Research Article - Interventional Cardiology (2024) Volume 16, Issue 5
In-hospital mortality and associated factors among adult patients with acute heart failure in a tertiary hospital, Harar, Eastern Ethiopia: A cross-sectional study
- Corresponding Author:
- Mesay Dechasa
Department of Clinical Pharmacy, Haramaya University, Harar, Ethiopia,
E-mail: Mesay.Dechasa@haramaya.edu.et
Received date: 09-Oct-2024, Manuscript No. FMIC-24-149909; Editor assigned: 11-Oct-2024, PreQC No. FMIC-24-149909 (PQ); Reviewed date: 25-Oct-2024, QC No. FMIC-24-149909; Revised date: 01-Nov-2024, Manuscript No. FMIC-24-149909 (R); Published date: 08-Nov-2024, DOI: Crossref
Abstract
Background: Acute heart failure is the gradual or rapid change of heart failure signs and symptoms, which poses a unique diagnostic and management challenge, requiring urgent therapy. It is responsible for nearly one million hospitalizations each year globally with rising rates. Despite therapeutic advances, it is associated with poor prognosis. Therefore, his study aimed to assess in-hospital mortality and its associated factors among adult acute heart failure patients in a tertiary hospital, Harar, Eastern Ethiopia.
Methods: A hospital-based retrospective cross-sectional study was employed among 454 adult acute heart failure patients treated in the medical ward of Haramaya University Hiwot Fana Comprehensive Specialized Hospital from June 01, 2016 to May 31, 2021. Data was collected using structured data abstraction format from July 15 to August 14, 2021. Collected data was entered to Epi-Data version 3.1, exported to and analyzed using Statistical Package for Social Science (SPSS) version 21.0. Bivariate and multivariate logistic regression was used to identify factors associated with in-hospital mortality.
Results: A total of 454 acute heart failure patient’s medical records were reviewed. More than half, 282 (62.1%) of patients were females. The median age of patients was 45 years (± 28 IQR). In-hospital mortality was 18.9% and it was more prevalent in the first week of admission, 61 (70.9%). Sex (female) (Adjusted Odds Ratio (AOR)=2.83, p=0.001)), having smoking history (AOR=2.51, p=0.031), generalized body swelling (AOR=2.67, p=0.001), hypotension (AOR=4.56, p=0.001) and tachycardia (AOR=4.57, p=0.000) were factors associated with in-hospital mortality.
Conclusion: In-hospital mortality is found to be very high among acute heart failure adult patients. Therefore, dedicated programs need to be developed to reduce mortality from acute heart failure and further prospective studies should be conducted to investigate the problem in-depth.
Keywords
Acute heart failure • Cardiac output • Cardiogenic shock • Pulmonary congestion • Hyperuricemia
Abbreviations
ACEI: Angiotensin-Converting Enzyme Inhibitors; ADHF: Acute Decompensated Heart Failure; AHF: Acute Heart Failure; HFCSH: Hiwot Fana Comprehensive Specialized Hospital; LVSD: Left Ventricular Systolic Dysfunction; SBP: Systolic Blood Pressure; HF: Heart Failure
Introduction
Heart Failure (HF) is a clinical syndrome characterized by classic symptoms and signs which occurs on exertion or at rest [1]. HF is caused by a structural and/or functional cardiac abnormality, resulting in reduced and/ or elevated intra-cardiac pressure. This pressure impairs the ability of the heart to fill with blood at normal pressure or eject blood adequate to fulfill the needs of the metabolizing organs. HF remains a major cause of mortality and morbidity [2-4].
AHF is defined as a gradual or rapid change in heart failure syndromes, which poses a unique diagnostic and management challenge and requires urgent therapy [5]. AHF also covers a wide range of the spectrum, which ranges from mild exacerbations with gradual increases in edema to cardiogenic shock [6]. These symptoms in AHF are the result of severe pulmonary congestion due to reduced left ventricular filling pressures with or without low cardiac output [7].
AHF is responsible for nearly one million hospitalizations each year with rising rates and after initial hospitalization, 25% of patients are readmitted at 30 days, 35% of which are due to a new exacerbation [8]. In Africa, 7% to 10% of all medical admissions to hospitals are due to cardiovascular disease, with heart failure contributing to 3% to 7% [9]. There were no data on the prevalence of heart failure in the general population in Ethiopia. A study in single setting at Dabat district, northwest Ethiopia, revealed that out of 216,420 populations 32.2% had heart disease. Hospitalization due to AHF is associated with several factors and comorbidities like older age, female gender, hyperuricemia, obesity, atrial fibrillation, peripheral artery disease and chronic kidney disease [10].
