Case Report - Interventional Cardiology (2022) Volume 14, Issue 4
Intravascular lithotripsy as a rescue option in the treatment of stent underexpansion: A case report
- Corresponding Author:
- Grzegorz Sobieszek
Department of Cardiology,
1st Military Clinical Hospital,
Lublin,
Poland,
E-mail: marknguyen.dr@gmail.com
Received date: 07-Jun-2022, Manuscript No. FMIC-22-66083; Editor assigned: 09-Jun-2022, PreQC No. FMIC-22-66083 (PQ); Reviewed date: 27-Jun-2022, QC No. FMIC-22-66083; Revised date: 04-Jul-2022, Manuscript No. FMIC-22-66083 (R); Published date: 11-Jul-2022, DOI: 10.37532/1755- 5310.2022.14(4).537
Abstract
The treatment of calcified atherosclerotic lesions in the coronary arteries is one of the greatest challenges of contemporary invasive cardiology. Insufficient preparation of the lesion before stent implantation may cause complications. The introduction of new tools, such as intravascular lithotripsy, is a valuable method of treatment not only at the stage of atherosclerotic plaque preparation, but also a rescue option in the case of non-expansion of a stent implanted in a calcified, suboptimally prepared lesion. This paper presents the cases of two patients treated with intravascular lithotripsy in the Department of Cardiology of the 1st Military Clinical Hospital in Lublin. In both cases, the reason for the intervention was insufficient expansion of previously implanted stents. Thanks to the use of ultrasound wave energy, it was possible to treat this complication, which was confirmed in endovascular imaging studies. In view of the effectiveness and widespread use of lithotripsy in such situations, the need to extend the indications for the use of this valuable tool seems obvious.
Keywords
lithotripsy • Stent underexpansion • Percutaneous coronary intervention
Abbreviations
PCI: Percutaneous Coronary Intervention; NC: Non-Compliant; OCT: Optical Coherence Tomography; IVL: Intravascular Lithotripsy; LM: Left Main; LAD: Left Descending Artery; Cx: Circumflex artery; LVEF: Left Ventricular Ejection Fraction; NSTEMI: Non-ST-Elevation Myocardial Infarction; MLA: Minimal Lumen Area; DES: Drug-Eluting Stent; DEB: Drug-Eluting Balloon; IVUS: Intravascular Ultrasound; atm.: atmosphere
Introduction
The treatment of highly calcified atherosclerotic lesions in the coronary arteries has been one of the greatest challenges of contemporary interventional cardiology for many years. It is estimated that severe calcification affects up to 20% of patients undergoing Percutaneous Coronary Interventions (PCI). Patients with this type of atherosclerotic lesions are a group at increased risk of adverse cardiovascular events, and are also characterized by a worse prognosis. A higher frequency of complications of percutaneous coronary interventions performed on lesions of this type is also known [1-6].
The success of percutaneous coronary interventions within highly calcified lesions requires diligence and due care from even the most experienced operator. Thorough lesion preparation prior to stent implantation is a prerequisite for success. The use of endovascular imaging methods, especially Optical Coherence Tomography (OCT), can provide information about the morphology of the atherosclerotic plaque, which will facilitate the planning of the procedure, and thus increase the patient’s safety and avoid complications [7-9].
Over the years, many solutions have been introduced into common use, the mutual goal of which is to optimize the treatment outcomes of calcified atherosclerotic lesions. Apart from aggressive dilation with the use of high pressure Non-Compliant (NC) balloons, cutting and scoring balloons, rotational atherectomy (rotablation) is a well-known and available method for many years. Relatively new tools are orbital atherectomy, laser atherectomy and Intravascular Lithotripsy (IVL). The latter method is highly hoped for in particular due to its favorable safety profile. A combination of several therapeutic options brings good results [10-14].
In this paper, we present the cases of two patients treated with intravascular lithotripsy in the Department of Cardiology of the 1st Military Clinical Hospital in Lublin due to underexpanded stents in the coronary vessels. Both patients are sent to the ward from centers without access to this.
