in limb perfusion that has a potential threat of life and limb viability. The risk of limb loss is ranging between 5% and 30% and the mortality rate as high as 18% [1,2]. Although, surgical thrombectomy using an occlusion catheter (Fogarty catheter) has been traditionally performed as the standard approach for ALI, endovascular treatment (EVT) has recently been developed as an alternative to surgical revascularization because it is less invasive and has shown the acceptable Amputation Free Survival (AFS) rate [3-7]. There are several conventional EVT procedures for ALI such as Percutaneous Aspiration Thrombectomy (PAT), angioplasty, stenting and Catheter-Directed Thrombolysis (CDT). However, their indication remains unclear. Here, we summarize the endovascular management and their indication for ALI.
Etiology of Acute Limb Ischemia
The etiology of ALI can be classified into five main categories: embolism (30%), native vessel thrombosis (40%), stent or graft-related thrombosis (20%), peripheral aneurysm-related thrombosis (5%), and trauma (5%) [1,8]. The two major etiologies are native vessel thrombosis and embolism, representing 70% of all ALI [8]. Native vessel thrombosis usually occurs in the severe and complicated atherosclerotic plaques [9]. Those patients often have a history of claudication or atherosclerosis in the contralateral limb artery. Embolism is derived from intracardiac thrombus due to atrial arrhythmia (flutter/fibrillation) or congestive heart failure, or intracardiac mass such as myxoma or vegetation [1]. Rarely, paradoxical embolization occurs in patients with venous thromboembolism and right to left shunt diseases. Recently, embolism of thrombus or atherosclerotic debris from aortic ruptured plaque has been regarded as an important cause of limb ischemia [10,11]. Those patients do not usually have contralateral limb artery atherosclerosis. Stent or graft related thrombosis occurs in the patients with a prior history of treatment for Peripheral Arterial Disease (PAD), which can be easily visualized by imaging modalities [1]. Trauma and peripheral artery aneurysm are uncommon causes of ALI. Popliteal artery aneurysms are the most frequent and accounting for approximately 70% of peripheral artery aneurysms [12].
Conventional Treatments
PAT, which is a simple suction of embolized material by 6-8F catheter connected to a syringe, is recommended for the patients with ALI in small vessels such as below-the-knee arteries [13]. Since a catheter can aspirate the material smaller than its size, the recanalization by PAT alone is not frequently successful in ALI [8]. The recanalization by PAT alone was reported successful only in approximately 30%. However, PAT has been reported very useful for an acute iatrogenic distal embolization during endovascular treatment in the below-the-knee arteries [8].
CDT is considered as first-line strategy for ALI with a similar clinical outcome compared to surgical treatment, based on three major trials (Rochester [14], TOPAS [5], and STILE [6] trials). These trials randomized patients with ALI to CDT or surgical treatment. In Rochester trial, AFS rate at 12 months were equivalent (82% vs. 82%). There was also no significant difference in AFS rate at 6 months between CDT and surgical groups in TOPAS trial (71.8% vs. 74.8%; P=0.23) and in STILE trial (88.2% vs. 89.4%; P=0.87). The procedures of CDT are as follows; the catheter with multiple holes is inserted into thrombus and thrombolytic drug is infused through the catheter. Although the severity of ALI is classified by Rutherford category [15], CDT can be used only in Rutherford grade I patients [5,6]. In other Rutherford grades patients, immediate revascularization is required for limb salvage.
Angioplasty and stent implantation is a well-established strategy in chronic arterial disease. Kim et al. reported that stent-assisted recanalization was successful in all patients and eliminated the clinical symptoms in 12 (80%) patients among 15 ALI patients, suggesting its high technical success rate with good clinical outcome as a bailout procedure for ALI [16]. These procedures are often required for the pre-existing atherosclerotic lesions, which cannot be sufficiently removed by thrombectomy or thrombolysis [8]. Although stent implantation is widely applicable for the ALI patients in any Rutherford grade, we usually avoid it in the nonstenting zone such as common femoral artery and popliteal artery. Since non-stenting zone is located in the area of major joint, the stent implanted in the zone is easily fractured by the joint movement.
Anticoagulant therapy
Intravenous administration of unfractionated heparin is widely accepted as an initial medical treatment for ALI [17]. It is initially administrated at the dose of 5000 IU or 70-100 IU/ kg and monitored by activated clotting time or activated partial thromboplastin time and continued in the early postoperative period. The aim of heparin administration is to reduce further embolism or secondary clot propagation [18]. Low molecular weight heparin, already used in Europe in the last 10 years, is widely administrated in case of acute venous thromboembolism and acute coronary syndrome [19]. However, it is not still commonly used for ALI.
