Research Article - Interventional Cardiology (2022) Volume 14, Issue 1
Intracoronary verapamil vs. intracoronary epinephrine in the management of coronary no reflow during primary percutaneous coronary intervention
- Corresponding Author:
- Mohamed Saber Hafez
Department of Cardiology,
Ain Shams University Hospital,
Cairo,
Egypt,
E-mail: dr.mohammadsaber@yahoo.com
Received date: 29-Nov-2021, Manuscript No. FMIC-21-48552; Editor assigned: 01-Dec-2021, 2021, PreQC No. FMIC-21-48552 (PQ); Reviewed date: 17-Dec-2021, QC No. FMIC-21-48552; Revised date: 22-Dec-2021, Manuscript No. FMIC-21-48552 (R); Published date: 27-Dec-2021, DOI: 10.37532/1755-5310.2022.14(1).436
Abstract
Background: Coronary No-Reflow (CNR) is one of the common and life-threatening complications that occurs during Primary Percutaneous Coronary Intervention (PPCI) in the setting of acute ST Elevation Myocardial Infarction (STEMI). Rapid restoration of myocardial perfusion is a major challenge during this condition in order to reduce morbidity and mortality. Unfortunately, the best treatment of CNR is still unknown.
Aim: To compare between the efficacy of intracoronary verapamil and intracoronary epinephrine in the treatment of coronary no-reflow during PPCI for STEMI patients versus standard therapy (Glycoprotein IIb/IIIa inhibitors).
Methodology: This study was a prospective clinical trial in which 150 patients were included and randomly divided into three groups (verapamil, adrenaline and control-intracoronary Glycoprotein IIb/IIIA inhibitors). Immediate outcome was noted (Thrombolysis in Myocardial Infarction (TIMI) flow grade and Myocardial Blush Grade (MBG)) as well as short term outcome (Rise in Left Ventricular Ejection Fraction (LVEF) after 3 months from the index event).
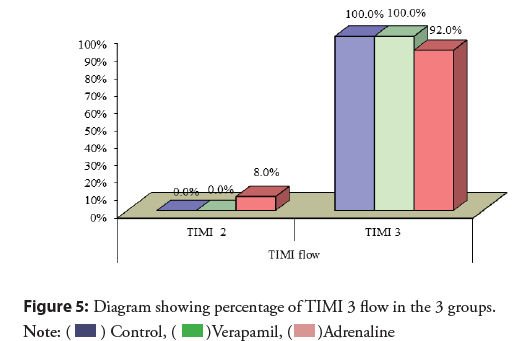
Results: Verapamil and Control groups achieved better TIMI flow (100%) than adrenaline group (92%). Intracoronary verapamil led to significantly better MBG (grade 2 or 3 in 60% of cases) compared to 38% in adrenaline group and 46% in control group and rise in LVEF was significantly higher in verapamil group (mean rise=19.6%).
Conclusion: Intracoronary verapamil injection is better than intracoronary adrenaline and intracoronary Glycoprotein II/IIIa inhibitors in the reversal of CNR during PPCI and in the improvement of LVEF at three months follow up.
Keywords
Coronary no reflow • Intracoronary verapamil • Coronary intervention
Introduction
ST segment Elevation Myocardial Infarction (STEMI) is usually caused by total thrombotic occlusion of one or more of the epicardial coronary arteries. All recent trials and guidelines point to the importance of early and successful reperfusion of the myocardium by Primary Percutaneous Coronary Intervention (PPCI) in order to reduce Major Cardiac Adverse Events (MACE) and mortality. One of the major complications that faces interventional cardiologists during PPCI is Coronary No Reflow (CNR), a situation that affects both short term and long-term results [1].
CNR is defined as reduced coronary flow and myocardial perfusion despite reperfusion therapy with Percutaneous Coronary Intervention (PCI) during acute Myocardial Infarction (MI), and is diagnosed immediately after PCI when post-procedural angiographic Thrombolysis in Myocardial Infarction risk score (TIMI) flow is <3, or if TIMI flow is 3 and Myocardial Blush Grade (MBG) is 0 or 1, or when ST resolution is <70% within 60-90 min of the procedure [2].