Case Presentation
An 84-year-old patient after coronary interventions in the right coronary artery and bifurcation of the left main with DES implantation as part of NSTEMI treatment was admitted to the Cardiology Department of the 1st Military Clinical Hospital in Lublin in order to optimize the effect of LM/LAD/Cx angioplasty done 8 days earlier. In addition, a transthoracic echocardiography performed on admission revealed left ventricular systolic dysfunction (LVEF 30%) and segmental contractility disorders in the form of inferior and posterior wall akinesia and hypokinesia of the remaining walls. In laboratory tests, attention was drawn to increased level of troponin and NT pro-BNP. After proper preparation, the patient was qualified for invasive treatment.
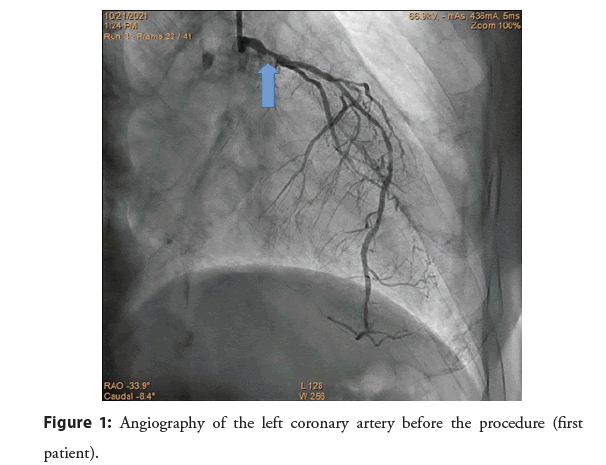
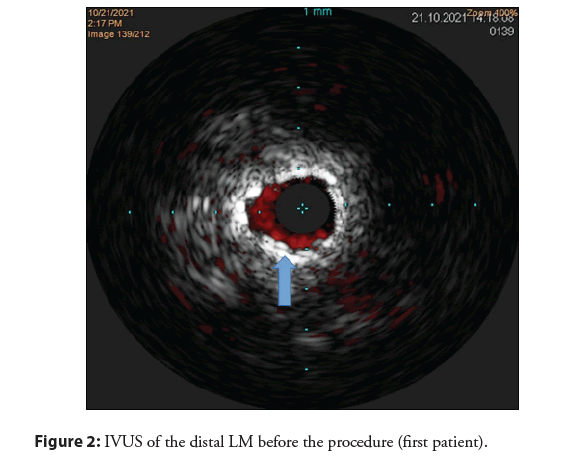
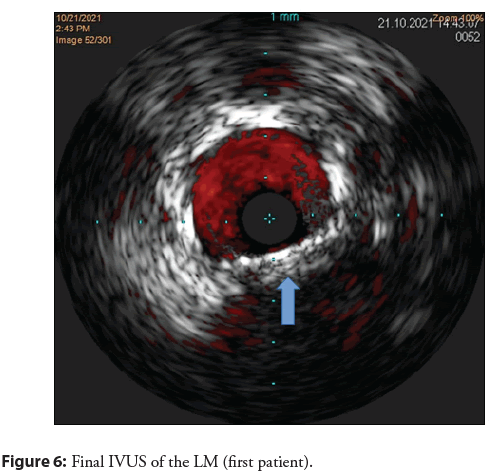
The projection of the left coronary artery revealed the presence of a significantly under–expended stent in the distal segment of the LM and significant stenosis in the middle segment of the anterior descending branch, as well as chronic total occlusion of the circumflex (Figure 1). In order to optimally plan the procedure, imaging with Intravascular Ultrasound (IVUS) was used (Figure 2). The MLA of the distal LM was estimated to be 2.7 mm² within the implanted DES. A decision was made to perform immediate vessel angioplasty.
Figure 1: Angiography of the left coronary artery before the procedure (first patient).