Once diagnosed, AHF patients may be classified using different methods based on presentation. Depending on whether patients have a history of HF or not, it is classified as ADHF which occurs in patients with heart failure history and de novo AHF that occurs in individuals with no history of heart failure”. Based on SBP at presentation, AHF is classified as “hypertensive AHF (SBP>140 mmHg), normotensive AHF (SBP is between 90-140 mmHg) and hypotensive AHF (SBP<90 mmHg)”. Depending on the hemodynamic condition of the patients, it is classified as “warm and dry (well-perfused without congestion), warm and wet (wellperfused but congested), cold and dry (hypo-perfusion without congestion) and cold and wet (hypo-perfusion and congestion)”. Based on Left Ventricular Ejection Fraction (LVEF), AHF is classified as “AHF with reduced ejection fraction and AHF with preserved ejection fraction” [11].
Depending on congestive and organ perfusion status the management approaches of AHF involves relief of symptoms, restoration of systemic tissue perfusion via improved cardiac output and minimization of further cardiac damage. These can be attained by using diuretics, neuro-hormonal antagonists and inotropes [12,13]. Despite therapeutic advances, the prognosis of AHF is poor and re-hospitalization is high which is 25% to 30% [14]. HF in general is associated with a huge economic burden which the overall cost is estimated at $108 billion globally and $28 million in Ethiopia per annum [15].
The burden of AHF is high in resource-limited countries where patient’s low levels of education and income also contribute [16]. In sub-Saharan Africa, many of the equipment and drugs commonly used to diagnose and treat AHF in resource-rich settings are lacking [17,18]. In Ethiopia, in addition to this lack of equipment and drugs, knowledge about cardiovascular risk factors is at suboptimal levels (46%) and AHF patients are of middle age this is an additional burden due to the impact on productivity [19-21].
Regarding in-hospital mortality from AHF, it is 1.5% to 5.3% in developed countries [22-24]. However, it is very high in Ethiopia (17.2% to 24.4%) [25]. One single setting study showed a high burden of the HF (32.2% of the population had heart disease) and household food insecurity was among factors associated with the non-communicable disease which include heart disease, HF is the third most common reason for immediate admissions, with a prevalence of 16.0% among patients admitted to medical wards [26,27].
Throughout the country, hospital-based studies on AHF that look into in-hospital mortality of the disease and its associated factors are scarce and are lacking in this study setting. Therefore, this study aimed to assess in-hospital mortality and its associated factors among adult patients with acute heart failure Fana Comprehensive Specialized Hospital from 15 July to 14 August 2021, Harar, Ethiopia.
This study provides insights regarding in-hospital mortality of AHF and its associated factors among adult patients. Therefore, primarily it encourages hospital managers and each health professionals who participate in patient care to take measure in the spirit of improving the treatment outcome of AHF by forwarding necessary recommendations for possible changes and to scale up current standard of care in HFSCH and other similar hospitals. This study is also a stepping-stone for the study setting to alarm other researchers to investigate the problem in-depth throughout the country. Furthermore, the finding of this study can be used as input for development of treatment guidelines need to be modified for the future at the national level.
Materials and Methods
Study design, setting and period
The retrospective cross-sectional study was conducted from July 15 to August 14, 2021 at HFCSH, Eastern Ethiopia. HFCSH is a specialized hospital in Eastern Ethiopia, which is found in Harar town, 526 km from Addis Ababa, the capital city of Ethiopia. It is serving as a referral hospital for the entire eastern part of the country including Eastern Oromia, Dire Dawa city administration, Harari and Somali regional states. There are different wards and clinics within the hospital that provide services for the community such as medical ward, pediatric ward, surgery ward, gynecologic and obstetrics ward, oncology ward, antenatal clinic, dental clinic, a tuberculosis clinic, ante-retroviral therapy clinic, dermatology clinic and ophthalmologic clinic. The medical ward has 22 beds.
Population
All adult patients with a diagnosis of AHF treated at HFCSH were source population. All adult patients with a diagnosis of AHF treated at HFCSH in the past five years (from June 01, 2016 to May 31, 2021) who fulfilled the inclusion criteria were the study population.
Eligibility criteria
All adult patients whose was age less than 18 years with a confirmed diagnosis of AHF and treated during the data retrieval period at the medical ward of HFCSH were included in this study. However, all patients with unknown outcome (referred or disappeared) and lost and/or incomplete patients’ medical records were excluded from the study.
