Mini Review - Interventional Cardiology (2022)
Larger or smaller, which size of balloon expandable transcatheter aortic valve is better for border zone aortic annulus?
- Corresponding Author:
- Tomohiro Kawaguchi
Department of Cardiology,
Kagawa Prefectural Central Hospital,
1-2-1 Asahi-cho,
Takamatsu,
Kagawa,
Japan,
E-mail: tomokawa9313@gmail.com
Received date: 25-Jul-2022, Manuscript No. FMIC-22-70148; Editor assigned: 27-Jun-2022, PreQC No. FMIC-22-70148 (PQ); Reviewed date: 15-Aug-2022, QC No. FMIC-22-70148;Revised date: 22-Aug-2022, Manuscript No. FMIC-22-70148 (R);Published date: 29-Aug-2022, DOI: 10.37532/1755-5310.2022.14(S11). 263
Abstract
Transcatheter Aortic Valve Implantation (TAVI) is an established treatment for Aortic Stenosis (AS). In the balloon expandable aortic valve, SAPIEN 3, valve size is selected based on the size chart published by the manufacturer. However, in patients with border zone annulus, the valve sizing is chosen at the discretion of the clinicians, which is controversial. Larger Transcatheter Heart Valves (THV) with underfilling have been found to contribute to larger effective orifice area, and both larger THV sizing and smaller THV sizing with overfilling have been found to reduce the transvalvular mean pressure gradient. Larger THV sizing with underfilling might reduce aortic regurgitation compared with small THV sizing with overfilling. With larger THV sizing, coronary impairment can occur considering redo TAVI if the THV commissure level is located above the sino-tubular junction level. Smaller THVs should be considered for patients with the possibility of a redo TAVI procedure if coronary obstruction can be avoided. When a larger THV is selected for border zone cases, implantation with underfilling is safe and feasible for avoiding annular rupture. In TAVI with SAPIEN 3 for border zone cases, valve size selection should be made according to each patient’s background and anatomical features. Considering lifetime management of patients with AS, careful and ‘tailor-made’ TAVI strategies could be essential to ensuring the best treatment option in border zone cases.
Keywords
Transcatheter aortic valve implantation • Balloon expandable valve • Border zone annulus • Underfilling • Overfilling
Abbreviations
AS: Aortic Stenosis; AR: Aortic Regurgitation; EOA: Effective Orifice Area; LVOT: Left Ventricular Outflow Tract; MDCT: Multi-Detector Computed Tomography; PPI: Permanent Pacemaker Implantation; PPM: Patient Prosthesis Mismatch; PVL: Paravalvular Leakage; SAVR: Surgical Aortic Valve Replacement; STJ: Sino-Tubular Junction; TAVI: Transcatheter Aortic Valve Implantation; THV: Transcatheter Heart Valve
Introduction
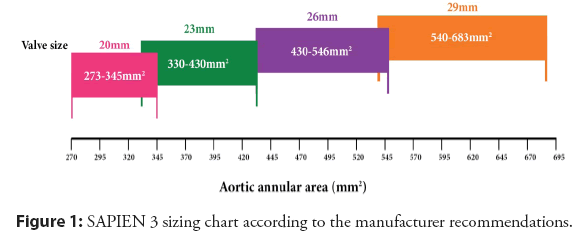
Transcatheter Aortic Valve Implantation (TAVI) is an established treatment option for Aortic Stenosis (AS) [1,2]. In the balloon-expandable transcatheter aortic valve, SAPIEN 3 (Edwards Life Sciences, Irvine, CA, USA), the valve size recommended by the manufacturer is based on the echocardiographic measurement or the annular area measured by Multi-Detector Computed Tomography (MDCT), the latter is generally utilized (Figure 1). However, in patients with border zone annulus, the valve size is selected at the discretion of the operators in clinical practice. The definition of the border zone is not confirmed; different studies have various definitions (Table 1) [3-6].
In border zone cases, there is a dilemma because annular rupture can occur with oversized Transcatheter Heart Valves (THVs), and suboptimal THV performance and residual Paravalvular Leakage (PVL) can occur with undersized THV. In this review article, we describe how oversized and undersized balloon-expandable THV have clinical impacts on border zone cases.
