Review Article - Clinical Investigation (2018) Volume 8, Issue 3
LEOSound - A new device for long-term recording of wheezing and cough in pediatric and adult patients with asthma (during sleep)
- Corresponding Author:
-
Department of Internal Medicine
Division of Pneumology
Intensive Care and Sleep Medicine
Hospital of the University of Marburg, Germany
E-mail: koehleru@med.uni-marburg.de
Submitted Date: 07 June 2018; Accepted Date: 19 June 2018; Published Date: 22 June 2018
Abstract
Children with asthma often have a decreased performance during the day because of night-time asthma symptoms. Asthma is still poorly controlled in more than 50% of patients despite the availability of very effective drugs. GINA defined criteria for asthma control include asking about daytime symptoms, limitation of activity, night-time symptoms/awakenings and need for reliever treatment. Standardized and validated questionnaires such as asthma control test (ACT) help to assess the level of asthma control. Approximately 30 to 40% of asthmatic children are affected by sleep disturbances. Asthma symptoms during night-time must be seen as a special feature of asthma. Computerized cough, wheeze and respiratory rate monitoring provides additional and objective information on current night-time symptoms. To reduce risk for children with asthma, control of night-time symptoms is important to improve respiratory function and quality of sleep.
Keywords
Asthma, Pediatrics, Night-time, Sleep quality, Daytime performance, Long-term monitoring and LEOSound
Introduction
Many children with asthma have a decreased performance during the day because of night-time asthma symptoms and consecutive sleep disturbances [1-6]. Because of the economic and social burden of asthma health care providers should be aware of this problem. Asthma is a complex and chronic inflammatory disorder which is associated with reversible airway obstruction and bronchial hyperresponsiveness. It is one of the most prevalent chronic diseases in children and prevalence further increases worldwide. Typical symptoms of asthma are breathlessness, cough, wheezing and chest tightness. The tools for asthma control which are available in clinical practice are subjective (questionnaires, diary cards) and objective ones (lung function). GINA defined criteria for asthma control include asking about daytime symptoms, limitation of activity, night-time symptoms/awakenings and need for reliever treatment. Control of asthma symptoms and a good quality of life are the main goals of therapy.
Mechanisms of Night-Time Asthma
The cause of night-time asthma is still not fully understood. Increased airway inflammation and bronchial hyperreactivity during night-time may be related to heightened parasympathetic tone, airway cooling, allergen exposition or hormonal changes [7-9]. Lung function is usually highest at 4:00 pm and lowest at 4:00 am, so asthma symptoms are more pronounced in second half of the night. The association of asthma with a variety of comorbidities like chronic rhinosinusitis, obstructive sleep apnea (OSA), gastrooesophageal reflux disease (GERD) and obesity is known in adults; its relevance for childhood asthma is less clear and hence under further discussion [1,2].
Night-time Asthma Symptoms
Asthma symptoms during night-time must be seen as a special feature of asthma or an uncontrolled status, which are associated with increased morbidity, mortality and decreased quality of life. Wheezing is the acoustic manifestation of lower airway obstruction limiting airflow in a collapsible bronchial system and is typically diagnosed by auscultation. Wheezes are adventitious continuous respiratory sounds with a musical quality, a duration > 250 ms and a frequency range from 400 up to 2000 Hz [10]. Wheezing may be either a benign self-limited process or a symptom of respiratory disease like asthma. Wheezing can originate from airways of any size and requires sufficient airflow to initiate airway oscillation. Typical for bronchial obstruction in asthmatic patients is wheezing during the expiration cycle. The presence of biphasic inand expiratory wheezing is a sign for a very severe bronchoconstriction or a combination of upper and lower airway origin stenosis or constriction. As far as we know, most children do not wheeze during sleep, however intermittent mild wheezing has been reported in children without asthmatic symptoms. It is unknown how common nocturnal wheezing is in preschool children without asthma. The combination of daytime symptoms and the concurrent presence of wheezing at night reported by parents is an alarm sign for uncontrolled asthma symptoms. In addition, a non-productive cough, which worsens at night, may be also a typical symptom for asthma. In children, the information about night-time symptoms is often based on the observation of the parents. Children are not able to give adequate information on night-time symptoms and the parents thus often underestimate the severity of symptoms.