Sample size determination
For the first two objectives sample size of the study was calculated using single population proportion formula by considering the following assumptions: Prevalence of in-hospital mortality (p)=17.2% taken from another similar study, Confidence Level (CI)=95% and corresponding Z score of 1.96, margin of error (W)=5%.
Thus sample size was, n=(Zα/2)2 p (1-p)/w2=(1.96)2*0.172*0.828/ (0.05)2=218.8. For the objective of factors associated with inhospital mortality sample size was calculated using Epi-Info version 7.2.4.0 (Table 1).
| Determinants of treatment outcome | |||||
|---|---|---|---|---|---|
| Factors | Assumptions | % Exposed | % Unexposed | Reference | Sample size (N) |
| Smoking | CI: 95% Power:80% Ratio:1:1 | 44.4 | 15.6 | -20 | 80 |
| Diabetes mellitus | CI: 95% Power:80% Ratio:1:1 | 50 | 15.6 | -20 | 60 |
| Pulmonary hypertension | CI: 95% Power:80% Ratio:1:1 | 15.1 | 41.2 | -20 | 94 |
| Chronic kidney disease | CI: 95% Power:80% Ratio:1:1 | 39.59 | 22.44 | -25 | 230 |
| Heart rate>100beats/min at presentation | CI: 95% Power:80% Ratio:1:1 | 34.3 | 47.9 | -25 | 412 |
Abbreviations: CI: Confidence interval
Table 1: Sample size calculation for factors associated with in-hospital mortality of acute heart failure patients using Epi-Info software (version 7.2.4.0).
Therefore, by adding 10% for contingency on the largest sample size, the calculated sample size was found to be 454 adult patients with AHF.
Sampling procedures and sampling techniques
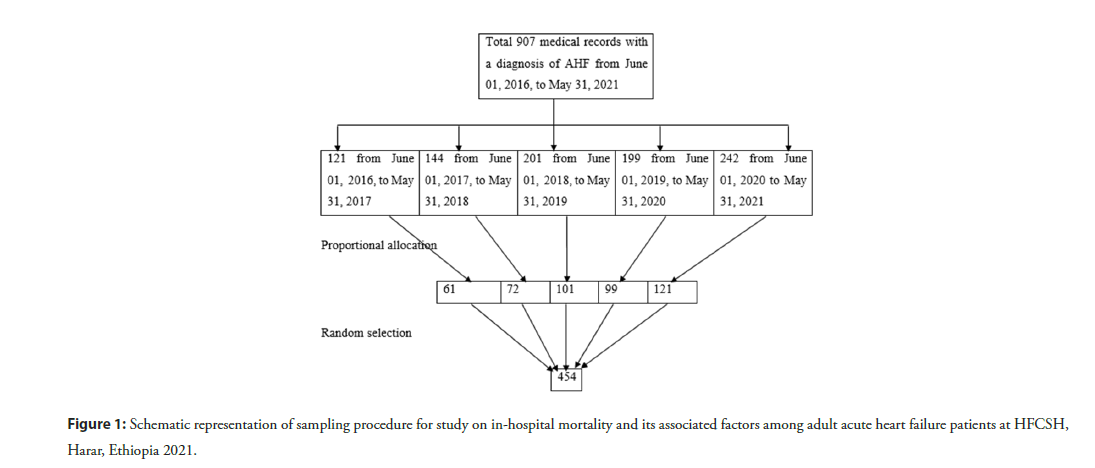
The 907 adult patients were treated at HFCSH for AHF during the last five years. That is 121, 144, 201, 199, 242 patients from June 01, 2016, to May 31, 2021, each year respectively.
For this study, record numbers of those patients’ medical records were obtained from the medical registration book of the Medical ward of HFCSH. Finally, 454 patients’ medical records included in the study were selected using proportionally allocated simple random sampling technique (Figure 1).
Figure 1: Schematic representation of sampling procedure for study on in-hospital mortality and its associated factors among adult acute heart failure patients at HFCSH, Harar, Ethiopia 2021.
Data collection method
Data were collected from patients’ medical records using an English version of structured and pretested data abstraction format prepared by reviewing different pieces of literature on similar topics, which consists of socio-demographic information, vital signs at presentation, clinical presentations, comorbidities, laboratory and radiologic findings.
Record numbers of the individual patients’ medical cards were obtained from medical registration book of medical ward and the numbers of those patients’ medical cards to be included in the study were randomly selected using lottery method. Then using randomly selected numbers, patients’ medical cards were drawn from the hospital card room. In-hospital mortality was confirmed by principal investigator from discharge summary. Finally, the data were collected from those medical cards by two clinical pharmacists and one clinical nurse.
