Research Article - Interventional Cardiology (2011) Volume 3, Issue 6
Influence of metabolic syndrome on outcome after percutaneous coronary intervention
- Corresponding Author:
- Deepak L Bhatt
VA Boston Healthcare System, Brigham and Women’s Hospital
Harvard Medical School, Boston, MA, USA
E-mail: dlbhattmd@post.harvard.edu
Abstract
Keywords
bare-metal stents, drug-eluting stents, major adverse cardiac events, metabolic syndrome, percutaneous coronary intervention
Metabolic syndrome (MetSyn) is the term applied to identify a constellation of factors, namely dyslipidemia, abdominal obesity, glucose intolerance and hypertension, recognized many years ago by Reaven et al. as insulin resistance syndrome, syndrome X or the deadly quartet [1]. In 2001, the National Cholesterol Education Program (adult treatment panel [ATP] III) defined MetSyn to highlight the importance of increased risk of cardiovascular disease associated with MetSyn [2]. According to ATP III, MetSyn is defined as the presence of any three of the following five traits:
▪ Abdominal obesity, defined as a waist circumference in men >102 cm (40 in) and in women >88 cm (35 in);
▪ Serum triglycerides ≥150 mg/dl (1.7 mmol/l);
▪ Serum high-density lipoprotein (HDL) cholesterol <40 mg/dl (1 mmol/l) in men and <50mg/dl (1.3 mmol/l) in women;
▪ Blood pressure ≥130/85 mmHg;
▪ Fasting plasma glucose (FPG) ≥110 mg/dl (6.1 mmol/l).
In October 2009, the MetSyn criteria were updated in a statement from the International Diabetes Federation, American Heart Association, National Heart, Lung and Blood Institute, and others, which included lowering the threshold for abnormal fasting glucose to 100 mg/dl and included diabetes in the hyperglycemia trait definition, use of drugs for lipid control or blood pressure control in the dyslipidemia and hypertension trait definitions, respectively and ethnic specific measures of waist circumference [3].
With the obesity pandemic, the incidence of MetSyn has greatly increased worldwide and the prevalence is estimated to be approximately 20% in the adult population in the USA [4–6]. MetSyn is associated with an increased risk of cardiovascular disease and can be used to predict the new onset of diabetes [7–10]. MetSyn is also associated with worse outcomes after coronary artery bypass grafting (CABG) [11]. However, the data with respect to effect of MetSyn on outcomes after percutaneous coronary interventions (PCI) have been mixed [12–16]. Due to disparate findings of various studies, we studied the effect of MetSyn and its components on outcomes in a large group of patients who underwent PCI with bare-metal stents (BMS) at the Cleveland Clinic (OH, USA) using the Cleveland Clinic interventional database.
Methods
▪ Study population
All patients who underwent PCI at the Cleveland Clinic are followed in a prospective database. Between January 2000 and November 2002, 6759 patients had PCI at the Cleveland Clinic. Patients were included for this analysis if they had complete information about lipids, principally triglycerides and HDL cholesterol, BMI, history of elevated blood pressure and history of diabetes mellitus. Fasting lipid values obtained within 5 days of the PCI, were extracted from the laboratory database. We chose to use BMI as waist circumference was not available and BMI has been validated as an alternative to measuring waist circumference in the definition of MetSyn in previous studies [17]. Fasting glucose was not routinely measured in all patients who underwent PCI and so a history of treated diabetes mellitus was used instead. Complete data regarding all of the components of MetSyn were only available in 2362 of the 6759 patients and hence they formed the study cohort. Baseline characteristics, medication use and procedural variables were collected at the time of procedure. Interventional procedures were performed as per conventional standards and as deemed by the interventional cardiologist. Research coordinators prospectively collected information about myocardial infarction (MI), or repeat revascularization at the time of the procedure and at 1-year follow-up. Mortality data were obtained from the social security death index. The institutional review board approved the use of the interventional registry and subsequent data analysis. Participants have provided prior informed consent to be included in the interventional registry.
▪ Definitions
For our analysis, the components of MetSyn were defined as follows:
▪ Obesity (BMI ≥30 kg/m2);
▪ History of treated diabetes;
▪ History of treated increased blood pressure;
▪ Low HDL cholesterol <40 mg/dl in men and <50 mg/dl in women and/or fasting triglycerides ≥150 mg/dl).
The patients were divided into five groups, from group zero, which consisted of patients with none of the components, to group four, which consisted of patients with all four components of MetSyn. All components were given equal importance. For example, if a patient had any one of the four components, he would be treated as group one, any two components as group two and so on. This was performed in order to study the effect of each of the individual components as well as the combination of the components on the outcomes after PCI.
