Case Report - Interventional Cardiology (2021)
Initial of acute stent thrombosis after stenting based on balloon angioplasty continuously
- Corresponding Author:
- Lam Truong Hoai
Department of Cardiology, Tam Anh Hospital, Hanoi, Vietnam
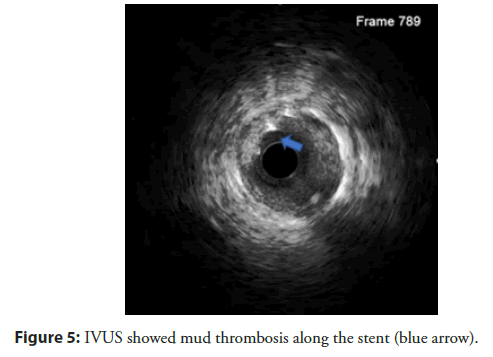
E-mail: truonglamcs@gmail.com
Received date: April 22, 2021; Accepted date: May 06, 2021l; Published date: May 13, 2021
Abstract
Acute stent thrombosis is the formation of a thrombus that obstructs the coronary lumen following stent placement. It is one of the serious complications in cardiovascular intervention with a high mortality rate. The assessment and prognosis of patients at risk of acute thrombosis after stenting plays an important role in the selection process of the intervention strategy, but careful evaluation before the intervention strategy is not avoided from acute thrombosis. Therefore, the management of acute thrombosis during the intervention plays a vital role, preventing death during the intervention. We report that a clinical case of acute stent thrombosis is successfully managed using a continuous balloon angioplasty technique to prevent thrombosis, maintain flow to perfusion myocardium, and reduce complications and mortality during acute thrombosis during the intervention.
Keywords
Thrombosis stent • Balloon angioplasty • Coronary intervention • Blood clotting
Abbreviations
LM: Left Main; LAD: Left Anterior Descending; LCx: Left Circumflex; SC: Subcutaneous; IV: Intravenous Injection.
Introduction
The immediate formation of thrombus immediately following stent placement can be caused by a variety of factors such as coagulation factors and antiplatelet, or excessive stenting expend damages the endothelium causing acute thrombosis. Many reasons are still not understood clearly. The management of acute thrombosis can be done by many methods such as thrombus aspiration device, using fibrinolysis, but the effect is still low. We report a clinical case of acute thrombosis occurring shortly after post stenting interferes with the flow. The strategy is to continuously compress the thrombosis, preventing the formation of thrombus continuing to maintain the coronary flow. Thereby preventing fatal complications during the intervention.
Case Presentation
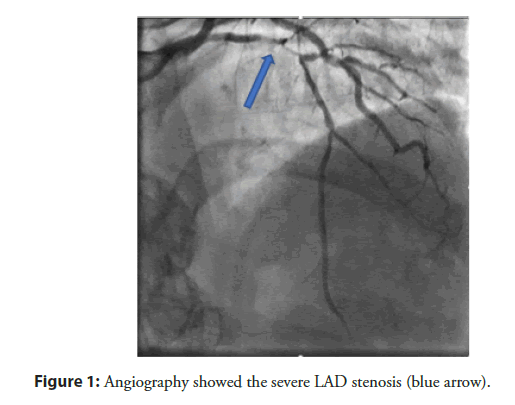
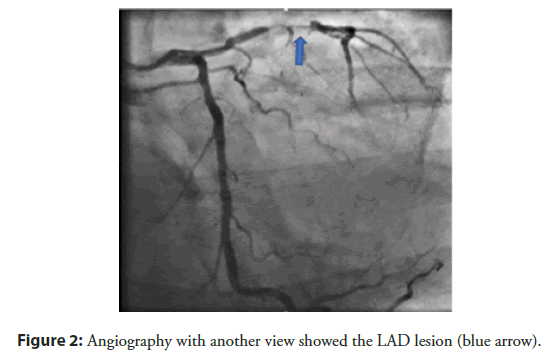
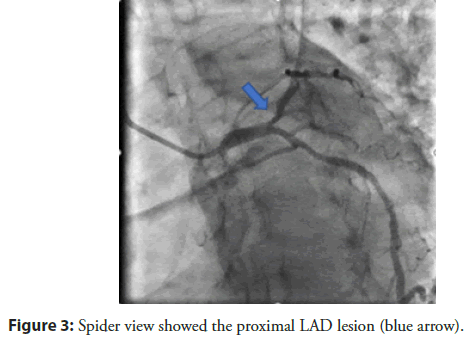