Literature Review
THV performance and prosthesis-patient mismatch in the border zone
In borderline cases, larger valve selection has been reported to improve several aspects related to better THV performance. We reported that Effective Orifice Area (EOA) measured by echocardiography was significantly greater in all border zones with larger valve sizing; the majority of THV were implanted with underfilling, and there was no significant increase in the rates of Permanent Pacemaker Implantation (PPI), disabling stroke, or annular rupture [3]. Talmor, et al. reported that larger valve sizing contributed to significantly lower post-procedural transvalvular 264mean pressure gradients than smaller THV, without increasing serious complications [4]. The data of PARTNER 3 (Placement of Aortic Transcatheter Valves 3) showed that in selected patients with annular dimensions in between 2 valve sizes, the larger THV device oversized to both the annular area and perimeter optimized THV hemodynamics [7]. On the other hand, Patsalis, et al. reported that a smaller THV with overfilling implantation, which the 23-, 26-, and 29-mm SAPIEN 3 were over-expanded by overfilling inflation with 2 ml, 3 ml, and 4 ml additional volume, improved the mean pressure gradient and reduced the incidence of annular rupture in border zones [5]. In Surgical Aortic Valve Replacement (SAVR), EOA is an important marker for prognosis, and severe Patient Prosthesis Mismatch (PPM) is a confirmed negative predictor for long-term prognosis [8-12]. A large-scale meta-analysis including 27,186 patients revealed negative impacts of severe and moderate PPM on all-cause and cardiac-related mortality over 5 years [12]. However, in TAVI, the impact of PPM on mortality is still a matter of debate. According to the STS (The Society of Thoracic Surgeons)/American College of Cardiology TVT (Transcatheter Valve Therapy) registry, severe PPM after TAVI was present in 12% of patients and was associated with significantly higher mortality and heart failure rehospitalization than moderate PPM and no PPM at 1-year follow-up [13]. In the OCEAN-TAVI registry, which included 1,546 Japanese patients, severe PPM was observed in 0.7% of patients and was not associated with a higher rate of mortality at 1-year follow-up [14]. Definite criteria for border zone annuli and prospective randomized study are needed to evaluate which valve sizing contributes to better THV performance. In addition, long-term follow-up data on TAVI are necessary to confirm how THV performance impacts on prognosis.
Aortic regurgitation following TAVI in the border zone
In terms of Aortic Regurgitation (AR), including PVL, AR ≥ mild following TAVI was less prevalent in patients with larger valvesizing with underfilling [3], and the presence of AR ≥ moderate reduced in patients with smaller valve sizing with overfilling [5]. It was reported that there was a significant increase in mortality associated with each grade of AR compared with none following TAVI, and the hazard ratio for each 1+ increase in AR was 2.26 [15]. Classification of left ventricular diastolic dysfunction with echocardiography was proposed from the American Society of Echocardiography and the European Association of Cardiovascular Imaging [16]. Along with this classification, several reports about AR following TAVI were published. Patients with left ventricular diastolic dysfunction do not have the ability to increase dimension and compliance for acute increased AR [17]. The presence of PVL ≥ mild following TAVI is associated with increased mortality [18].
In vitro study, even trace AR can increase left ventricular end-diastolic pressure and deteriorate heart function in patients with severe baseline diastolic dysfunction, compared to none AR [19]. Considering previous reports, it is important not to increase AR from baseline and to achieve<mild AR. Larger valve sizing might be a better option in the border zone annulus for patients with severe diastolic dysfunction.