Operational definitions
Acute heart failure: Sign and symptoms of new-onset of heart failure or decompensation or worsening of ADHF [28].
In-hospital mortality: AHF patient died in the hospital after he/she was admitted to the medical ward which confirmed by physician’s death summary [29].
Elevated blood pressure: Systemic blood pressure of greater than 120/80 mmHg.
Data quality control
Necessary training was given for data collectors on the contents of the data collecting tool, data collection procedures and consent was obtained from head of hospital before data collection. A pretest was conducted on randomly selected 5% of the sample size (twenty-three AHF patient’s medical records) before the actual data collection. Then, adjustments were made on the tool for final data collection. The supervisors carried close supervision out daily during the data collection time. The principal investigator checked data for completeness, clarity, consistency and accuracy.
Data analysis procedures
The collected data were entered to Epi-data (version 3.1), transferred to and analyzed using SPSS version 21.0®. Quantitative variables were reported as a median and interquartile range. Categorical variables were presented using percentages and frequency. Bivariate and multivariate logistic regression was used to analyze factors associated with treatment outcome. Each variable with no missing value were checked for association against the outcome variable in the binary model. Then, Variables with p<0.25 in the bivariate model analyses were entered into the multivariate model.
The Binary Logistic Regression model fitness was checked by Hosmer-Lemeshow statistic. Multicollinearity test was carried out to see the correlation between independent variables using Variance Inflation Factor (VIF). Crude Odds Ratio (COR) and Adjusted Odds Ratio (AOR) were calculated with the 95% confidence interval to measure the strength of the association between the outcome and independent variables. The variable with a p-value less than 0.05 in the multivariable analysis was considered significantly associated with in-hospital mortality.
Results
Socio-demographic characteristics
Out of 454 study participants, more than half 282 (62.1%) of them were females. The median age of patients was 45 years (± 28 IQR) and the highest percent 192 (42.3%) of them were between the age of 40 and 61 years. About 404 (89.0%) of the participants were nonsmokers (Table 2).
| Variables | Frequency (%) |
|---|---|
| Sex | |
| Female | 282 (62.1) |
| Male | 172 (37.9) |
| Age in years | |
| 18-39 | 163 (35.9) |
| 40-61 | 192 (42.3) |
| 61 and above | 99 (21.8) |
| Cigarette smoking history | |
| Non-smokers | 404 (89.0) |
| Smoker | 50 (11.0) |
Table 2: Socio-demographic characteristics of acute heart failure adult patients treated from June 01, 2016 to May 31, 2021 at HFCSH, Harar, Eastern Ethiopia (N=454).
| Medications | In hospital Frequency (%) | At discharge Frequency (%) |
|---|---|---|
| Furosemide | 442 (97.4) | 358 (97.3) |
| Spironolactone | 237 (52.2) | 210 (57.1) |
| Enalapril | 163 (35.9) | 152 (41.3) |
| Aspirin | 129 (28.4) | 116 (31.5) |
| Digoxin | 111 (24.4) | 70 (19.0) |
| Intranasal oxygen | 73 (16.1) | - |
| Atorvastatin | 47 (10.4) | 38 (10.3) |
| Simvastatin | 41 (9.0) | 28 (7.6) |
| Clopidogrel | 39 (8.6) | 13 (3.5) |
| Dopamine | 30 (6.6) | - |
| Amlodipine | 18 (4) | 8 (2.2) |
| Nifedipin | 16 (3.5) | 7 (1.9) |
| Atenolol | 7 (1.5) | 4 (1.1) |
Table 3: Medications used for treatment of adult patients with acute heart failure at HFCSH during the study period, Harar, Eastern Ethiopia, 2021 (N=454).
| In-hospital mortality | Frequency (%) | 95% CI |
|---|---|---|
| Survived | 368 (81.1%) | 1 |
| In-hospital mortality | 86 (18.9%) | 15.3-22.5 |
| ≥1day and ≤ week 1 of admission | 61 (70.9%) | |
| > week1 and ≤ 30 days admission | 24 (27.9%) | |
| >30 days | 1 (1.2%) |
Table 4: In-hospital mortality of acute heart failure patients at HFCSH, Harar, Eastern Ethiopia, from June 01, 2016 to May 31, 2021 (N=454).