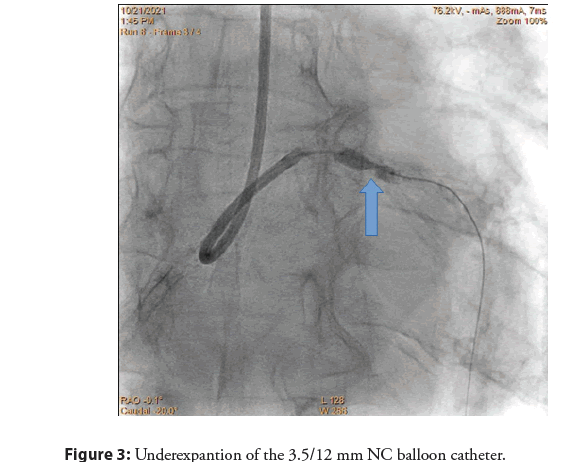
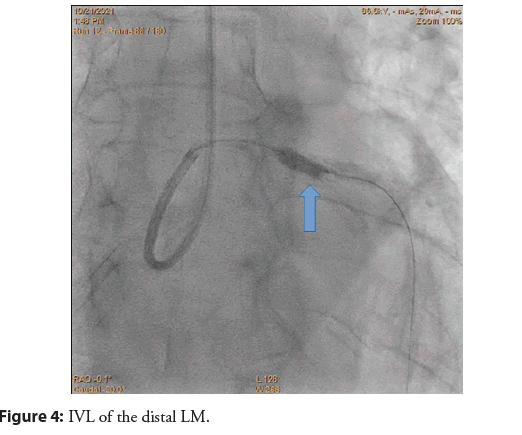
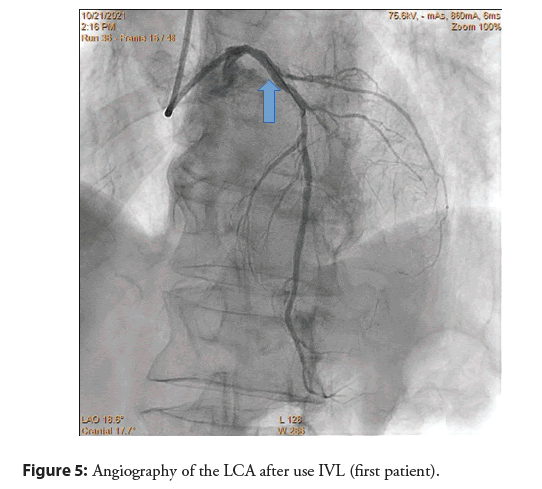
In the first stage of the procedure, a 3.5/12 mm NC balloon catheter was used (Figure 3). Despite the use of high pressures (20 atm.), the optimal expansion of the balloon was not achieved. Angioplasty with endovascular lithotripsy was performed (Figure 4). After using 80 pulses (8 cycles of 10 pulses), the optimal expansion of the IVL balloon 4.0/12 mm was found. At a later stage of the procedure, an effective angioplasty of the middle segment of the LAD was performed with the implantation of a 3.0/38 mm DES. The final projections showed a good angiographic effect (Figure 5). In the postoperative IVUS control, the MLA of the distal LM was estimated at 9.8 mm2 (Figure 6).
Figure 5: Angiography of the LCA after use IVL (first patient).
The patient was discharged in good general condition on the fifth day of hospitalization. Pharmacological treatment included dual antiplatelet therapy with clopidogrel, as well as perindopril, rosuvastatin, eplerenone, torasemide, empagliflozin and pantoprazole. Due to bradycardia, treatment with the beta-blocker was discontinued. Echocardiographic control was recommended to qualify for cardioverter-defibrillator implantation.
The second patient treated in a similar manner in the Cardiology Department of the 1st Military Hospital was a 71-year-old patient after many coronary interventions in the past, with an underextended stent in the middle part of the left anterior descending coronary artery implanted 4 days earlier. Transthoracic echocardiography revealed left ventricular systolic dysfunction (LVEF 45%). In laboratory tests, elevated levels of troponins have been noted. The patient was qualified for invasive treatment.