Coronary blood flow is evaluated using the (TIMI) flow grading system as follows; TIMI 0=no ante-grade flow beyond the point of occlusion, TIMI 1=faint ante-grade flow beyond the point of occlusion with incomplete filling of the distal vascular bed, TIMI 2=delayed or sluggish ante-grade flow with complete filling of the distal vascular beds, TIMI 3=normal flow with complete filling of the distal vascular bed [3].
MBG is defined as; MBG 0=No myocardial blush or contrast density, MBG 1=minimal myocardial blush or contrast density, MBG 2=moderate myocardial blush or contrast density but less than that obtained during angiography of a contralateral or ipsilateral non-infarct-related coronary artery, MBG 3=normal myocardial blush or contrast density, comparable with that obtained during angiography of a contralateral or ipsilateral noninfarct-related coronary artery [3].
The exact mechanism of CNR is not fully understood, thus the best treatment strategy is still unknown. The only therapy mentioned in the guidelines of STEMI management is GP IIb/IIIa inhibitors. Many other treatment strategies were proposed but did not gain solid approval, e.g. mechanical maneuvers like balloon inflation or thrombus aspiration, or pharmacological agents like intracoronary injection of adenosine, sodium nitroprusside, nitrates, verapamil and epinephrine [4].
Aim of the study
To compare between the efficacy of intracoronary verapamil and intracoronary epinephrine in the treatment of CNR during PPCI for STEMI patients versus standard therapy (Glycoprotein IIb/IIIa inhibitors).
Methodology
This study is a single center randomized controlled trial that included all STEMI patients who presented to the Emergency Room of Ain Shams University Hospital from December 2020 till September 2021 and who developed CNR during PPCI.
The study was conducted after gaining the approval of the ethical committee of faculty of medicine in Ain Shams university (FWA 000017585 MD 97/2020).
Patients were subjected to the following
Informed consent: History taking include name, age sex, race, smoking status, diabetes, hypertension, renal impairment, history of coronary artery disease, drug history, previous coronary intervention, and time to first to medical contact.
Examination: Including vital data and local examination. 12 lead ECG within 10 minutes of presentation.
Laboratory investigations: Including random blood sugar at admission, complete blood picture and kidney function tests.
All patients received a loading dose of 300 mg aspirin and 600 mg clopidogrel as well as 20 mg rosuvastatin. Upon diagnosis of STEMI, patients were transferred to the catheterization lab for PPCI performed by an expert interventional cardiologist who performed more than 75 PPCI per year [5].
Inclusion and Exclusion Criteria in our Study
Inclusion criteria
• Patients who are 18 years or older.
• Patients who fulfilled STEMI diagnosis: Symptoms consistent with myocardial ischemia in the form of persistent chest pain and ECG findings consistent with STEMI as following ST-segment elevation measured from the J point in the following settings: ≥ 2 contiguous leads with ST segment elevation ≥ 2.5 mm in men <40 years old, >2 mm in men >40 years old, or >1.5 mm in women in leads V2-V3 and/or >1 mm in all other leads [5].
• Patients who developed CNR during PPCI after stent deployment.
Exclusion criteria
• Performance of rescue PCI after thrombolysis.
• Patients who developed dissection or mechanical complication during the procedure.
• Patients with other vessel significant disease (other than the culprit vessel) or those who have more than one culprit vessel.
• Contraindications to epinephrine as hypertension with SBP>180 mmHg, known allergy to epinephrine.
• Contraindications to verapamil as hypotension with SBP<90 mmHg or cardiogenic shock and severe bradycardia or second- and third-degree heart block.
• Patient who has received both medications.
Angiography and PCI
Diagnostic coronary angiography was done viewing the anatomy of the coronary circulation. Stenosis or occlusion of the coronary arteries was then visualized, and the culprit vessel was identified. Culprit vessel in STEMI was identified angiographically by total or near total occlusion of the epicardial coronary vessel supplying the territory affected as suggested by ECG changes on presentations [6].