Statistical analysis
Chi-squared tests were used for categorical variables. Log-rank tests were used to compare event-free survival in patients with one, two, three and four of the MetSyn components to patients with none of the components. Hazard ratios (HR) (with 95% CI) for major adverse cardiac events (MACE) were described. Multivariate analysis was performed using Cox regression models using MetSyn as a cumulative score after assessing the risk associated with the increasing risk components and adjusted for univariate predictors of MACE. All statistical analyses were performed with STATA 8.2 (College Station, TX, USA) statistical package. Results were considered statistically significant if p < 0.05.
Results
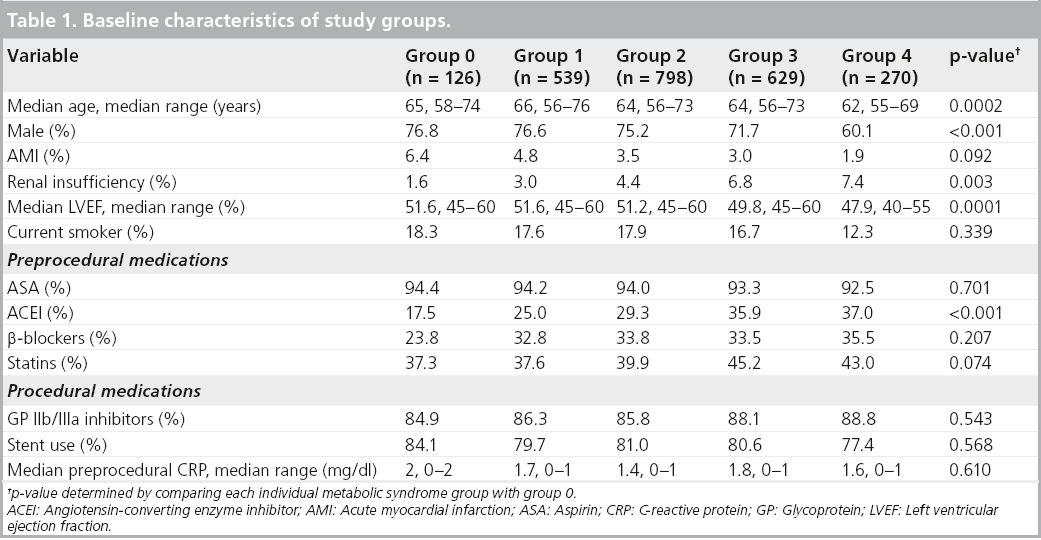
The baseline characteristics of the 2362 patients who formed the different MetSyn groups are shown in Table 1. Age, gender, left ventricular ejection fraction (LVEF) and renal insufficiency were significantly different across the groups. Medication use was not significantly different except angiotensin-converting enzyme (ACE) inhibitor use. Prior MI, smoking, stent use and preprocedural C-reactive protein (CRP) were not significantly different across the various groups.
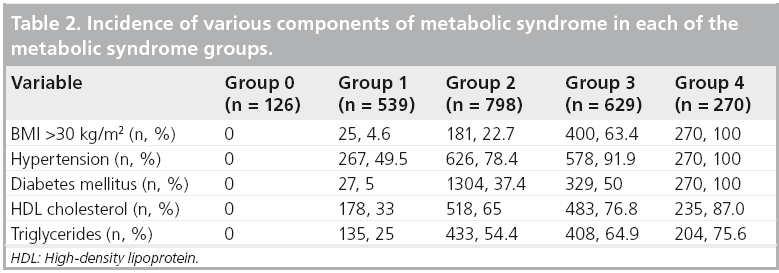
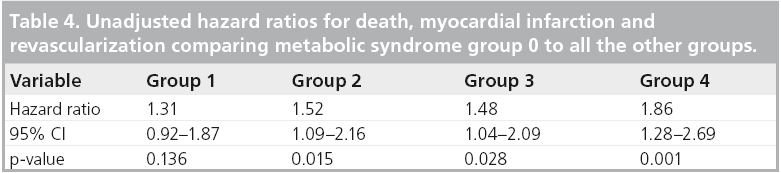
Table 2 shows the prevalence of the different MetSyn components in each group. MACE are summarized in Table 3. There were a total of 296 deaths, 103 MI and 551 revascularization procedures (PCI) over a follow-up of 60 months (median 36 months, interquartile range 12–47 months) resulting in a total of 950 MACE. The combined end point of death, MI and revascularization was significantly different across the groups. The adjusted hazard for the combined end point of death, MI and revascularization increased by 65% in group four, with all four of the MetSyn risk factors (HR: 1.65; 95% CI: 1.11–2.45; p = 0.001). The unadjusted risk for death, MI and revascularization increased in all groups as shown in Table 4. Compared with the group with no MetSyn components, all other groups demonstrated a significant increase in risk for combined end point of death, MI and revascularization.