Sleep Quality of Patients with Night- Time Asthma
In pediatrics approximately 30 to 40% of children are affected by sleep disturbances [3,4,11,12]. Nighttime asthma symptoms may disrupt the continuity of sleep by awakenings or arousals and can lead to daytime sleepiness, reduced mental and physical health, altered immune function, reduced school performance and increased school absences. Until very recently, asthma induced sleep disturbances received comparatively little attention. However, increased daytime sleepiness because of night-time symptoms has been reported in a few studies with stable asthmatic children. In the study by Chugh et al. in 38 out of 40 stable asthmatic children (95%) night-time symptoms of asthma, sleep disturbances and poorer sleep quality were evident [12]. Sleep disturbances were reported in 60% of the asthmatics and included daytime sleepiness, difficulty in maintaining sleep, early morning awakenings and struggle against sleep during daytime. Meijer et al. reported the presence of nocturnal symptoms in almost half of 796, Strunk et al. in a third of 1041 children with asthma [4,13]. Most findings of the studies rely on self-reporting by the children or their parents. Evaluating sleep quality to achieve good control of asthma is important since nocturnal symptoms may disturb sleep. Poor asthma control may increase the risk for sleep problems and a higher rate of exacerbations. Luyster et al. reported that poorer sleep quality is an independent predictor of worse asthma control and quality of life in non-severe and severe asthma patients [14]. A study by Desager et al. describes increased daytime sleepiness and tiredness in wheezing schoolaged children [15]. Meltzer et al. demonstrated that out of 298 adolescents (age 12-17 years; 48% with asthma) almost 40% of the patients with severe asthma reported clinically significant insomnia [16]. Daytime sleepiness was also found to be more present in adolescents with severe asthma compared to those patients with mild or no asthma. Asthma severity and insomnia severity were predictors for daytime sleepiness. Sleep fragmentation and poor sleep quality are associated with asthma control and quality of life. Sleep quality, daytime activity and academic performance improve when children with nocturnal asthma and disturbed daytime psychological function are successfully treated.
Self and Parental Questionnaires to Assess Night-Time Asthma Symptoms are of only Small Value
Nocturnal respiratory symptoms in children with asthma are difficult to diagnose because patients often do not wake up until severe obstruction occurs. Previous studies evaluated night-time respiratory situation by waking up the patient in order to obtain data by peak-flow. However, interruption of a patients sleep cannot represent the actual respiratory situation during sleep. Questionnaire-based studies or diary cards are of small value, because parents often differ in their understanding of wheeze and cough [17,18]. Furthermore, the reports of parents or children do not reflect the real occurrence of wheezes and cough episodes throughout the night. Usually wheeze episodes are only detected by auscultation. If wheezing can be heard without stethoscope, it is only a small, noticeable part of a problem, and does not necessarily reflect the total occurrence. Therefore, further diagnostic tools are necessary to monitor symptoms during sleep objectively.
Why do we Need Objective Long-Term Monitoring of Asthma Symptoms During Sleep?