A 59-year-old male patient with a history of treatment infrequent hypertension, smoking, weighing 55 kg, hospitalized with chest pain at the 4th hour of hospitalization. The examination Blood pressure 130/80 mmHg, heart rate 80 bpm, no crackles on the lungs. ECG showed ST elevation in V2-V4 with T inverted. Medication use Lovenox 1 mg/kg SC, Lovenox 0.5 mg/kg IV, aspirin 300 mg, Ticagrelor 160 mg, Rosuvastatin 20 mg and transferred immediately Cathlab. The patient had an angiography show the lesion on proximal to mid LAD with TIMI II flow (Figures 1-3).
Figure 1: Angiography showed the severe LAD stenosis (blue arrow).
Figure 2: Angiography with another view showed the LAD lesion (blue arrow).
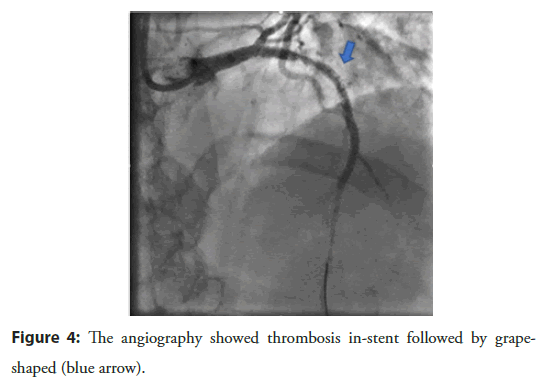
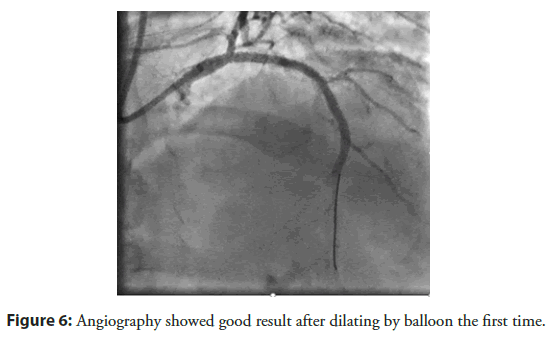
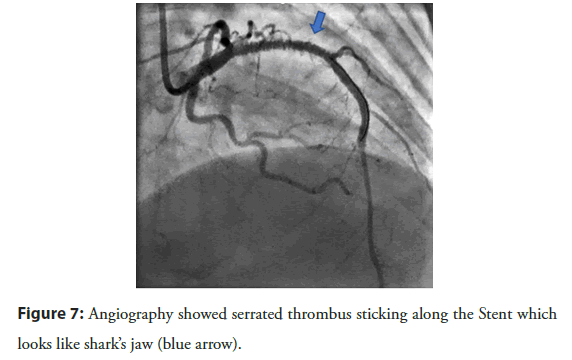
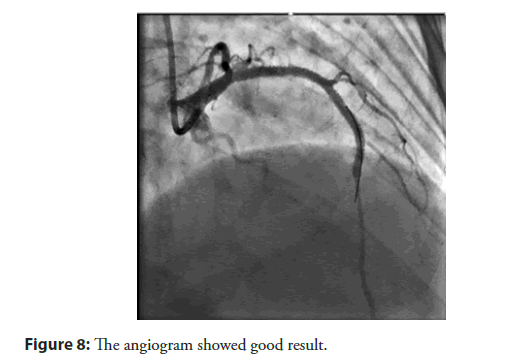
The patient had a stent placement with EBU 3.5 guiding, Wire Run through NS, predilation balloon 2.5 × 20 mm with 10 atm, DES Stent 2.75 × 24 mm (Nominal 8), and 3.0 × 26 mm (Nominal 9). After stenting, the patient had dilation with NC ballon 2.75 × 20 mm and 3.0 × 20 mm respectively. After that acute thrombus formation, large lateral branch loss, severe chest pain, sweat, hemodynamic was still stable, followed by grape-shaped thrombosis along the stent (Figure 4). Successfully opened the lateral branch due to loss with the Filder XT-A. The patient underwent an IVUS procedure to see an acute picture of an acute thrombus in a stent of a mud thrombus attached to the stent (Figure 5). This sludge thrombus formation couldn’t be used thrombus aspiration device. The interventionist decided to balloon angioplasty for the first time, the flow is clear, the smooth stent didn’t see thrombus (Figure 6). Wait 3 minutes and the angiogram showed thrombus reappear at the proximal Stent. Followed by a re-angiogram after 3 minutes of the second time, the thrombus was gradually increasing to the middle of the Stent. Angiogram the 3rd time after 3 minutes, saw the picture of serrated thrombus sticking along the stent which looks like shark’s jaw (Figure 7). When the image of serrated stent thrombus, do not hesitate to carry out an inflated balloon to break the fibrin to prevent the formation of thrombus continuing, maintaining the flow. Active balloon angioplasty every 5 minutes for the first 30 minutes, 10 minutes during the next 30 minutes. Then angiogram, the stent was clear, no thrombus formation. Angiogram after 15 minutes of good flow without stent thrombosis. Taking the third shot after 15 minutes got good results (Figure 8). After a total of 3 hours of intervention, the patient achieved good results. The patient was discharged from the hospital 2 days after the intervention with a stable condition.