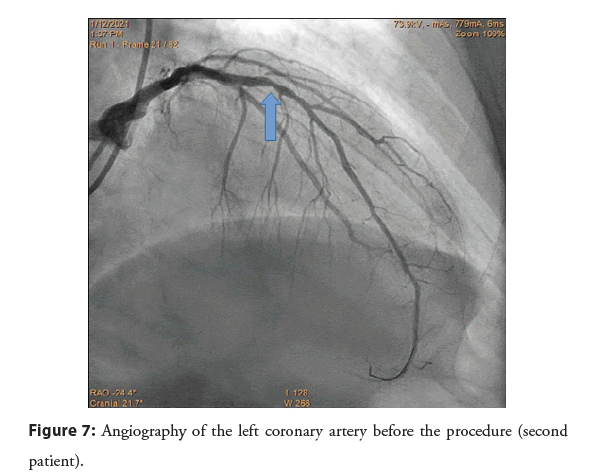
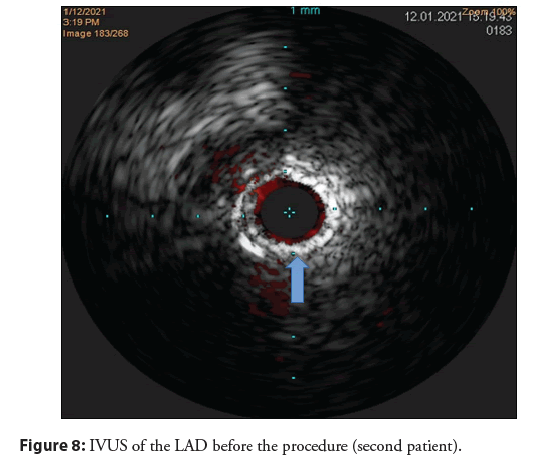
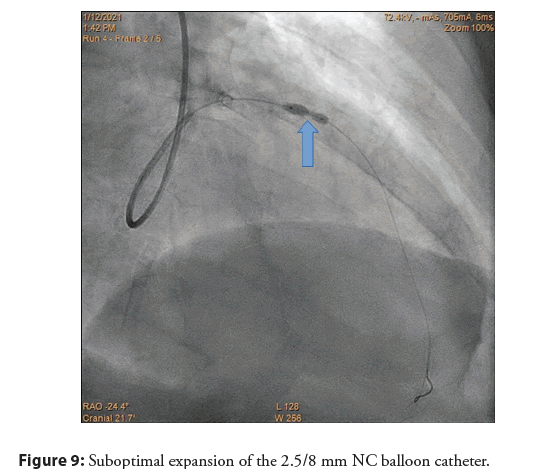
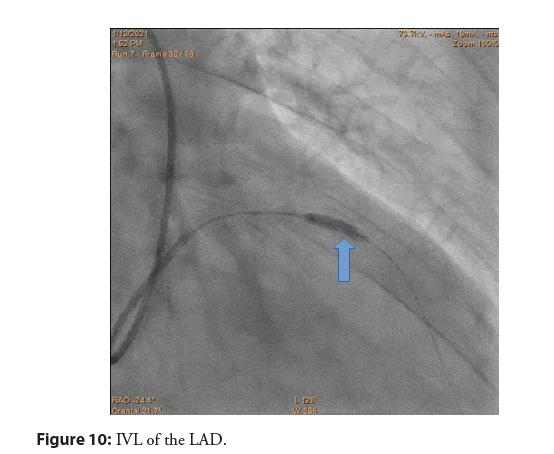
The projections of the left coronary artery showed a significant stenosis in the anterior descending branch in an underexpanded stent (Figure 7). No significant atherosclerotic changes were found in the remaining vessels. As in the first case, intravascular ultrasound was used. Within the lesion, the MLA of the vessel was 2.0 mm² (Figure 8). A decision was made to implement PCI. Due to the suboptimal expansion of the 2.5/8 mm NC balloon catheter within the lesion (Figure 9) and the scoring balloon, a decision was made to use lithotripsy (Figure 10). The result was in a good expansion of the 3.0/12 mm balloon.
Figure 7: Angiography of the left coronary artery before the procedure (second patient).
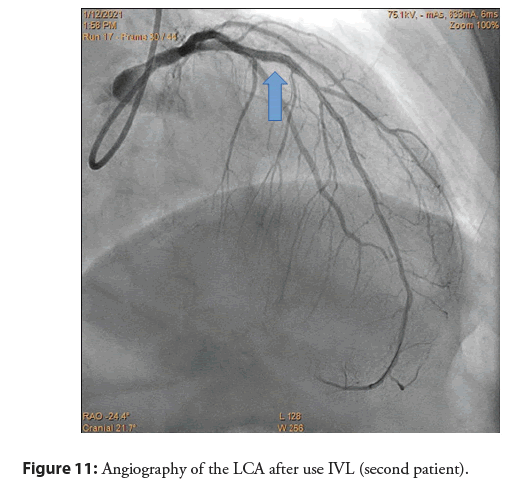
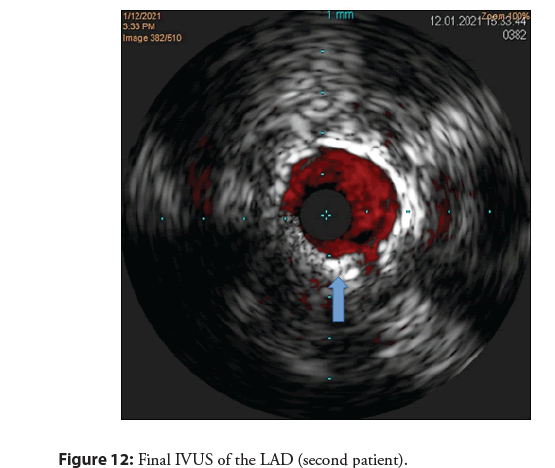
A good angiographic effect (Figure 11) and MLA of the 5.5 mm2 vessel in IVUS were achieved with the use of a drug eluting balloon (DEB) (Figure 12).