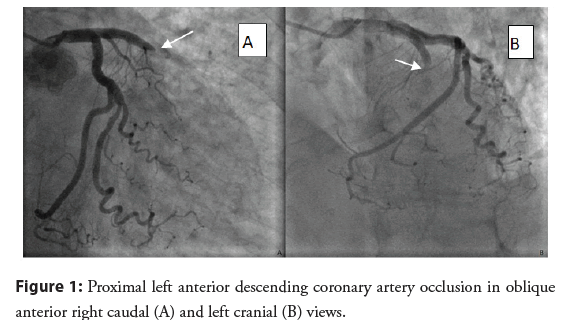
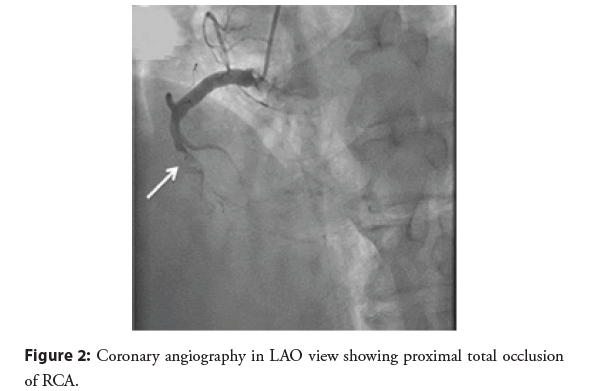
Several examples of totally occluded coronary arteries from our patients: PPCI was performed according to current guideline recommendations and operators’ routine practice. Balloon inflation was only done if distal flow was not clear after passing the PTCA wire through the culprit vessel. Mechanical thrombus aspiration was not done in any case (Figures 1 and 2). All PPCI cases were done using Drug Eluting Stents (DES), the size and positioning of the stent were determined by the operators’ decision based on case-by-case basis [7].
Figure 1: Proximal left anterior descending coronary artery occlusion in oblique anterior right caudal (A) and left cranial (B) views.
Figure 2: Coronary angiography in LAO view showing proximal total occlusion of RCA.
Tissue perfusion as an immediate outcome and one of the end points in this study was reassessed after an average latent period of 2 minutes in at least 2 projections using TIMI Flow Grade (TFG) and MBG at a frame rate of 30 per second.
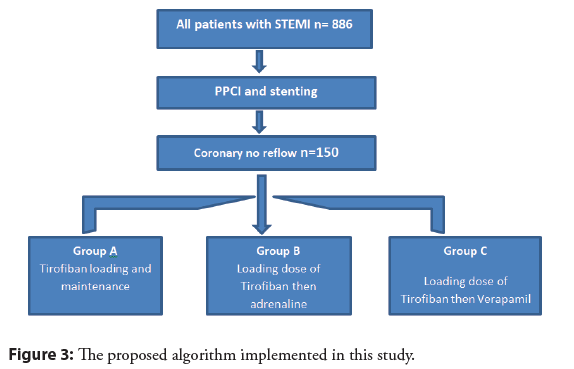
No reflow was diagnosed in patients when post-procedural angiographic TIMI flow is <3, or if TIMI flow is 3 and Myocardial Blush Grade (MBG) is 0 or 1. Patients who developed CNR (n=150) were randomly divided into 3 equal groups (n=50) using a dedicated computer software program (Research Randomizer) as follows [8]:
• Group A was the standard Control group.
• Group B was the adrenaline group.
• Group C was the verapamil group. As illustrated in Figure 3
(A) Group A represented the standard control group which was given loading dose of intracoronary tirofiban of 0.25 mg/kg slowly over 3 minutes duration and after the procedure is finished, patients were continued in the CCU on a maintenance dose of tirofiban at an infusion rate of 0.15 mg per kg per minute for 18 hours [4].
(B) Group B represented the adrenaline group which was given loading dose of tirofiban of 0.25 mg/kg slowly over 3 minutes duration and 200 micrograms of adrenaline intracoronary.
(C) Group C represented the verapamil group which was given loading dose of tirofiban of 0.25 mg/kg slowly over 3 minutes duration and 200 micrograms of verapamil intracoronary.
The Tirofiban loading dose, adrenaline and verapamil were given distal to the lesion site for better tissue accessibility. Self-made holes were created in a semi compliant balloon and then introduced distal to the lesion where the intracoronary agent was injected via the balloon into the distal capillary bed by an in-deflator [9]. After the drug was delivered, the coronary flow was re-assessed by the TIMI Flow Grade (TFG) and MBG 3 minutes later using the same projections previously used.