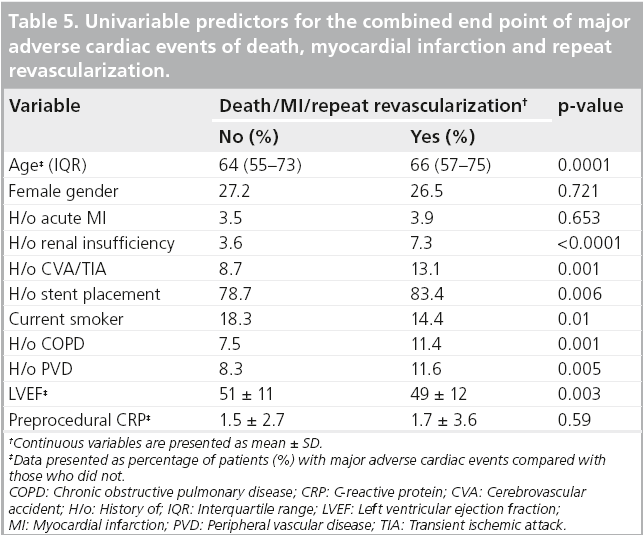
Figure 1 shows the Kaplan–Meier survival curves for MACE according to the MetSyn group. As depicted, the risk is worse with the increasing number of MetSyn components (p = 0.0045). Table 5 shows the univariable predictors of the combined end point of death, MI and revascularization. Age, renal insufficiency, stent placement, history of peripheral arterial disease, history of prior cerebrovascular accident or transient ischemic attack and lower LVEF were found to be significant predictors. In Cox proportional hazards modeling, adjusting for potential confounders (age, gender, renal insufficiency, LVEF, stent placement, peripheral vascular disease, glycoprotein IIb/IIIa use, statins, ACE inhibitors and b-blockers), increasing MetSyn risk factors (i.e., increasing MetSyn group) was associated with a significant reduction in event-free survival (Table 6).
Figure 1: Kaplan–Meier survival curves for death, myocardial infarction and revascularization stratified by metabolic syndrome groups over a follow-up of 60 months (median 36 months, range 12–47 months).
Discussion
Our study suggests that in patients who underwent PCI during the BMS era at the Cleveland Clinic from January 2000 until November 2002, there was an incremental risk of death, MI and revascularization associated with the presence of risk factors that constitute the MetSyn. The risk appears to be worse with increasing number of MetSyn components. Patient survival was worse as the number of MetSyn risk factors increased.
Presence of MetSyn has been shown to worsen outcomes following CABG [11], and previous studies have shown disparate results for risk of MetSyn with PCI [13–16]. In contrast, more patients were included in our study with high rates of stent implantation, although this was exclusively with BMS. In our study, we found MetSyn to be predictive of MACE, which may be due to the inclusion of treated diabetic patients. As noted previously, most of the adverse events may have been due to need for repeat revascularization.
It is well known that diabetes increases the risk for mortality after PCI [17]. In our analysis, diabetes mellitus was not studied as a separate covariate from the other MetSyn components, to assess for individual risk of either total mortality or repeat revascularization from the various components. Also within MetSyn components, low HDL cholesterol and high fasting glucose seem to have the best predictive ability for prediction of adverse events [18]. In our cohort, fasting blood glucose levels were not available and hence we did not study the effect of this on MACE. Similarly, the present study is limited to BMS and may not apply to drug-eluting stents.
In summary, patients with risk factors that constitute MetSyn, who underwent PCI are at higher risk for MACE over long-term followup. Identification and aggressive treatment of patients with MetSyn is needed to mitigate this increased risk.
Limitations
There are several limitations to our study. This is an analysis from a single center registry and BMS were used for PCI. As in observational studies, our study is limited by the data that were collected and included in the PCI database and hence there may be unmeasured confounders that may not have been adjusted for. Due to lack of complete information regarding the various MetSyn components, more than two-thirds of the total patients eligible were excluded from the analysis. Furthermore, the definition of MetSyn used in our study is not concordant with ATP III guidelines as we used surrogate measures of BMI for waist circumference and treated diabetes mellitus for impaired fasting glucose.
Conclusion
Patients with MetSyn have an increased risk of adverse outcomes after PCI with BMS. As the prevalence and incidence of this syndrome is increasing worldwide, it is imperative that we identify whether aggressive treatment of patients with MetSyn will impact their outcomes after revascularization.
Future perspective
MetSyn will continue to increase in the next decade due to worldwide proliferation in rates of obesity. The rate of coronary artery disease and subsequent PCI will likely grow and hence it is important to recognize and treat these patients aggressively. Our study sheds light on this important issue, albeit with the use of BMS. However, the risk exists even with the use of drug-eluting stents and hence it is imperative to treat the metabolic abnormalities to mitigate the complications.