Clinical characteristics of participants
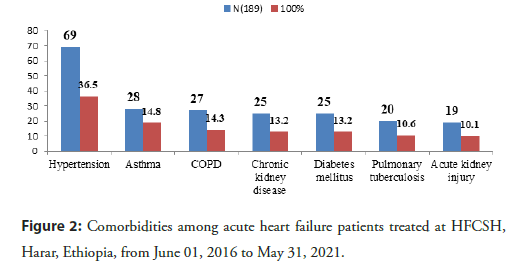
Among comorbidities of AHF, patient’s hypertension was the most common 69 (36.5%) followed by asthma 28 (14.8%), (Figure 2). Pneumonia 115 (44.7%) followed by drug discontinuation 94 (36.6%) were the major precipitating factors among acute heart failure patients. The majority of the patients had normal vital signs except blood pressure was elevated in 221 (48.7%) and tachypnea in 392 (86.3%) of patients at admission.
Figure 2: Comorbidities among acute heart failure patients treated at HFCSH, Harar, Ethiopia, from June 01, 2016 to May 31, 2021.
Medication used for treatment of acute heart failure
Among medications used treatment of AHF, furosemide was most commonly used 442 (97.4%) and 358 (97.3%) both in hospital and at discharge, respectively. Atenolol was the least medications used for treatment of adult patients with acute heart failure.
In-hospital mortality
From 454 study participants, 368 (81.1%) were survived and in-hospital mortality was 86 (18.9%) at a 95% CI of 15.3- 22.5. In-hospital mortality was more prevalent in the first week of admission, 61 (70.9%) and median time to death was 9 days (Tables 3 and 4).
Factors associated with in-hospital mortality
In the bivariate model, eight variables were associated with inhospital mortality at a p-value <0.25. The associated variables were; Sex (p=0.106), smoking history (p=0.180), presence of generalized body swelling (p=0.000), murmur sound (0.183), vomiting (0.026), blood pressure (hypotension) (p=0.000), heart rate ((tachycardia) (p=0.000), respiratory rate (bradypnea (p=0.098) and tachypnea (p=0.051)) at admission. In multivariate binary logistic regression analysis, five variables: Sex (female), smoking history, presence of generalized body swelling, blood pressure (hypotension) and heart rate (tachycardia) were retained in the final models.
This study showed that the odds of in-hospital mortality among females was 2.83 times than males (AOR=2.83; 95% CI: 1.50- 5.33, p=0.001). The odds of in-hospital mortality among those who had a smoking history were 2.51 times higher (AOR=2.51; 95% CI: 1.09-5.77, p=0.031) when compared with those who had no smoking history. Similarly, the odds of in-hospital mortality among those who had generalized body swelling at admission were 2.67 times higher as compared to those who had no generalized body swelling (AOR=2.67; 95% CI: 1.49-4.76, p=0.001). Inhospital mortality among patients who had hypotension at admission was 4.56 times more likely (AOR=4.56; 95% CI: 1.89- 10.10, p=0.001) as compared to those with normal blood pressure. The likelihoods of in-hospital mortality among those who had tachycardia at admission were 4.57 times (AOR=4.57; 95% CI: 2.57-8.10, p=0.000) higher as compared to those who had normal heart rates (Table 5).
| Variables | Treatment outcomes | Bivariate | Multivariate | |
|---|---|---|---|---|
| Mortality (86) | Survival (368) | COR (95% CI) | AOR (95% CI) | |
| Sex | ||||
| Male | 26 | 146 | 1 | 1 |
| Female | 60 | 222 | 1.52 (0.92-2.52) | 2.83 (1.50-5.33)* |
| Smoking history | ||||
| Non smoker | 73 | 331 | 1 | 1 |
| Smoker | 13 | 37 | 1.59 (0.81-3.15) | 2.51 (1.09-5.77)* |
| Generalized body swelling | ||||
| No | 23 | 181 | 1 | 1 |
| Yes | 63 | 187 | 2.65 (1.58-4.46) | 2.67 (1.49-4.76)* |
| Murmur at admission | ||||
| No | 42 | 209 | 1 | 1 |
| Yes | 44 | 159 | 1.38 (0.86-2.20) | 1.33 (0.78-2.27) |
| Vomiting at admission | ||||
| No | 58 | 290 | 1 | 1 |
| Yes | 28 | 78 | 1.79 (1.07-3.01) | 1.70 (0-94-3.07) |
| Blood pressure at admission | ||||
| Normal | 34 | 163 | 1 | 1 |
| Hypotension | 18 | 18 | 4.79 (2.26-10.16) | 4.56 (1.89-10.10)* |
| Elevated | 34 | 187 | 0.87 (0.52-1.47) | 0.68 (0.38-1.22) |
| Heart rate | ||||
| Normal | 25 | 230 | 1 | 1 |
| Bradycardia | 3 | 14 | 1.97 (0.53-7.33) | 0.73 (0.08-6.91) |
| Tachycardia | 58 | 124 | 4.30 (2.57-7.22) | 4.57 (2.57-8.10)* |
| Respiratory rate | ||||
| Normal | 5 | 51 | 1 | 1 |
| Bradypnea | 2 | 4 | 5.10 (0.74-35.14) | 2.32 (0.11-49.55) |
| Tachypnea | 79 | 313 | 2.57 (0.99-6.67) | 1.87 (0.64-5.55) |
Abbreviations: COR: Crude Odds Ratio; AOR: Adjusted Odds Ratio; *indicates significantly associated at p<0.05.