All patients were admitted to the coronary care unit for follow up and performed an echocardiogram for establishing a baseline Left Ventricular Ejection Fraction (LVEF). A Vivid 7 echo-machine and a 2.5 MHz matrix transducer with second harmonic imaging were used for data acquisition. Echocardiographic raw data of the apical 4, 2 and long axis view were stored in cineloop format triggered on the R-wave in the corresponding ECG, and analysis of three consecutive sinus heart beats was performed using dedicated software (EchoPAC software workstation (version BT11), GE Vingmed Ultrasound AS). 2D Eyeballing from a combination of parasternal and apical images, Simpson 2D-volumetric method based on endocardial tracing of an apical 2 and 4-chamber image were used to assess LVEF.
Patient were asked for a follow up appointment after 3 months for recanting functional capacity of the patient, repeat echo to assess LVEF, repeat hospitalization, re-infarction.
Statistical analysis
Data were collected, coded, revised, and entered the Statistical Package for Social Science (IBM SPSS) version 20. The data were presented in the form of numbers and percentages for the qualitative data, mean, standard deviations, and ranges for the quantitative data with the parametric distribution. Chi-square test was used in the comparison between three groups with qualitative data. The comparison between three groups with quantitative data and parametric distribution (tested by histogram) was done by using One-way ANOVA test.
The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the P-value was considered significant as the following:
• P>0.05: Non-Significant (NS)
• P<0.05: Significant (S)
• P<0.01: Highly significant (HS).
Results
The demographic data and cardiovascular risk factors of the studied patient population were shown in Table 1.
| N=150 | ||
| Age(years) | Mean ± SD | 56.75 ± 9.64 |
| Range | 37-85 | |
| Sex | Female | 32 (21.3%) |
| Male | 118 (78.7%) | |
| Diabetes | No | 81 (54.0%) |
| Yes | 69 (46.0%) | |
| Hypertension | No | 82 (54.7%) |
| Yes | 68 (45.3%) | |
| Previous ischemic history | No previous ischemic | 114 (76.0%) |
| Previous ischemic | 31 (20.7%) | |
| AF | 2 (1.3%) | |
| Post COVID | 1 (0.7%) | |
| No previous ischemic+post COVID | 2 (1.3%) | |
| Smoking | No | 31 (20.7%) |
| Yes | 115 (76.7%) | |
| Smoker+Cannabis | 4 (2.7%) | |
| Chest pain onset(hours) | Median (interquartile range) | 6.5 (3-12) |
| Range | 1-36 | |
Table 1: The demographic data and cardiovascular risk factors of the studied patient population.
Amongst the non-modifiable risk factors: Age and male gender were associated with higher risk of CNR, probably due to higher thrombus burden in such patients. Regarding the modifiable risk factors smoking, Diabetes and hypertension were associated with higher risk of CNR, possibly due to more extensive diseased microvascular coronary circulation. The median of chest pain onset was 6.5 hours.
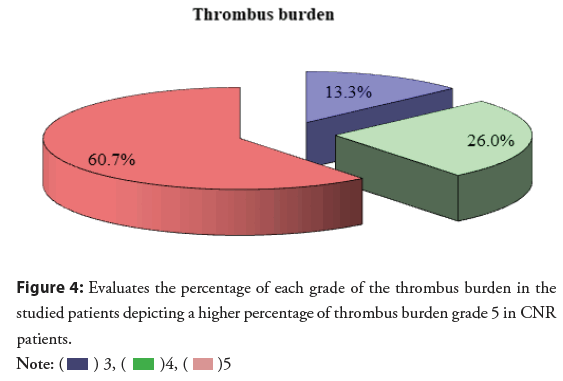
The baseline clinical, lesion, and procedural characteristics of the patients included in our study are shown in Table 2. Around two thirds (63.3%) of the patients in our study presented with anterior STEMI and more than two thirds of the patients in the study had proximal total occlusion in the culprit vessel. Almost 60% of the no reflow patients had grade 5 thrombus (Figure 4).