Financial and competing interests disclosure
D Bhatt has received research grants from Amarin, AstraZeneca, Bristol–Myers Squibb, Eisai, Ethicon, Medtronic, Sanofi Aventis and The Medicines Company. DP Chew has served as a consultant for Sanofi-Aventis (Australia), Eli-Lily (Australia), The Medicines Company and CSL Biotherapies (Australia). V Nambi has received research support from NHLBI K-23, research grants from Gillson Longenbaugh Foundation, Gulf Coast Regional Foundation, has research collaboration with no financial support from GE, Medipattern and Tomtec, is a national monitor for study sponsored by Anthera, is on the virtual advisory board for Roche and is speaker for the AHA. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Executive summary
▪ Metabolic syndrome (MetSyn) is a growing public health problem, due to an increase in obesity worldwide.
▪ MetSyn increases risk for patients undergoing coronary artery bypass grafting.
▪ Our study demonstrates increased risk associated with percutaneous coronary intervention with bare-metal stents in patients with MetSyn and is independently associated with risk.
▪ It is important to identify and treat patients with MetSyn aggressively to mitigate risk for adverse events after percutaneous coronary intervention.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Reaven GM, Chen YD. Insulin resistance, its consequences, and coronary heart disease. Must we choose one culprit? Circulation 93(10), 1780–1783 (1996).
- Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285(19), 2486–2497 (2001).
- Alberti KG, Eckel RH, Grundy SM et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation task force on epidemiology and prevention, National Heart, Lung, And Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society and International Association for the Study of Obesity. Circulation 120(16), 1640–1645 (2009).
- Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch. Intern. Med. 163(4), 427–436 (2003).
- Alexander CM, Landsman PB, Teutsch SM, Haffner SM. NCEP-defined metabolic syndrome, diabetes and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes 52(5), 1210–1214 (2003).
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 287(3), 356–359 (2002).
- Sattar N, Gaw A, Scherbakova O et al. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation 108(4), 414–419 (2003).
- Lakka HM, Laaksonen DE, Lakka TA et al. The metabolic syndrome and total and cardiovascular disease mortality in middleaged men. JAMA 288(21), 2709–2716 (2002).
- Isomaa B, Almgren P, Tuomi T et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24(4), 683–689 (2001).
- Wilson PW, Kannel WB, Silbershatz H, D’Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch. Intern. Med. 159(10), 1104–1109 (1999).
- Sprecher DL, Pearce GL. How deadly is the ‘deadly quartet’? A post-CABG evaluation. J. Am. Coll. Cardiol. 36(4), 1159–1165 (2000).
- Bin H, Yujie Z, Yuyang L et al. Impact of metabolic syndrome on clinical outcomes after drug-eluting stent implantation in patients with coronary artery disease. Angiology 62(6), 440–446 (2011).
- Kasai T, Miyauchi K, Kurata T et al. Impact of metabolic syndrome among patients with and without diabetes mellitus on long-term outcomes after percutaneous coronary intervention. Hypertens. Res. 31(2), 235–241 (2008).
- Hoffmann R, Stellbrink E, Schroder J et al. Impact of the metabolic syndrome on angiographic and clinical events after coronary intervention using bare-metal or sirolimus-eluting stents. Am. J. Cardiol. 100(9), 1347–1352 (2007).
- Kasai T, Miyauchi K, Kurata T et al. Prognostic value of the metabolic syndrome for long-term outcomes in patients undergoing percutaneous coronary intervention. Circ. J. 70(12), 1531–1537 (2006).
- Rana JS, Monraats PS, Zwinderman AH et al. Metabolic syndrome and risk of restenosis in patients undergoing percutaneous coronary intervention. Diabetes Care 28(4), 873–877 (2005).
- Wilson SR, Vakili BA, Sherman W, Sanborn TA, Brown DL. Effect of diabetes on long-term mortality following contemporary percutaneous coronary intervention: analysis of 4,284 cases. Diabetes Care 27(5), 1137–1142 (2004).
- Anderson JL, Horne BD, Jones HU et al. Which features of the metabolic syndrome predict the prevalence and clinical outcomes of angiographic coronary artery disease? Cardiology 101(4), 185–193 (2004).
▪ One of the first articles that described the importance of insulin resistance.
▪▪ Early definition of metabolic syndrome (MetSyn).
▪▪ Revised definition of MetSyn.
▪ Important description of influence of MetSyn on outcomes after coronary artery bypass grafting.
▪▪ Report of influence of MetSyn on outcomes after percutaneous coronary intervention with drug-eluting stents.