The keystone of asthma management is the achievement and maintenance of asthma control [1]. Many patients do not report night-time symptoms to their doctor or the doctor does not ask for those. Lack of awareness of nocturnal asthma symptoms can lead to a worse asthma control and impaired daytime activity. It is obvious that asthmatic children who suffer from tiredness during daytime do not have a stable asthma during sleep. Lung function testing during the day is not representative for the 24h time circle. Children up to the age of 5 years are also often not able to perform a correct spirometry. Peak flow measurements during the night are only possible when the patient is awake, but this status does not represent sleep. Computerized cough and wheeze monitoring is a practical and noninvasive method for assessing asthma symptoms in children and adults with asthma [19-22]. It provides additional and objective information on current symptoms in chronic respiratory diseases. A trend plot of nighttime cough and wheeze can be helpful for identifying the timing and the distribution of wheeze and cough activity during sleep
The LEOSound-system
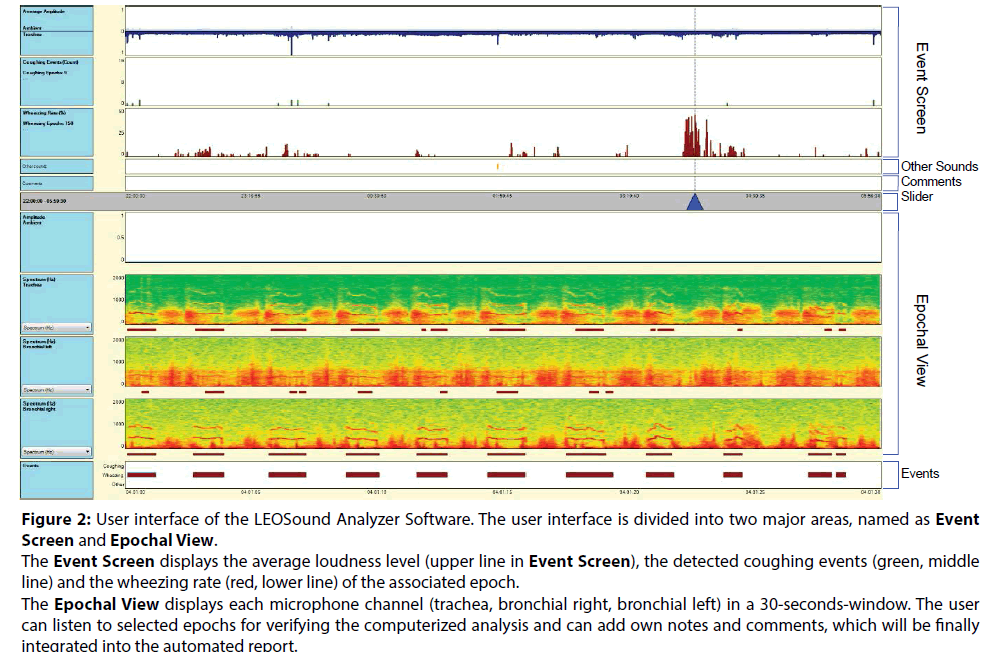
LEOSound is a commercial available, automated respiratory sound monitoring device, which records respiratory sounds continuously by three small bioacoustical sensors attached to the trachea and to the back of the patient (Figure 1). Beside this, an ambient microphone is integrated. Thus, it is possible to differentiating respiratory sounds from speech, and other ambient sounds. The validated system works like a ‘long-term stethoscope’ and allows objective 24 hours respiratory sound auscultation at patients home or at the hospital. The 24 hours interval is especially useful to determine frequency and diurnal variation of coughs in patients with asthma or with persistent cough of unknown cause. The LEOSound analyzer software automatically evaluates the data for the presence of respiratory sounds like cough and wheezing and the respiratory rate and stores the results and the raw data in a database. The records as well as the automatic ratings are shown on a graphic illustrated user interface (Figure 2). Additionally, the user can listen on all three channels to verify the automated analysis. LEOSound is the only respiratory sound monitoring system so far, which analyses both, wheezing, as well as cough events automatically. The relationship between chronic cough and disease entities such as gastrooesophageal reflux, obstructive sleep apnea and chronic sinusitis are further indications for using the LEOSound system.