Figure 11: Angiography of the LCA after use IVL (second patient).
The patient was discharged from the ward on the third day of hospitalization in good general condition with the recommendation of standard pharmacotherapy.
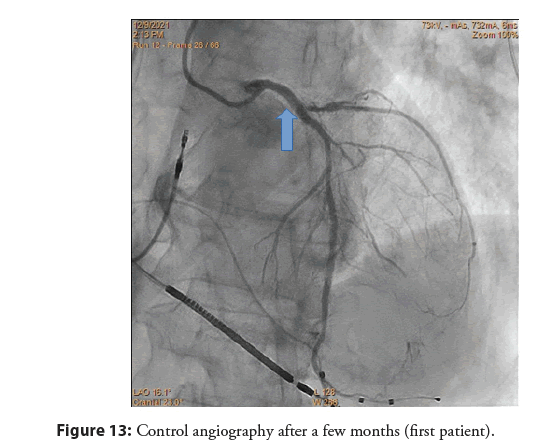
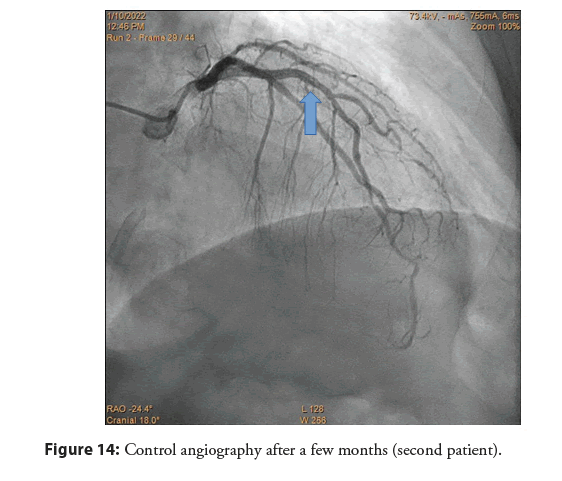
After a few months, control angiography was performed in both patients, confirming the good effect of the procedure in patient no. 1 (Figure 13) and in patient no. 2 (Figure 14).
Figure 13: Control angiography after a few months (first patient).
Figure 14: Control angiography after a few months (second patient).
Results and Discussion
Despite the wide range of available tools, there are still cases of stent implantation in insufficiently prepared atherosclerotic lesions. The obvious consequence of such a procedure is insufficient stent expansion, which is associated with an increased rate of complications. In most cases, the lack of effective treatment methods entails the necessity to perform additional, even more aggressive dilatation, which increases the risk of complications. The use of intravascular lithotripsy in such cases seems to be beneficial due to the effectiveness of the method and a favorable safety profile. IVL is a method based on the use of ultrasonic waves, the pulses of which lead to the generation of a shock wave that crushes limestone deposits, thus modifying the atherosclerotic plaque. Despite the fact that the use of IVL in this type of cases, as well as in the treatment of in-stent restenosis, is an off-label indication, the effectiveness of the method means that it is also widely used in such situations, bringing good results, which is also indicated by the published records and case reports [15-21].
Conclusion
Treatment of severely calcified lesions in the coronary arteries continues to be a challenge even for the most experienced hemodynamics. The key aspect is the appropriate planning of the procedure and preparation of the lesion before possible stenting. Despite the wide range of tools available, there are cases of hasty decisions about stent implantation. In such cases, endovascular lithotripsy may be a good therapeutic option, which in many situations turns out to be the only rescue option. It seems necessary to develop more extensive research on this topic.