Table 5: Factors associated with in-hospital mortality of acute heart failure patients treated at HFCSH, Harar, Ethiopia, from June 01 2016 to May 31, 2021 (N=454).
Discussion
The findings of this study indicated that of AHF patients were higher among young. The patients in the current study are older than previous study in Ethiopia, median 45 years versus 34 years. However, our patients are younger than AHF patients are in global study and in developed countries, median age of 67 to 79 years [30,31]. The discrepancy might be due to high level of awareness on prevention of cardiovascular disease, age cut-point differences of participants and life expectance of patients in developed countries. The overall in-hospital mortality was found to be 18.9% at a 95% confidence interval of 15.3% to 22.5%. Being female, having a smoking history, presence of generalized body swelling, hypotension and tachycardia at admission were factors associated with in-hospital mortality.
The magnitude of in-hospital mortality found in this study is 18.9% in the current study. A prospective study conducted at Tikur Anbessa Specialized Hospital, Ethiopia (17.2%) and a retrospective study conducted at Yaoundé Central Hospital, Cameroon (18.45%) reported similar magnitude of in-hospital mortality [32]. On the other hand, the finding of this study is higher than the studies reported from Gondar Comprehensive Specialized Hospital (10.6%), Middle East and North Africa (5.4%), and European and Mediterranean countries 5.3%. This could be due to advanced health care service in these study settings as they included patients from developed countries. However, it is lower than the study conducted in Addis Ababa, Ethiopia (24.4%). The discrepancy might be due to patient’s age difference, patient care process and setting differences.
In this study, in-hospital mortality among females was 2.83 times more likely as compared to males. This might be attributable to a high proportion of female patients (62.1%) in this study. The finding is similar with the result reported from study conducted at St. Paul’s Hospital Millennium Medical College in Addis Ababa that showed the association of female sex with in-hospital mortality among heart failure patients.
The odds of in-hospital mortality were more than double among those who had a smoking history than those who had no smoking history. Cigarette smoking is well-established cardiovascular risk factor. It makes the heart work harder due to its blood pressure increasing effect and thus, negatively affect the treatment outcome of AHF [33,34]. Other studies also showed an association between smoking and in-hospital mortality among AHF patients [35].
In-hospital mortality among patients who had generalized body swelling at admission was found to be 2.67 times more likely as compared to those who had no generalized body swelling at admission in the current study. Generalized body swelling is the result of the activation of a series of humoral and neurohumoral mechanisms that promote sodium and water reabsorption by the kidneys and expansion of the extracellular fluid. It occurs after signs of dyspnea and fatigue, which means it is not an early sign of heart failure, indicating that the acute heart failure patients with generalized body swelling is relatively at an advanced stage which negatively affects the outcome of the treatment [36].
There were significant differences in clinical characteristics such as hypotension between survivors and non-survivors among acute heart failure patients. In-hospital mortality among patients who had hypotension was more than four times as compare to normotensive patients in present study. This may be due to the life threatening effect of shock. This finding is supported by other different studies [37,38].
The odds of in-hospital mortality were more than four times higher among those who had tachycardia than those with normal heart rates in this study. The possible explanation is that as tachycardia is a compensatory mechanism in heart failure to meet the body’s oxygen and nutrient requirement, over time it causes a rapid decline in left ventricular function and worsens the acutely failed heart resulting in poor treatment outcome (death). This finding is almost similar with other studies that showed mortality rate is higher among patients with tachycardia.
Conclusion
In this study, in-hospital mortality is very high, which is almost one in six among patients admitted to HFCSH with AHF. Being female, having a smoking history, presences of generalized body swelling, hypotension and tachycardia at admission were variables found to be significantly associated with in-hospital mortality among patients with AHF. Therefore, the current study outlined that there is a need for the reduction of in-hospital mortality among adult patients with acute heart failure in hospitals. Furthermore, a prospective research with strong design regarding in-hospital mortality and its associated factors among AHF is need to be conducted to investigate the problem in-depth and to establish causality.