Figure 2: User interface of the LEOSound Analyzer Software. The user interface is divided into two major areas, named as Event Screen and Epochal View. The Event Screen displays the average loudness level (upper line in Event Screen), the detected coughing events (green, middle line) and the wheezing rate (red, lower line) of the associated epoch. The Epochal View displays each microphone channel (trachea, bronchial right, bronchial left) in a 30-seconds-window. The user can listen to selected epochs for verifying the computerized analysis and can add own notes and comments, which will be finally integrated into the automated report.
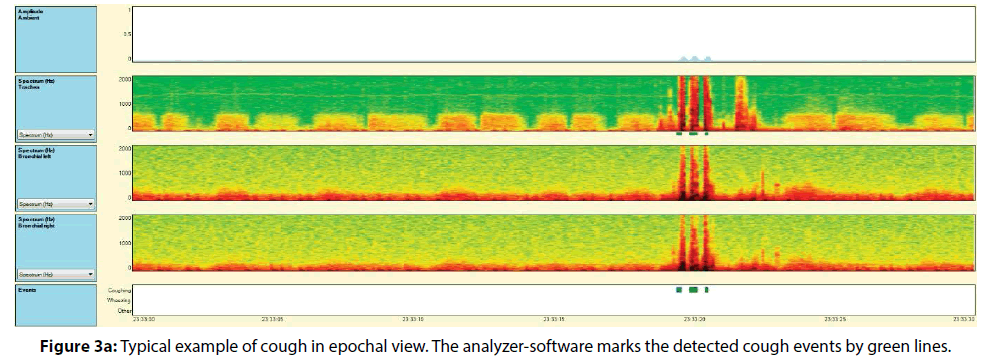
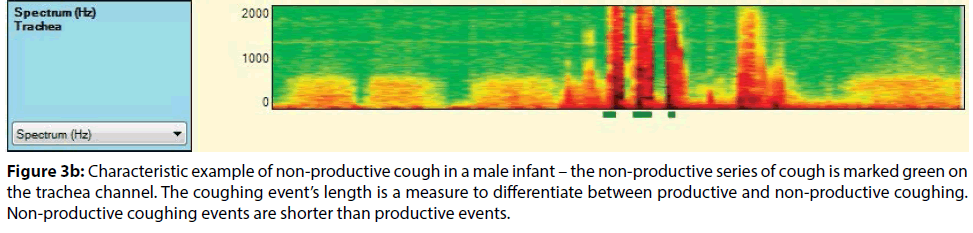
As part of a validation study of LEOSound in children, we compared software-based analysis with medical expert’s assessment. The results show high sensitivity of 93%, and specificity of 99% for the detection of cough. Figures 3a and 3b show a typical cough event in epochal view (3a) and an enlarged view to single events (3b), exemplarily demonstrating the sensitivity of the algorithms (green lines). Wheezing can be identified by its typical frequency band in the spectrogram. Sensitivity and specificity for wheezing detection is 98% and 96%, respectively [23]. The LEOSound system allows an objective recording of cough and wheezing events, without having to rely on the help of the patient. In children and adults with asthma control of night-time symptoms is important to improve respiratory function and quality of sleep.
Figure 3b: Characteristic example of non-productive cough in a male infant – the non-productive series of cough is marked green on the trachea channel. The coughing event’s length is a measure to differentiate between productive and non-productive coughing. Non-productive coughing events are shorter than productive events.
References
- Dinakar C, Chipps BE. AAP Section on allergy and immunology, AAP Section on pediatric pulmonology and sleep medicine. Clinical tools to assess asthma control in children. Pediatrics 139 (2017).
- Banasiak NC. Understanding the Relationship Between Asthma and Sleep in the Pediatric Population. J Pediatr Health Care 30: 546-550 (2016).
- Janson C, De Backer W, Gislason T, et al. Increased prevalence of sleep disturbances and daytime sleepiness in subjects with bronchial asthma: a population study of young adults in three European countries. Eur Respir J 9: 2132-2138 (1996).
- Meijr GG, Postma DS, Wempe JB, Gerritsen J. Frequency of nocturnal symptoms in asthmatic children attending a hospital out-patient-clinic. Eur Respir J 8:2076-2080 (1995).