Concern about future coronary access related to redo TAVI
The latest guideline in the United States recommends the transfemoral TAVI as a first-line treatment option for patients with symptomatic aortic stenosis aged >65 years [1]. European guidelines state that the transfemoral TAVI is first-line treatment option for the patients aged ≥ 75 years or aged <75 years with >8% of surgical mortality score [2]. It was reported that the structural valve deterioration rate of a previous generation of balloon expandable valve in 10 years was 6.5% [20], although the sample size was small. There is no data on the long-term balloon-expandable valve durability over 10 years. Considering estimated life expectancy, it is possible that some patients require re-intervention for failed THV. Because SAVR as treatment for early failed THV is reported to have a high mortality rate of 17.1% [21], redo TAVI can become a first-line option for failed THV. However, redo TAVI has an increased risk of impaired coronary access and is considered a risk factor for coronary obstruction owing to sinus sequestration [22,23]. Ochiai, et al. considered patients with two conditions to be at high risk of coronary obstruction: Prior THV commissure level above Sino-Tubular Junction (STJ), and a distance of <2.0 mm between THV and STJ in each coronary sinus [22]. Buzzatti, et al. defined increased risk of coronary obstruction as a coronary ostium below the THV commissures with a valve-to-coronary distance of <2 mm [23]. Recently, radiolucent line-guided TAVI with balloon-expandable THV, which implants at a higher position than the conventional center marker-guided implantation, has been performed to reduce PPI rate. Ishizu, et al. reported that the lower edge of SAPIEN 3 was 1.7 mm below the aortic annular level and PPI rate decreased significantly with radiolucent line-guided TAVI [24]. However, theoretically, the possibility of the THV commissure level being above the STJ level would increase with this technique. It is important to predict the distance from the STJ to THV commissure level in reference to the commercially presented expanded valve height of SAPIEN 3 (Table 2) and STJ height from aortic annulus measured by pre-procedural MDCT. In patients with the possibility of a redo TAVI procedure, smaller valve sizing with overfilling might be a better option if coronary obstruction can be avoided.
Validity of THV implantation with underfilling in the border zone
With balloon-expandable THV, the strongest predictor of annular rupture is MDCT-based area oversizing >20%, and the presence of moderate to severe Left Ventricular Outflow Tract (LVOT)/sub-annular calcification, which is nodule of calcium extending ≥ 5 mm, was considered to have an 8.4-fold and 10.8-fold increased risk of annular rupture, respectively [25]. Some cases would be oversized >20% if THV implantation was performed with nominal filling in border zone annular area defined by each study [3-6] (Tables 1 and 3). Our study suggests that a larger THV implantation with underfilling for selected borderline cases is safe and feasible [3]. However, a smaller THV implantation with nominal filling or overfilling could be selected when outstanding annular or moderate to severe LVOT/sub-annular calcifications are present. There is concern that THV implantation with underfilling is related to suboptimal leaflet movements and coaptation and these might lead to a faster degeneration of THV. In the 2 mm and 3 mm under-expanded THVs, THV leaflets exhibited severe pinwheeling during valve closure, which increased leaflet stresses, and resulted in accelerated fatigue damage of the leaflets. The leaflet fatigue damage in the 1 mm under-expanded case was similar to that in the fully expanded case [26]. In clinical practice, acute recoil phenomenon of approximately 0.5-1.0 mm in the stent frame of balloon-expandable THV was observed [27,28]. It was reported that modest frame under-expansion did not result in a loss of frame strength sufficient to result in progressive stent recoil, deformation, or fracture with CT imaging at 1-year [29]. Taking these findings into consideration, >1 ml underfilling might not be acceptable in terms of valve durability. Long-term follow-up is needed to ensure influence of underfilling on valve durability.
| Authors | Definition of border zone annulus |
|---|---|
| Kawaguchi, et al. [3] | 300-345 mm2 for THV size of 20 mm vs. 23 mm |
| 400-430 mm2 for 23 mm vs. 26 mm | |
| 500-546 mm2 for 26 mm vs. 29 mm | |
| Talmor, et al. [4] | 330-350 mm2 for THV size of 20 mm vs. 23 mm |
| 420-440 mm2 for THV size of 23 mm vs. 26 mm | |
| 530-550 mm2 for 26 mm vs. 29 mm | |
| Patsalis, et al. [5] | 420-440 mm2 for THV size of 23 mm vs. 26 mm |
| 530-550 mm2 for 26 mm vs. 29 mm | |
| Okuno, et al. [6] | THV size located within 5% to each border of the optimal sizing recommendation |
Abbreviation: THV: Transcatheter Heart Valve
Table 1: Definition of border zone annulus in each study.