Strength and limitations of the study
Although this study is among a few of its kind and it can serve as a stepping-stone for further investigation, it has some limitations. First, the study was based on a retrospective chart review. Thus, due to poor documentation, important variables like adherence and adverse drug effect were missed. This might have influenced the results. Second, the data was collected from a single health facility and generalizability of the results is limited. Finally, since this study used cross-sectional study design, it cannot make a causal inference. Therefore, the authors recommend further follow-up study with stronger study design to address these limitations.
Availability of Data and Materials
All data generated or analyzed during this study are included in this manuscript. Data collection tool submitted with manuscript as Annexes (supplementary information files) and raw data can be accessible upon request from the authors.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (IHRERC) with a reference number of IHRERC/131/2021 and all methods were performed in accordance with Declaration of Helsinki. Written information sheet and consent, which explained the study, was provided to the medical director of HFCSH (Additional file 2). Then, officials at different levels in the hospital were communicated through formal letters. Consent from all participants and/or their legal guardian(s) was not relevant for this study because data were collected from patient’s records, not directly from patients. The information collected in this study was kept confidential through not writing the name of patient on data collection tool. Only medical record number was used for identification. Data collectors informed and trained to preserve confidentiality of the patient information and the investigators used only for the study.
Authors Contributions
Chala Deriba is principal author responsible for designing the study, data collection and analysis and interpretation of the findings. Chala Deriba, Firehiwot Amare and Jemal Abdela are responsible in the conception. Chala Deriba, Firehiwot Amare, Shambel Nigussie, Jemal Abdela, Abera Jambo and Mesay Dechasa participated in study design, analysis and interpretation of the findings. Mesay Dechasa and Abera Jambo drafted the manuscript. All authors read, revised and approved the final manuscript for submission.
Acknowledgments
Before all, we would like to acknowledge our staffs for providing constructive comments and suggestions in writing this research paper. We would also like to express our sincere thanks to Haramaya University research ethical committee for evaluating the paper. In addition, we would like to forward our gratitude to Hiwot Fana Comprehensive Specialized Hospital (HFCSH) mangers for allowing us to conduct this study in this setting and to the staff for their cooperation.
References
- Oliva F, Mortara A, Cacciatore G, et al. Acute heart failure patient profiles, management and inâhospital outcome: Results of the Italian Registry on heart failure outcome. Eur J Heart Fail. 14(11):1208-17 (2012).
[CrossRef] [Google Scholar] [PubMed]
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 74(10):1037-1147 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Atherton JJ, Sindone A, de Pasquale CG, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Guidelines for the prevention, detection, and management of heart failure in Australia 2018. Heart Lung Circ. 27(10):1123-1208 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: Developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 119(14):e391-e479 (2099).
[CrossRef] [Google Scholar] [PubMed]
- Bui AL, Horwich TB, Fonarow GC, et al. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 8(1):30-41 (2011).
[CrossRef] [Google Scholar] [PubMed]
- Abraham WT, Fonarow GC, Albert NM, et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: Insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). J Am Coll Cardiol. 52(5):347-356 (2008).
[CrossRef] [Google Scholar] [PubMed]
- Gheorghiade M, Zannad F, Sopko G, et al. Acute heart failure syndromes: Current state and framework for future research. Circulation. 112(25):3958-3968 (2005).
[CrossRef] [Google Scholar] [PubMed]
- Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: Retrospective cohort study. BMJ. 350 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Damasceno A, Mayosi BM, Sani M, et al. The causes, treatment, and outcome of acute heart failure in 1006 Africans from 9 countries: Results of the sub-Saharan Africa survey of heart failure. Arch Intern Med. 172(18):1386-1394 (2012).
[CrossRef] [Google Scholar] [PubMed]
- Meireles M, Gonçalves J, Neves J, et al. Acute heart failure comorbidome: The impact of everything else. Acta medica portuguesa. 33(2):109-115 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Kurmani S, Squire I. Acute heart failure: Definition, classification and epidemiology. Curr Heart Fail Rep. 14(5):385-392 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Kardiol Pol. 74(10):1037-1147 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Deriba C, Amare F, Abdela J, et al. In-hospital mortality and its associated factors among adult acute heart failure patients at Haramaya University hiwot fana comprehensive specialized hospital, Harar, Ethiopia.