- Diette GB, Markson L, Skinner EA, Nguyen TT, Algatt-Bergstrom P, Wu AW. Nocturnal asthma in children affects school attendance, school performance, and parents’ work attendance. Arch Pediatr Adolesc Med 154:923-928 (2000).
- Ginsberg D. An unidentified Monster in the Bed – Assessing Nocturnal Asthma in Children. J Med 12:31-38 (2009).
- Khan WH, Mohsenin V, D’Ambrosio CM. Sleep in Asthma. Clin Chest Med 35:483-493 (2014).
- Sutherland ER. Nocturnal Asthma: Underlying Mechanisms and Treatment. Curr Allergy Asthma Rep 5: 161-167 (2005).
- Turner-Warwick M. Epidemiology of nocturnal asthma. Am J Med 85: 6-8 (1988).
- Pasterkamp H, Brand PL, Everard M, Garcia-Marcos L, Melbye H, Priftis KN. Towards the standardisation of lung sound nomenclature. Eur Respir J 47: 724-732 (2016).
- Storms WW, Bodmann SF, Nathan RA, Bayer P. Nocturnal asthma symptoms may be more prevalent than we think. J Asthma 31: 313-318 (1994).
- Chugh IM, Khanna P, Shah A. Nocturnal symptoms and sleep disturbances in clinically stable asthmatic children. Asian Pac J Allergy Immunol 24: 135-142 (2006).
- Strunk RC, Sternberg AL, Bacharier LB, Szefler SJ. Nocturnal awakening caused by asthma in children with mild-to-moderate asthma in the childhood asthma management program. J Allergy Clin Immunol 110: 395-403 (2002).
- Luyster FS, Teodorescu M, Bleecker E, et al. Sleep quality and asthma control and quality of life in non-severe and severe asthma. Sleep Breath 16: 1129-1137 (2012).
- Desager KN, Nelen V, Weylerr JJ, De Backer WA. Sleep disturbances and daytime symptoms in wheezing school-aged children. J Sleep Res 14: 77-82 (2005).
- Meltzer L, Ullrich M, Szefler SJ. Sleep Duration, Sleep Hygiene, and Insomnia in Adolescents with Asthma. J Allergy Clin Immunol Pract 2: 562-569 (2014).
- Falconer A, Oldman C, Helms P. Poor agreement between reported and recorded nocturnal cough in asthma. Pediatr Pulmonol 13: 541-545 (1993).
- Chang AB, Newman RG, Carlin JB, Phelan PD, Robertson CF. Subjective scoring of cough in children: parent-completed vs child-completed diary cards vs an objective method. Eur Respir J 11: 462-466 (1998).
- Koehler U, Brandenburg U, Weissflog A, Sohrabi K, Gross V. LEO Sound, an innovative procedure for acoustic long-term monitoring of asthma symptoms (wheezing and coughing) in children and adults. Pneumologie 68: 277-281 (2014).
- Kroenig J, Hildebrandt O, Weissflog A, et al. Long-term Recording of Night-Time Respiratory Symptoms in Patients with Stable COPD II–IV. Pulmon 14:498-503 (2017).COPD:J Chron Obstruct
- Koehler U, Hildebrandt O (Hrsg). Atem- und Atemnebengeräusche bei Kindern und Erwachsenen – Akustische Langzeitregistrierung und –analyse. UNI-MED Verlag, Bremen-London-Boston (2017).
- Guenter K, Cassel W, Hildebrandt O, et al. Control of respiratory symptoms during sleep in patients with stable bronchial asthma. DMW (in press).
- Gross V, Scholtes M, Sohrabi K. Validation of the LEOSound®-monitor for standardized detection of cough and wheezing in children. Worldsleep 2015 - 7th World Congress of the World Sleep Federation, hosted by ESRS. Istanbul, TR. Abstract book, no 468: 143(2015).