Another option of endovascular treatment
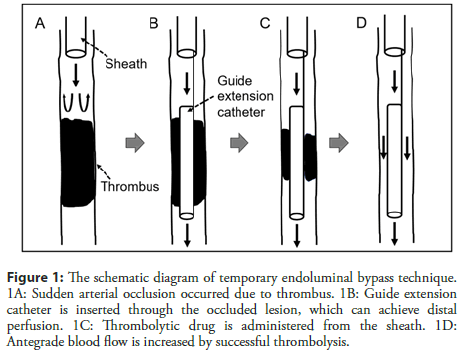
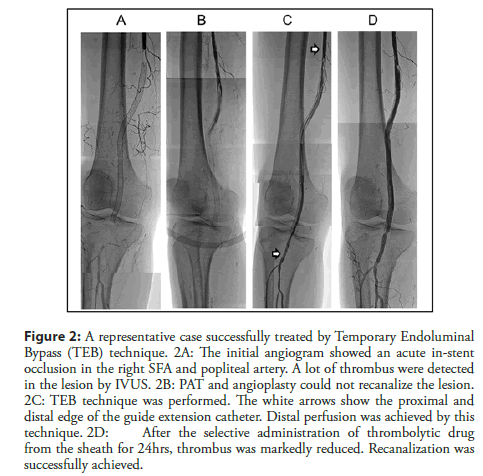
We previously reported an endovascular technique using a guide extension catheter [20]. This technique, named “Temporary Endoluminal Bypass (TEB) technique”, maintains distal perfusion while thrombolysis is performed. The schematic diagram of this technique is presented in Figure 1. This technique is composed of 3 steps. First, we measure the lesion length. Second, we deliver the guide extension catheter to fully cover the lesion. Finally, we confirm the distal blood flow by angiography. Subsequently, urokinase (10,000 U/hr) is selectively administered to the vessel from the sheath. The endpoint of drug administration is determined by the achievement of antegrade blood flow after removal of the guide extension catheter. We evaluate it every 24 hrs by repeated angiography. We also show the representative case, successfully treated by TEB technique in Figure 2. Clinically, this technique is recommended for the ALI patients with Rutherford grades IIa and IIb, which are defined as salvageable with immediate recanalization. Although this technique is applicable for the ALI patient with Rutherford grade I, which is defined as viable limb without immediate threat of amputation. However, CDT has the higher recommendation than TEB technique as the first-line treatment according to the current guideline [21]. TEB technique can be used in the non-stenting zone and can be applied for the ALI patient of any etiology. Balloon angioplasty may be required to dilate the atherosclerotic stenosis before inserting the guide extension catheter. The lesion length of less than 40 cm can be covered by guide extension catheter. Depending on the lesion length, we can use GUIDEZILLA II PV (Boston Scientific, Tokyo, Japan) that can cover 40 cm lesion or GuideLiner PV (Japan Lifeline, Tokyo, Japan) that can cover 25 cm lesion.
Figure 1: The schematic diagram of temporary endoluminal bypass technique. 1A: Sudden arterial occlusion occurred due to thrombus. 1B: Guide extension catheter is inserted through the occluded lesion, which can achieve distal perfusion. 1C: Thrombolytic drug is administered from the sheath. 1D: Antegrade blood flow is increased by successful thrombolysis.
Figure 2: A representative case successfully treated by Temporary Endoluminal Bypass (TEB) technique. 2A: The initial angiogram showed an acute in-stent occlusion in the right SFA and popliteal artery. A lot of thrombus were detected in the lesion by IVUS. 2B: PAT and angioplasty could not recanalize the lesion. 2C: TEB technique was performed. The white arrows show the proximal and distal edge of the guide extension catheter. Distal perfusion was achieved by this technique. 2D: After the selective administration of thrombolytic drug from the sheath for 24hrs, thrombus was markedly reduced. Recanalization was successfully achieved.
There are some disadvantages in this technique. During delivery of the catheter beyond the occluded lesion, vessel dissection or pushing thrombus into the distal patent vessel can be occurred. Besides, the patients need bed rest until the removal of all the devices, and they are exposed to the risks of bleeding and infection.
According to the PAD guideline [21], PAT, CDT, angioplasty, stenting, or thrombectomy are recommended to revascularize the occluded artery in ALI. However, this TEB technique might be an alternative in cases of failed conventional treatments for ALI and further investigation with TEB technique needs to be undertaken. Recommended non-surgical managements for ALI are summarized in Table 1.
| Lesion | ALI grade | Reference | |
|---|---|---|---|
| PAT | Below-the-knee artery | - | [8,13] |
| CDT | - | Ⅰ | [5,6] |
| Angioplasty | - | - | |
| Stenting | Iliac artery SFA | - | [16] |
| TEB technique | CFA Popliteal artery | Ⅱa, Ⅱb | [20] |
ALI: Acute Limb Ischemia; PAT: Percutaneous Aspiration Thrombectomy; CDT: Catheter-Direct Thrombolysis; SFA: Superficial Femoral Artery; TEB: Temporary Endoluminal Bypass; CFA: Common Femoral Artery
Table 1: Recommended non-surgical managements according to the occluded lesion and ALI grade.
Conclusion
We summarized the indications of non-surgical treatments of ALI. Their indications are determined by Rutherford category of ALI and by the area of culprit lesion. We should select the appropriate strategy knowing the advantage and disadvantage of those treatments.
Statement of Consent
The authors confirm that written consent for submission and publication of this review including images and associated text has been obtained from the patient in line with COPE guidance.