| SAPEIN 3 Valve size | Valve height following crimping | Expanded height |
|---|---|---|
| 20 mm | 21 mm | 15.5 mm |
| 23 mm | 24.5 mm | 18 mm |
| 26 mm | 27 mm | 20 mm |
| 29 mm | 31 mm | 22.5 mm |
Table 1: Definition of border zone annulus in each study.
| 23 mm THV (407 mm2 for nominal filling) | 26 mm THV (519 mm2 for nominal filling) | 29 mm THV (649 mm2 for nominal filling) | |
|---|---|---|---|
| Annular area (mm2) | |||
| 300 | 35.7% | ||
| 310 | 31.3% | ||
| 320 | 27.2% | ||
| 330 | 23.3% | ||
| 340 | 19.7% | ||
| 350 | 16.3% | ||
| 400 | 29.8% | ||
| 410 | 26.6% | ||
| 420 | 23.6% | ||
| 430 | 20.7% | ||
| 440 | 18.0% | ||
| 500 | 29.8% | ||
| 510 | 27.3% | ||
| 520 | 24.8% | ||
| 530 | 22.5% | ||
| 540 | 20.2% | ||
| 550 | 18.0% | ||
Abbreviation: THV: Transcatheter Heart Valve
Table 3: Oversizing chart for SAPIEN 3 implantation.
Conclusion
In TAVI with SAPIEN 3 for border zone cases, valve size selection should be made according to patient’s background and anatomical features. Although larger THVs contributes to larger EOA, impact of PPM on long-term prognosis is unknown. In addition, larger THVs might be considered for patients with severe diastolic disfunction to reduce the degree of AR. Smaller THVs should be considered for patients with the possibility of a redo TAVI procedure, if coronary obstruction can be avoided, and with outstanding annular or sub-annular calcifications. Considering lifetime management of patients with AS, careful and “tailor-made” TAVI strategies including all the risks for coronary obstruction related to a redo TAVI procedure will be essential to ensure the best treatment option in border zone cases.
Funding
None.
Acknowledgments
Figure 1 is courtesy of Edwards lifesciences.
Conflicts of Interest
Shinichi Shirai is a proctor of transfemoral-TAVI for Edwards SAPIEN 3 valve. The other authors have no conflicts of interest to declare.
References
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 77(4): e25-e197 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 43(7): 561-632 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Kawaguchi T, Miyoshi T, Hayashi M, et al. Efficacy of larger valve sizing with underfilling in balloon-expandable transcatheter aortic valve replacement. Catheter Cardiovasc Interv. 99(7): 2082-91 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Talmor-Barkan Y, Kornowski R, Bar N, et al. Impact of valve size on paravalvular leak and valve hemodynamics in patients with borderline size aortic valve annulus. Front Cardiovasc Med. 9: 847259 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Patsalis PC, Kloppe A, Plicht B, et al. Undersizing but overfilling eliminates the gray zones of sizing for transcatheter aortic valve replacement with the balloon-expandable bioprosthesis. Int J Cardiol Heart Vasc. 30: 100593 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Okuno T, Heg D, Lanz J, et al. Heart valve sizing and clinical outcomes in patients undergoing transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 98(5): E768-e79 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Ihdayhid AR, Leipsic J, Hahn RT, et al. Impact of annular oversizing on paravalvular regurgitation and valve hemodynamics: New insights from PARTNER 3. J Am Coll Cardiol Intv. 14(19): 2158-69 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Mohty D, Malouf JF, Girard SE, et al. Impact of prosthesis-patient mismatch on long-term survival in patients with small St Jude Medical mechanical prostheses in the aortic position. Circulation. 113(3): 420-6 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Bleiziffer S, Ali A, Hettich IM, et al. Impact of the indexed effective orifice area on mid-term cardiac-related mortality after aortic valve replacement. Heart. 96(11): 865-71 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Takagi H, Yamamoto H, Iwata K, et al. A meta-analysis of effects of prosthesis-patient mismatch after aortic valve replacement on late mortality. Int J Cardiol Heart Vasc. 159(2): 150-4 (2012).
