Review Article - Interventional Cardiology (2011) Volume 3, Issue 1
Lessons for the treatment of bifurcation lesions: from nowadays to the future
- Corresponding Author:
- Andrejs Erglis
University of Latvia, Latvian Centre of Cardiology
Pauls Stradins Clinical University Hospital
Pilsonu Street 13, Riga, 1002, Latvia
Tel: +37 167 069 541
Fax: +37 167 069 548
E-mail: Arina.Bingeliene@uhn.ca
Abstract
Keywords
bifurcation, drugs, restenosis, stents, technique
Coronary bifurcation lesions account for 15–20% of all coronary lesions that require percutaneous coronary intervention (PCI) [1]. Bifurcation stenosis is one of the most complex coronary lesions requiring endovascular treatment because the lumen of both the main vessel and the side branch needs to be restored. The best approach for the management of a bifurcation to achieve optimal procedural outcomes and, more importantly, long-term success with low restenosis rates and low major adverse clinical event (MACE) rates is still debated. Balloon angioplasty alone to treat bifurcation lesions has resulted in relatively low angiographic success and high restenosis rates [2,3]. Although the introduction of bare-metal stents (BMSs) resulted in more predictable results and higher success rates, angiographic restenosis rates still remained high. The introduction of drug-eluting stents (DESs) in clinical practice has altered the treatment perspective when dealing with this type of lesion; however, abrupt side-branch closure with the single-stent strategies, together with the risk of thrombosis and restenosis associated with the complex two-stent techniques, remains a predictor of adverse clinical outcomes.
Bifurcation types
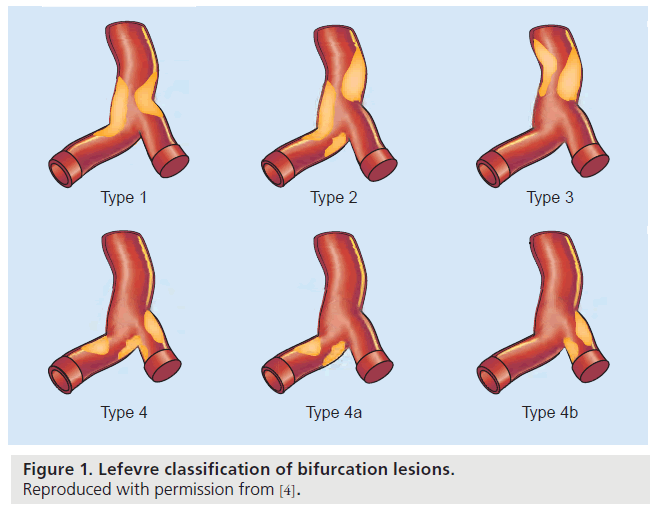
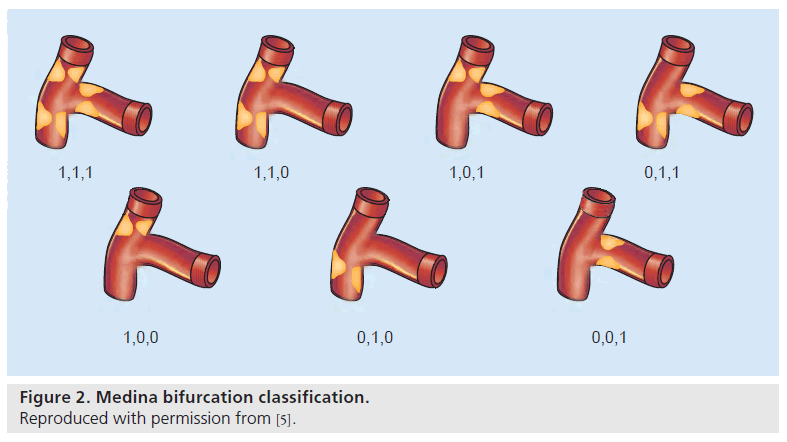
Bifurcations vary in plaque burden, the location of plaque, the angle between branches, the diameter of the branches and the bifurcation site. No two bifurcations are identical, and no single strategy exists that can be applied to every bifurcation. Thus, the more important issue in bifurcation PCI is selecting the most appropriate strategy for an individual bifurcation. The most frequently used older bifurcation classification is the Lefevre classification (Figure 1) [4]. However, Lefevre and other older classifications of coronary bifurcation lesions require significant efforts of memorization. The Medina classification (Figure 2) is a simplified and universal classification of bifurcation lesions, is straightforward and does not need to be memorized, even though it provides all the information contained in the others [5]. It consists of recording any narrowing in excess of 50% in each of the three arterial segments of the bifurcation in the following order: proximal main vessel, distal branch and side branch – ‘1’ is used to indicate the presence of a significant stenosis and ‘0’ represents the absence of stenosis. The three figures are separated by commas. It has been suggested that the Medina classification should also contain information regarding the lesion length, especially for the side branch, or the presence of calcifications.