References
- Vliegenthart R, Oudkerk M, Hofman A, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 112(4): 572-7 (2005).
[CrossRef] [Google Scholar] [PubMed]
- Liu W, Zhang Y, Yu C-M, et al. Current understanding of coronary artery calcification. J Geriatr Cardiol. 12(6): 668-75 (2015).
[Google Scholar] [PubMed]
- Leopold JA. Vascular calcification: Mechanisms of vascular smooth muscle cell calcification. Trends Cardiovasc Med. 25(4): 267-74 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 358: 1336-45 (2008).
[CrossRef] [Google Scholar] [PubMed]
- Bourantas CV, Zhang Y-J, Garg S, et al. Prognostic implications of coronary calcification in patients with obstructive coronary artery disease treated by percutaneous coronary intervention: A patient-level pooled analysis of 7 contemporary stent trials. Heart. 100: 1158-64 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Généreux P, Madhavan MV, Mintz GS, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. J Am Coll Cardiol. 63(18): 1845-54 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Fujino A, Mintz G, Matsumura M, et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention. 13(18): e2182-9 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Räber L, Mintz GS, Koskinas KC, et al. Clinical use of intracoronary imaging. Part 1: Guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 39(35): 3281-300 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Alawami M, Thirunavukarasu S, Ahmed J. Intravascular lithotripsy to treat an underexpanded coronary stent: 4‐Month angiographic and OCT follow‐up. Catheter Cardiovasc Interv. 96(6): 1251-1257 (2020).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Cortese B. The role of optimal lesion preparation for de-novo coronary vessels when a stentless intervention strategy is planned. Minerva Cardioangiologica. 68(1): 51-6 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Akin I, Pohlmann S, Nienaber CA, et al. A different way of coronary lesion preparation: Stentablation and rotastenting. Clin Med Insights Cardiol. 6: 53-6 (2012).
[CrossRef] [Google Scholar] [PubMed]
- Abdel-Wahab M, Toelg R, Byrne RA, et al. High-speed rotational atherectomy vs. modified balloons prior to drug-eluting stent implantation in severely calcified coronary lesions. Circ Cardiovasc Interv. 11(10): e007415 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Hemetsberger R, Toelg R, Mankerious N, et al. Impact of calcified lesion complexity on the success of percutaneous coronary intervention with upfront high-speed rotational atherectomy or modified balloons–A subgroup-analysis from the randomized PREPARE-CALC trial. Cardiovasc Revasc Med. 33: 26-31 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Bujak M, Wanha W. Intravascular lithotripsy: A novel method for revascularization of severely calcified coronary stenoses. Medycyna po Dyplomie. 6: 14-20. (2021).
- Hill JM, Kereiakes DJ, Shlofmitz RA, et al. Intravascular lithotripsy for treatment of severely calcified coronary artery disease. J Am Coll Cardiol. 76(22): 2635-46 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Ali ZA, Brinton TJ, Hill JM, et al. Optical coherence tomography characterization of coronary lithoplasty for treatment of calcified lesions. JACC Cardiovasc Imaging. 10(8): 897-906 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Górny B, Balak W, Bielawski G. Underexpanded stent in left anterior descending coronary artery treated with intravascular lithotripsy. Postepy Kardiol Interwencyjnej. 16(2): 216‐218 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Arroyo-Úcara E, Vazquiáneza MR, Sauraa FT. Coronary intravascular lithotripsy and severe stent underexpansion. Rev Port Cardiol. 38(12): 899-901 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Yeoh J, Cottens D, Cosgrove C, et al. Management of stent underexpansion using intravascular lithotripsy-Defining the utility of a novel device. Catheter Cardiovasc Interv. 97(1): 22-29 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Ali ZA, McEntegart M, Hill JM, et al. Intravascular lithotripsy for treatment of stent underexpansion secondary to severe coronary calcification. Eur Heart J. 41(3): 485-486 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Nagaraja V, Ubaid S, Khoo C, et al. Intravascular lithotripsy for stent underexpansion despite utilization of rotational atherectomy for plaque modification. Cardiovasc Revasc Med. 21(11S): 147-148 (2020).
[CrossRef] [Google Scholar] [PubMed]