[CrossRef] [Google Scholar] [PubMed]
- Dayan V, Vignolo G, Soca G, et al. Predictors and outcomes of prosthesis-patient mismatch after aortic valve replacement. J Am Coll Cardiol Imaging. 9(8): 924-33 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Head SJ, Mokhles MM, Osnabrugge RL, et al. The impact of prosthesis-patient mismatch on long-term survival after aortic valve replacement: A systematic review and meta-analysis of 34 observational studies comprising 27186 patients with 133141 patient-years. Eur Heart J. 33(12): 1518-29 (2012).
- Herrmann HC, Daneshvar SA, Fonarow GC, et al. Prosthesis-patient mismatch in 62,125 patients following transcatheter aortic valve replacement: From the STS/ACC TVT registry. J Am Coll Cardiol. 72(22): 2701-11 (2018).
- Miyasaka M, Tada N, Taguri M, et al. Incidence, predictors, and clinical impact of prosthesis-patient mismatch following transcatheter aortic valve replacement in Asian patients: The OCEAN-TAVI registry. J Am Coll Cardiol Intv. 11(8): 771-80 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Jones BM, Tuzcu EM, Krishnaswamy A, et al. Prognostic significance of mild aortic regurgitation in predicting mortality after transcatheter aortic valve replacement. J Thorac Cardiovasc Surg. 152(3): 783-90 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 29(4): 277-314 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Gotzmann M, Lindstaedt M, Mügge A. From pressure overload to volume overload: Aortic regurgitation after transcatheter aortic valve implantation. Am Heart J. 163(6): 903-11 (2012).
[CrossRef] [Google Scholar] [PubMed]
- Kampaktsis PN, Bang CN, Wong SC, et al. Prognostic importance of diastolic dysfunction in relation to post procedural aortic insufficiency in patients undergoing transcatheter aortic valve replacement. Catheter Cardiovasc Interv. 89(3): 445-51 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Okafor I, Raghav V, Midha P, et al. The hemodynamic effects of acute aortic regurgitation into a stiffened left ventricle resulting from chronic aortic stenosis. Am J Physiol Heart Circ Physiol. 310(11): H1801-7 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Sathananthan J, Lauck S, Polderman J, et al. Ten year follow-up of high-risk patients treated during the early experience with transcatheter aortic valve replacement. Cathet Cardiovasc Interv. 97(3): E431-E437 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Jawitz OK, Gulack BC, Grau-Sepulveda MV, et al. Reoperation after transcatheter aortic valve replacement: An analysis of the society of thoracic surgeons database. J Am Coll Cardiol Intv. 13(13): 1515-25 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Ochiai T, Oakley L, Sekhon N, et al. Risk of coronary obstruction due to sinus sequestration in redo transcatheter aortic valve replacement. J Am Coll Cardiol Intv. 13(22): 2617-27 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Buzzatti N, Montorfano M, Romano V, et al. A computed tomography study of coronary access and coronary obstruction after redo transcatheter aortic valve implantation. EuroIntervention. 16(12): e1005-e13 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Ishizu K, Shirai S, Kawaguchi T, et al. Effect of radiolucent line-guided balloon-expandable transcatheter aortic valve implantation on subsequent pacemaker rate. Am J Cardiol. 165: 72-80 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Barbanti M, Yang TH, Rodès Cabau J, et al. Anatomical and procedural features associated with aortic root rupture during balloon-expandable transcatheter aortic valve replacement. Circulation. 128(3): 244-53 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Martin C, Sun W. Transcatheter valve underexpansion limits leaflet durability: Implications for valve-in-valve procedures. Ann Biomed Eng. 45(2): 394-404 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Kawaguchi T, Yamaji K, Ishizu K, et al. Effect of postdilatation following balloon expandable transcatheter aortic valve implnatation. Catheter Cardiovasc Interv. 96(6): E630-E639 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Nombela-Franco L, Ribeiro HB, Urena M, et al. Incidence, predictive factors and haemodynamic consequences of acute stent recoil following transcatheter aortic valve implantation with a balloon-expandable valve. Eurointervention. 9(12): 1398-406 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Tan JS, Leipsic J, Perlman G, et al. A strategy of underexpansion and Ad Hoc post-dilation of balloon-expandable transcatheter aortic valves in patients at risk of annular injury: Favorable mid-term outcomes. J Am Coll Cardiol Intv. 8(13): 1727-32 (2015).
[CrossRef] [Google Scholar] [PubMed]