Figure 4: The angiography showed thrombosis in-stent followed by grapeshaped (blue arrow).
Figure 6: Angiography showed good result after dilating by balloon the first time.
Figure 7: Angiography showed serrated thrombus sticking along the Stent which looks like shark’s jaw (blue arrow).
Figure 8: The angiogram showed good result.
Results and Discussion
Acute thrombosis during the intervention is a serious complication, which can lead to a complete blockage causing a loss of coronary flow, causing arrhythmias, hemodynamic disturbances, especially large branch sites such as ostial and proximal LAD, LCx with high mortality. The formation of acute thrombosis following stent placement can be caused by a variety of reasons, but it is not clear to understand. Some reasons are due to the patient’s coagulation factor, resistance to P2Y12 genetic, or coronary dissection after stent placement, stent structure, stent coating material, etc is one of the causes of thrombosis. Thanks to the development of the first generation drug-coated stent device, the improvement compared with the bare stent are reducing re-narrowing, but causing late thrombosis, so the second generation of the drug-coated stent with 3 coating technologies was born, reducing the rate of late thrombosis [1].
In current clinical practice, the use of dual antiplatelet agents, as well as the use of high-pressure balloons, significantly reduced the incidence of thrombosis and re-stenosis in stents by 0.7% for 1 year and 0.2%-0.6% in year 2. But the incidence is higher in patients arriving with acute coronary syndrome at 3.4% [2]. Virchow trial gives us a partial understanding of the mechanism of thrombus formation in-stent such as stent not fully expanding, the stent is smaller than lumen, diffuse long lesions. Also, endothelial damage due to dissection, or delay in-stent drug release. Besides, an attempt to steer the lateral branch wire causes an endothelial tear to the thrombus forms is also one of the top reasons. In summary, the factors that increase coagulation or increased thrombosis both contribute to the stent thrombosis situation can be congenital or acquired [3] or the injury caused during the intervention.