Funding
None
Disclosures
Ueda Y: Research grants from Abbott Vascular, Pfizer, Bayer, Daiichi-Sankyo, Astellas, Shionogi, Sanofi, Ono, Nihon Kohden, Amgen Astellas, Actelion, Bristol-Myers Squibb, Medtronic, AstraZeneca, Otsuka, and Novartis. Lecture fees from Daiichi- Sankyo, MSD, Goodman, Sanofi, Mochida, Takeda, Kowa, Teijin, Astellas, Actelion, Bristol-Myers Squibb, AstraZeneca, Boston Scientific, Sumitomo Dainippon Pharma, Eisai, and Amgen Astellas; Abe H: Research grants from Daiichi Sankyo and Boehringer Ingelheim; Others: None.
References
- Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg. 45(S1): S5-S67 (2007).
- Eliason JL, Wainess RM, Proctor MC, et al. A national and single institutional experience in the contemporary treatment of acute lower extremity ischemia. Ann Surg. 238(3): 382-9 (2003).
- Wang JC, Kim AH, Kashyap VS. Open surgical or endovascular revascularization for acute limb ischemia. J Vasc Surg. 63(1): 270-8 (2016).
- Ouriel K, Shortell CK, DeWeese JA, et al. A comparison of thrombolytic therapy with operative revascularization in the initial treatment of acute peripheral arterial ischemia. J Vasc Surg. 19(6): 1021-30 (1994).
- Ouriel K, Veith FJ, Sasahara AA. A comparison of recombinant urokinase with vascular surgery as initial treatment for acute arterial occlusion of the legs. Thrombolysis or Peripheral Arterial Surgery (TOPAS) Investigators. N Engl J Med. 338(16): 1105-11 (1998).
- Weaver FA, Comerota AJ, Youngblood M, et al. Surgical revascularization vs. thrombolysis for nonembolic lower extremity native artery occlusions: Results of a prospective randomized trial. The STILE Investigators. Surgery vs. Thrombolysis for ischemia of the lower extremity. J Vasc Surg. 24(4): 513-21 (1996).
- Earnshaw JJ, Whitman B, Foy C. National audit of thrombolysis for acute leg ischemia (NATALI): Clinical factors associated with early outcome. J Vasc Surg. 39(5): 1018-25 (2004).
- Olinic DM, Stanek A, Tătaru DA, et al. Acute Limb Ischemia: An update on diagnosis and management. J Clin Med. 8(8): 1215 (2019).
- Eldrup-Jorgensen J, Flanigan DP, Brace L, et al. Hypercoagulable states and lower limb ischemia in young adults. J Vasc Surg. 9: 334–41 (1989).
- Narula N, Dannenberg AJ, Olin JW, et al. Pathology of peripheral artery disease in patients with critical limb ischemia. J Am Coll Cardiol. 72(18): 2152-63 (2018).
- Komatsu S, Yutani C, Ohara T, et al. Angioscopic evaluation of spontaneously ruptured aortic plaques. J Am Coll Cardiol. 71(25): 2893-2902 (2018).
- Lawrence PF, Lorenzo-Rivero S, Lyon JL. The incidence of iliac, femoral, and popliteal artery aneurysms in hospitalized patients. J Vasc Surg. 22(4): 409-15 (1995).
- Desgranges P, Kobeiter K, d'Audiffret A, et al. Acute occlusion of popliteal and/or tibial arteries: the value of percutaneous treatment. Eur J Vasc Endovasc Surg. 20(2): 138-45 (2000).
- Ouriel K, Shortell CK, DeWeese JA, et al. A comparison of thrombolytic therapy with operative revascularization in the initial treatment of acute peripheral arterial ischemia. J Vasc Surg. 19: 1021-30 (1994).
- Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: Revised version. J Vasc Surg. 26(3): 517-38 (1997).
- Kim C, Jeon W, Shin T, et al. Stent-assisted recanalisation of acute occlusive arteries in patients with acute limb ischemia. Eur J Vasc Endovasc Surg. 39(1): 89-96 (2010).
- Björck M, Earnshaw JJ, Acosta S, et al. Editor's choice-European society for vascular surgery (ESVS) 2020 clinical practice guidelines on the management of acute limb ischaemia. Eur J Vasc Endovasc Surg. 59(2): 173-218 (2020).
- Norgren L, Swedish EnoxaVasc Study Group, Can low molecular weight heparin replace unfractionated heparin during peripheral arterial reconstruction? An open label prospective randomized controlled trial. J Vasc Surg. 39(5): 977-84 (2004).
- Ciccone MM, Cortese F, Corbo F, et al. Bemiparin, an effective and safe low molecular weight heparin: A review. Vascul Pharmacol. 62(1): 32-7 (2014).
- Yamane H, Araki R, Doi A, et al. A successful case of “temporary endoluminal bypass technique” using a guide extension catheter during thrombolysis for acute limb ischemia in the non-stenting zone. J Cardiol Cases. 2: 57 (2020).
- Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC Guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries Endorsed by: The European Stroke Organization (ESO) The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). ESC Scientific Document Group. Eur Heart J. 39: 763-816 (2018).