| N | % | ||
|---|---|---|---|
| Site | Anterior | 95 | 63.3% |
| Inferior | 36 | 24.0% | |
| Posterior | 2 | 1.3% | |
| Lateral | 4 | 2.7% | |
| Inferoposterior | 11 | 7.3% | |
| Inferolateral | 2 | 1.3% | |
| Culprit vessel | LAD | 95 | 63.3% |
| RCA | 40 | 26.7% | |
| LCX | 12 | 8.0% | |
| OM | 3 | 2.0% | |
| Level of occlusion | Proximal | 98 | 65.3% |
| Mid | 53 | 35.3% | |
| Ostial | 25 | 16.7% | |
| Distal | 7 | 4.7% | |
| Ectatic | 5 | 3.3% | |
| Aneursymal | 1 | 0.7% | |
| Stent | 1 | 88 | 58.7% |
| 2 | 59 | 39.3% | |
| 3 | 3 | 2.0% | |
| Thrombus burden | 3 | 20 | 13.3% |
| 4 | 39 | 26.0% | |
| 5 | 91 | 60.7% | |
| Intracoronary agent | Control | 50 | 33.3% |
| Verapamil | 50 | 33.3% | |
| Adrenaline | 50 | 33.3% |
Abbreviations: LAD: Left Anterior Descending; RCA: Right Coronary Artery; LCX: Left Circumflex Artery; OM: Obtuse Marginal
Table 2: The baseline clinical, lesion, and procedural characteristics of the patients included in our study.
The clinical characteristics and cardiovascular risk factors of all 3 groups were compared in Table 3. There was no statistically significant difference between all 3 groups. The chest pain duration was slightly higher in verapamil group (11 Hours) in contrast to adrenaline group (8 Hours) and control group (4 Hours) yet was statistically non-significant (P=0.25). Use of balloon dilatation before stent deployment was not significantly different between the three groups.
| Intracoronary agent | Test value | p-value | Sig. | ||||
|---|---|---|---|---|---|---|---|
| Control | Verapamil | Adrenaline | |||||
| N=50 | N=50 | N=50 | |||||
| Age | Mean ± SD | 53.38 ± 9.79 | 58.80 ± 9.99 | 58.08 ± 8.32 | 4.907 | 0.9 | Non-significant |
| Range | 38-74 | 37-85 | 43-78 | ||||
| Sex | Female | 10 (20.0%) | 10 (20.0%) | 12 (24.0%) | 0.318 | 0.853 | Non-significant |
| Male | 40 (80.0%) | 40 (80.0%) | 38 (76.0%) | ||||
| Diabetes | No | 26 (52.0%) | 31 (62.0%) | 24 (48.0%) | 2.093 | 0.351 | Non-significant |
| Yes | 24 (48.0%) | 19 (38.0%) | 26 (52.0%) | ||||
| Hypertension | No | 29 (58.0%) | 23 (46.0%) | 30 (60.0%) | 2.313 | 0.315 | Non-significant |
| Yes | 21 (42.0%) | 27 (54.0%) | 20 (40.0%) | ||||
| Previous ischemic history | No previous ischemic | 35 (70.0%) | 44 (88.0%) | 35 (70.0%) | 17.679 | 0.24 | Non-significant |
| Previous ischemic | 12 (24.0%) | 4 (8.0%) | 15 (30.0%) | ||||
| AF(atrial fibrillation) | 2 (4.0%) | 0 (0.0%) | 0 (0.0%) | ||||
| Post COVID | 1 (2.0%) | 0 (0.0%) | 0 (0.0%) | ||||
| No previous ischemic+post COVID | 0 (0.0%) | 2 (4.0%) | 0 (0.0%) | ||||
| Smoking | No | 4 (8.0%) | 9 (18.0%) | 18 (36.0%) | 20.368 | 0.1 | Non-significant |
| Yes | 46 (92.0%) | 37 (74.0%) | 32 (64.0%) | ||||
| Smoker+Hashish | 0 (0.0%) | 4 (8.0%) | 0 (0.0%) | ||||
| Chest pain onset | Median (IQR) | 4 (2-12) | 11 (4-12) | 8 (3-12) | 7.368 | 0.25 | Non-significant |
| Range | 1-24 | 2-36 | 1-24 | ||||
Table 3: The clinical characteristics and cardiovascular risk factors of all 3 groups.