- Farmakis D, Parissis J, Lekakis J, et al. Acute heart failure: Epidemiology, risk factors, and prevention. Rev Esp Cardiol (Engl Ed). 68(3):245-248 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Cook C, Cole G, Asaria P, et al. The annual global economic burden of heart failure. Int J Cardiol. 171(3):368-376 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Alhabib KF, Gamra H, Almahmeed W, et al. Acute myocardial infarction and acute heart failure in the Middle East and North Africa: Study design and pilot phase study results from the PEACE MENA registry. PLoS One. 15(7):e0236292 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Bukhman AK, Nsengimana VJ, Lipsitz MC, et al. Diagnosis and management of acute heart failure in sub-Saharan Africa. Curr Cardiol Rep. 21:1-8 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Carlson S, Duber HC, Achan J, et al. Capacity for diagnosis and treatment of heart failure in sub-Saharan Africa. Heart. 103(23):1874-1879 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Negesa LB, Magarey J, Rasmussen P, et al. Patients’ knowledge on cardiovascular risk factors and associated lifestyle behaviour in Ethiopia in 2018: A cross-sectional study. Plos one. 15(6):e0234198 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Tirfe M, Nedi T, Mekonnen D, et al. Treatment outcome and its predictors among patients of acute heart failure at a tertiary care hospital in Ethiopia: A prospective observational study. BMC Cardiovasc Disord. 20:1-0 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Tsega TA, Demissei BG. A systematic review of epidemiology, treatment and prognosis of heart failure in adults in Ethiopia. J Cardiovasc Med (Hagerstown). 19(3):91-97 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Filippatos G, Angermann CE, Cleland JG, et al. Global differences in characteristics, precipitants, and initial management of patients presenting with acute heart failure. JAMA cardiology. 5(4):401-410 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Chioncel O, Mebazaa A, Maggioni AP, et al. Acute heart failure congestion and perfusion status-impact of the clinical classification on inâhospital and longâterm outcomes; insights from the ESCâEORPâHFA Heart Failure LongâTerm Registry. Eur J Heart Fail. 21(11):1338-1352 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Jia Q, Wang YR, He P, et al. Prediction model of in-hospital mortality in elderly patients with acute heart failure based on retrospective study. J J Geriatr Cardiol. 14(11):669 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Asfaw E. Five years clinical characteristics and in hospital outcome of acute heart failure at tertiary care hospital in Ethiopia. Ethiop Med J. 58(01) (2020).
- Abebe SM, Andargie G, Shimeka A, et al. The prevalence of non-communicable diseases in northwest Ethiopia: Survey of Dabat health and demographic surveillance system. BMJ Open.7(10):e015496 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Bane A, Bayisa T, Adamu F, et al. Medical admissions and outcomes at Saint Paul’s Hospital, Addis Ababa, Ethiopia: A retrospective study. Ethiop J Health Dev. 30(1):50-56 (2016).
- Deriba C, Jambo A, Dechasa M, et al. In-hospital mortality and associated factors among adult patients with acute heart failure in a tertiary hospital, Harar, Eastern Ethiopia: A cross-sectional study.
- Tigabe M, Fentahun A, Getawa S, et al. Clinical characteristics and in-hospital outcome of acute heart failure patients admitted to the medical ward of University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Vasc Health Risk Manag. 16:581-590 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Storrow AB, Jenkins CA, Self WH, et al. The burden of acute heart failure on US emergency departments. JACC: Heart Failure. 2(3):269-277 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Logeart D, Isnard R, RescheâRigon M, et al. Current aspects of the spectrum of acute heart failure syndromes in a realâlife setting: The OFICA study. Eur J Heart Fail. 15(4):465-476 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Boombhi J. Clinical pattern and outcome of acute heart failure at the Yaounde Central Hospital. Open Access J. 4(03):1 (2017).
- Meijers WC, de Boer RA. Common risk factors for heart failure and cancer. Cardiovasc Res. 115(5):844-853 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Ahmed AA, Patel K, Nyaku MA, et al. Risk of heart failure and death after prolonged smoking cessation: Role of amount and duration of prior smoking. Circ Heart Fail. 8(4):694-701 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Abdellah AT, Mohamed AD, Hendawi HA, et al. Clinical and laboratory characteristics of short-term mortality in Egyptian patients with acute heart failure. Egypt Heart J. 69(3):201-208 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Deriba C, Jambo A, Dechasa M, et al. In-hospital mortality and associated factors among adult patients with acute heart failure in a tertiary hospital, Harar, Eastern Ethiopia: A cross-sectional study.
- Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: Results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ J. 47(3):341-353 (2017).
- Spinar J, Parenica J, Vitovec J, et al. Baseline characteristics and hospital mortality in the Acute Heart Failure Database (AHEAD) Main registry. Crit Care.15:1-3 (2011).
[CrossRef] [Google Scholar] [PubMed]