Essentially in coronary intervention is to maintain flow to perfusion the myocardium, preventing the blockage that causes thrombus to continue causing irreversible damage to the heart muscle leading to acute complications such as arrhythmia or later complications such as heart failure. After the vessels are open through by stent, the perfusion of the myocardium becomes better. Although many prognostic factors for acute stent thrombosis have been identified [4], but the formation of acute thrombosis after stenting is still unavoidable. This requires the experience and evaluation of the interventionist in the vital intervention process for the patient.
The use of a thrombus aspiration device in the formation of acute stent thrombosis is less effective because it is difficult to reach a sludge thrombus instead of an already clumped thrombus. Because the new thrombosis is rich in platelets, very thin, and does not clump to suck. The local thrombolysis does not have highly recommended, on the other hand, if the drug is infused through the microvascular system into the circulatory system, it is impossible to have an effective local thrombolytic effect.
The active balloon angioplasty force the thrombus to maintain the flow, if the thrombus blocks the flow, it will cause hemodynamic disorders leading to a drop in blood pressure, the slower the flow, the more blood thrombosis formation, making the patient easier more fatal, so the flow must be restrained. It is necessary to activate balloon angioplasty to prevent new thrombosis. The angioplasty needs to last up to 5 hours before the end of the internal and exogenous clotting stage [5] to break the clotting process, but maybe due to the anticoagulant and antiplatelet effects, the coagulation process no longer complies with the original standard, in this case, the clotting process stops within 2-3 hours.
Balloon size selection also plays an important role in suppressing newly formed blood clots, short repetitive balloon inflations allow better stent expansion than single prolonged inflation of the same cumulative time [6]. In the case of a balloon smaller than vascular size, the Fibrin still has a slot, the formation of blood clots continues. Using a circuit-sized balloon is the most optimal method.
Balloon size selection also plays an important role in suppressing newly formed blood clots, short repetitive balloon inflations allow better stent expansion than single prolonged inflation of the same cumulative time [6]. In the case of a balloon smaller than vascular size, the Fibrin still has a slot, the formation of blood clots continues. Using a circuit-sized balloon is the most optimal method.
Conclusion
New technique balloon angioplasty stent can be considered as a method of helping patients get off of stent thrombosis that causes loss of coronary flow with high mortality if we don’t have already of a GP IIb/IIIa inhibitor. Thanks to the active angioplasty of the thrombus to break clotting process before the thrombosis formation to fill the flow. Although successful with a few cases, this method needs more research.
References
- Ki Y-J, Park KW, Kang J, et al. Safety and efficacy of second-generation drug-eluting stents in real-world practice: Insights from the multicenter grand-DES registry. J Interv Cardiol. 2020: 3872704 (2020).
- Modi K, Soos MP, Mahajan K. Stent Thrombosis. StatPearls. (2021)
- Yahagi K, Kolodgie FD, Otsuka F, et al. Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis. Nat Rev Cardiol. 13(2): 79-98 (2016).
- Çınar T, Karabağ Y, Burak C, et al. A simple score for the prediction of stent thrombosis in patients with ST elevation myocardial infarction: TIMI risk index. J Cardiovasc Thorac Res. 11(3): 182-8 (2019).
- Yamamoto J, Inoue N, Otsui K, et al. A point-of-care global thrombosis test measuring occlusion time and endogenous lysis time may indicate thrombotic status. Future Science OA. 5(6): FSO402 (2019).
- Skowroński J, Wolny R, Jastrzębski J, et al. Impact of the balloon inflation time and pattern on the coronary stent expansion. J Interv Cardiol. 2019: 6945372 (2019).
- Oman Z, Khalid N, Boppana S, et al. Management options of acute left main coronary thrombus. Cardiovasc Revasc Med. 19(8S): 25-27 (2018).