The Baseline lesion and procedural characteristics of the coronary system of the patients in all three group were compared in Table 4 showing neither discernable difference nor statistical significance.
| Intracoronary agent | Test value | p-value | Sig. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control | Verapamil | Adrenaline | ||||||||
| N | % | N | % | N | % | |||||
| Site | Anterior | 31 | 62.0% | 34 | 68.0% | 30 | 60.0% | 14.228 | 0.163 | Non-significant |
| Inferior | 11 | 22.0% | 11 | 22.0% | 14 | 28.0% | ||||
| Posterior | 0 | 0.0% | 2 | 4.0% | 0 | 0.0% | ||||
| Lateral | 0 | 0.0% | 2 | 4.0% | 2 | 4.0% | ||||
| Inferoposterior | 6 | 12.0% | 1 | 2.0% | 4 | 8.0% | ||||
| Inferolateral | 2 | 4.0% | 0 | 0.0% | 0 | 0.0% | ||||
| Culprit vessel | LAD | 31 | 62.0% | 33 | 66.0% | 31 | 62.0% | 2.134 | 0.907 | Non-significant |
| RCA | 13 | 26.0% | 13 | 26.0% | 14 | 28.0% | ||||
| LCX | 4 | 8.0% | 4 | 8.0% | 4 | 8.0% | ||||
| OM | 2 | 4.0% | 0 | 0.0% | 1 | 2.0% | ||||
| Level of occlusion | Proximal | 30 | 60.0% | 38 | 76.0% | 30 | 60.0% | 3.768 | 0.152 | Non-significant |
| Mid | 23 | 46.0% | 13 | 26.0% | 17 | 34.0% | 4.435 | 0.109 | Non-significant | |
| Distal | 3 | 6.0% | 3 | 6.0% | 1 | 2.0% | 1.199 | 0.549 | Non-significant | |
| Ectatic | 4 | 8.0% | 0 | 0.0% | 1 | 2.0% | 5.379 | 0.068 | Non-significant | |
| Aneurysmal | 0 | 0.0% | 1 | 2.0% | 0 | 0.0% | 2.013 | 0.365 | Non-significant | |
Table 4: The Baseline lesion and procedural characteristics of the coronary system of the patients in all three group.
The immediate outcome depicted by the myocardial tissue perfusion assessed by TIMI flow grade and MBG were compared between the 3 groups in Table 5 showing superiority of verapamil and control group in TFG compared to the adrenaline where 100% of the control and verapamil group ended up with TIMI III flow while 92% of the adrenaline group had TIMI III flow (P=0.0106) (Figure 5).
| Intracoronary agent | Test value | p-value | Sig. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control | Verapamil | Adrenaline | ||||||||
| N | % | N | % | N | % | |||||
| Thrombolysis in Myocardial Infarction (TIMI flow) | TIMI 2 | 0 | 0.00% | 0 | 0.00% | 4 | 8.00% | 8.219 | 0.016 | Significant |
| TIMI 3 | 50 | 100.00% | 50 | 100.00% | 46 | 92.00% | ||||
| Myocardial Blush Grade | 0-1 | 27 | 54.00% | 20 | 40.00% | 31 | 62.00% | 10.047 | 0.003 | Highly significant |
| 2-3 | 23 | 46.00% | 30 | 60.00% | 19 | 38.00% | ||||
Table 5: The immediate outcomes depicted by the myocardial tissue perfusion assessed by TIMI flow grade and MBG were compared between the 3 groups.
Furthermore, 60% of the verapamil group had MBG 2 or 3 in contrast to (38% and 46%) in the adrenaline and control group respectively. So, in terms of immediate outcomes, verapamil was the most successful agent in the reversal of CNR.
The short term outcomes depicted by the improvement of LVEF after 3 months follow up period was compared between the 3 groups in Table 6 showing a better improvement in the LV functions with verapamil in comparison to the control and adrenaline groups (P=0.021). Some of the cases in the verapamil group had up to 30% rise in the EF after 3 months follow up.
| Intracoronary agent | Test value | p-value | Sig. | ||||
|---|---|---|---|---|---|---|---|
| Control | Verapamil | Adrenaline | |||||
| N=50 | N=50 | N=50 | |||||
| Index EF | Mean ± SD | 36.30 ± 8.19 | 35.70 ± 8.63 | 36.46 ± 8.76 | 0.11 | 0.896 | Non-significant |
| Range | 20-60 | 20-50 | 24-55 | ||||
| Follow up EF | Mean ± SD | 40.00 ± 9.85 | 41.70 ± 9.88 | 39.40 ±9.18 | 0.766 | 0.467 | Non-significant |
| Range | 20-60 | 25-60 | 25-55 | ||||
| % Of change | Mean ± SD | 10.11 ± 10.73 | 19.60 ± 29.47 | 9.18 ± 16.57 | 3.963 | 0.021 | Significant |
| Range | 0-33.33 | -11.11-125 | -14.29-66.67 | ||||
Table 6: The short term outcomes depicted by the improvement of LVEF after 3 months follow up period was compared between the 3 groups.
Discussion
The main goal of this study was to compare between the benefits obtained from intracoronary adrenaline and verapamil compared to standard control group in reversal of CNR during PPCI in the setting of acute STEMI. The study results showed that verapamil led to better MBG, TFG and higher rise in EF after 3 months as compared to adrenaline and control groups.
To the best of our knowledge, this head-to-head comparison between the two drugs was not previously performed. Yet, many prior studies have separately evaluated the efficacy of both the verapamil and adrenaline in the setting of no reflow during PPCI and have supported their use.
A recently published trial tackled the use of both drugs in the prevention of CNR using distal intracoronary drug delivery. No reflow was lower with epinephrine than verapamil (25% vs. 27.5%); however, with no statistically significant difference [10]. In our study, drug delivery was done to reverse CNR after its actual occurrence, a fact that might explain why we found verapamil superior than adrenaline.
In a previous meta-analysis study that evaluated short-term effect of verapamil on coronary no-reflow associated with percutaneous coronary intervention in patients with acute coronary syndrome, verapamil proved to be effective in decreasing the incidence of CNR, improving TFG, reducing the 30-day Wall Motion Index (WMI) and reducing MACE. However, administration of verapamil did not provide an additional improvement of left ventricular ejection fraction regardless of the time that had passed post-PCI [11]. In our study, verapamil led to a significant improvement in LVEF, 3 months after STEMI. This difference might be explained by the fact that they used Cardiac MRI to depict changes in ejection fraction, while echocardiography was used in this study.
In another study, verapamil had a success rate of 84% in reversal of CNR in patients with STEMI during PPCI [12].
Regarding adrenaline, a mean of 333 mcg of intracoronary epinephrine successfully reversed MBG in 75% of patients during PPCI [13]. However, in their study larger repeated dosing of the drug was used in the patient until reversal of no reflow, a fact that may explain why adrenaline was not that effective in our study (only 68% had MBG 2-3 in the adrenaline group).
In another study, thirty consecutive patients with severe refractory coronary no-reflow (TIMI 0-1, MBG 0-1) during PPCI were prospectively included after initial failure of conventional treatments, e.g. intracoronary Glycoprotein IIB/IIA inhibitors, nitrates and thrombectomy. Intracoronary administration of epinephrine yielded significantly better coronary flow compared to control and there was a significant reduction of 30-day composite of death or heart failure, improvement of ejection fraction and STsegment resolution [14].
Change and improvement in LV functions as one of the end points of the study was compared among all three groups showing significant improvement among the verapamil group (10.11% in the control group, 19.6% in the verapamil group and 9.18% in the adrenaline group with P=0.021). These results coincide with the previous studies in that both drugs reverse CNR and cause an improvement in LVEF during follow up [15,16].
Conclusion
Finally, it should be noted that the study showed no demonstrable benefit of adrenaline in both immediate and short term outcomes as compared to the control. We postulate that the cause of worse outcome in the adrenaline group was due to the fact that this drug increases platelet aggregation, causes ventricular arrythmias, increases left ventricular end diastolic pressure and has direct toxic effect on the myocardium.
In the case of CNR during PPCI, administration of intracoronary verapamil was more effective than adrenaline and Gp IIb/IIIa inhibitors in terms of both immediate outcome (reversal of CNR and better MBG) and short term outcome (higher rise in LVEF).
Limitations
The study was a single center study with limited number of patients. Many effective drugs were not included in the comparison, e.g. adenosine. The follow up period was short.
References
- Tasar O, Karabay AK, Oduncu V, et al. Predictors and outcomes of no-reflow phenomenon in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 30(4): 270-276 (2019).
[CrossRef] [Google scholar] [Pubmed]
- Rezkalla SH, Stankowski RV, Hanna J, et al. Management of no-reflow phenomenon in the catheterization laboratory. JACC Cardiovasc Interv. 10(3): 215-23 (2017).
[CrossRef] [Google scholar] [Pubmed]
- Henriques JP, Zijlstra F, van't Hof AW, et al. Angiographic assessment of reperfusion in acute myocardial infarction by myocardial blush grade. Circulation. 107(16): 2115-9 (2003).
[CrossRef] [Google scholar] [Pubmed]
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 39(2): 119-177 (2018).
[CrossRef] [Google scholar] (All versions) [Pubmed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Writing group on the joint ESC/ACCF/AHA/WHF task force for the universal definition of myocardial infarction, ESC committee for practice guidelines: Third universal definition of myocardial infarction. Eur Heart J. 33(20): 2551-67 (2012).
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 127: 362-425 (2013).
[CrossRef] [Google scholar] (All versions) [Pubmed]
- Nordmann AJ, Hengstler P, Harr T, et al. Clinical outcomes of primary stenting versus balloon angioplasty in patients with myocardial infarction: A meta-analysis of randomized controlled trials. Am J Med. 116(4): 253-262 (2004).
[CrossRef] [Google scholar] [Pubmed]
- Urbaniak GC, Plous S. Research randomizer (version 4.0) (Computer Software) (2013).
- Arab TA, Rafik R, Adel El Etriby. Efficacy and safety of local intracoronary drug delivery in treatment of no-reflow phenomenon: A pilot study. J Interv Cardiol. 29(5): 496-504 (2016).
[CrossRef] [Google scholar] [Pubmed]
- Yassin I, Ahmed A, Abdelhady G. Distal intracoronary delivery of epinephrine versus verapamil to prevent no-reflow during primary percutaneous coronary intervention: A randomized, open-label, trial. Cardiol Vasc Res. 5(5): 1-6 (2021).
- Su Q, Li L, Naing KA, et al. Safety and effectiveness of nitroprusside in preventing no-reflow during percutaneous coronary intervention: A systematic review. Cell Biochem Biophys. 68(1): 201-6 (2014).
[CrossRef] [Google scholar] [Pubmed]
- Fu Q, Lu W, Huang YJ, et al. Verapamil reverses myocardial no-reflow after primary percutaneous coronary intervention in patients with acute myocardial infarction. Cell Biochem Biophys. 67(3): 911-4 (2013).
[CrossRef] [Google scholar] [Pubmed]
- Aksu T, Guler TE, Colak A, et al. Intracoronary epinephrine in the treatment of refractory no-reflow after primary percutaneous coronary intervention: A retrospective study. BMC cardiovascular disorders. 15(1): 1-7 (2015).
[CrossRef] [Google scholar] [Pubmed]
- Navarese EP, Frediani L, Kandzari DE, et al. Efficacy and safety of intracoronary epinephrine versus conventional treatments alone in STEMI patients with refractory coronary no-reflow during primary PCI: The RESTORE observational study. Catheter Cardiovasc Interv. 97(4): 602-11 (2021).
[CrossRef] [Google scholar] [Pubmed]
- Dragula M, Ságová I, KÅazeje M, et al. Use of intracoronary epinephrine in a patient with noflow phenomenon in cardiogenic shock-case report. Cor et Vasa. 62(5): 457-460 (2020).
- Das R, Pluskota E, Plow EF. Plasminogen and its receptors as regulators of cardiovascular inflammatory responses. Trends Cardiovasc Med. 20(4): 120-4 (2010).
[CrossRef] [Google scholar] [Pubmed]