Figure 1: Lefevre classification of bifurcation lesions. Reproduced with permission from [4].
Figure 2: Medina bifurcation classification. Reproduced with permission from [5].
Simple bifurcations are those that represent side-branch origins (1,1,0; 1,0,0; and 0,1,0) with Medina’s classification. Their treatment is simple; it is often sufficient to simply implant a stent in the main vessel, as long as it covers the side-branch origin. Interventions should only be performed on the side branch if the ostium is compromised. However, in complex bifurcations, in which the proximal 1,0,1, distal 0,1,1 or both 1,1,1 components of the side-branch origin and the main vessel are involved, treatment with an additional stent could be effective.
Single stent versus double stenting for coronary bifurcation lesions
When stenting is used, a major question is whether both the main vessel and the side branch should be stented. Such double stenting is appealing because it produces attractive postprocedural angiographic results. However, there have been concerns about long-term major adverse cardiac events and, in particular, stent thrombosis with adjacent stents.
In the Nordic study, 413 patients were randomized to a simple treatment strategy, stenting of the main vessel and optional stenting of the side branch, or to a complex stenting strategy, involving stenting of both the main vessel and side branch. In this study, only sirolimus-eluting stents (SESs) were used. After 14 months of follow-up, the rates of stent thrombosis and MACEs (9.5 and 8.2%; p = not significant in single- and double- stent subgroups, respectively) were low and independent of treatment complexity. Mortality was observed in 2.4 versus 1.0% and non-PCIrelated myocardial infarction in 2.0 versus 1.0% in the single- and double-stent strategies, respectively. The simple stenting strategy used in the main vessel was associated with lower rates of procedure-related biomarker elevation [6,7].
The British Bifurcation Coronary Study randomized trial of simple versus complex drugeluting stenting for bifurcation lesions was published recently. In the simple strategy, the main vessel was stented, followed by optional kissing-balloon dilatation/T-stent placement. In the complex strategy, both vessels were systematically stented (‘culotte’ or ‘crush’ techniques) with mandatory kissing-balloon dilatation. This study analyzed a total of 500 patients, of which 82% had true bifurcation lesions according to Medina bifurcation classification. In the simple group (n = 250), 66 patients (26%) had kissing balloons in addition to main-vessel stenting, and seven (3%) had undergone T-stenting. In the complex group (n = 250), 89% of culotte (n = 75) and 72% of crush (n = 169) cases were completed successfully with final kissing-balloon inflations. MACEs occurred in 8.0% of the simple group versus 15.2% of the complex group (hazard ratio: 2.02; 95% CI: 1.17–3.47; p = 0.009). Myocardial infarction occurred in 3.6 versus 11.2%, respectively (p = 0.001), and in-hospital major adverse cardiovascular events occurred in 2.0 versus 8.0% (p = 0.002), respectively [8].
Gao et al. prospectively compared singleversus double-stent techniques for coronary bifurcation lesion treatment in 566 consecutive patients. In this study, only DESs were used, in the one-stent strategy, kissing balloon was mandatory and the two-stent strategy included crush, culotte, Y-, V-, and kissing-stent strategies. MACE rates were higher in the two-DES group than in the one-DES group (5.5 vs 2.0%; p = 0.032), which were mainly contributed to by acute myocardial infarction (4.5 vs 1.4%; p = 0.032) rather than death and target lesion revascularization (TLR; 0 vs 0.5%, p = 0.389; 1.4 vs 2.7%, p = 0.352). Stent thrombosis rates were higher in the two-DES group than in the one-DES group (0.6 vs 2.7%; p = 0.042). At the 7-month angiographic follow-up, in the main branch, no difference in restenosis rate in the one-DES group compared with the two-DES group (9.8 vs 11.9%; p = 0.652) was observed, but in the side branch, the restenosis rate was higher in the one-DES group (33.6 vs 15.5%; p = 0.004) [9].
The Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus- Eluting Stents (CACTUS) trial was a prospective, randomized, multicenter study comparing two different techniques of stenting using SES with mandatory final kissing-balloon inflation in true bifurcations: elective crush stenting, and stenting of only the main branch, with provisional side-branch T-stenting. A total of 350 patients were enrolled in the study. At 6 months, the rate of restenosis was similar in both the main branch (4.0 vs 8.7%; p = 0.09) and the side branch (14.6 vs 12.5%; p = 0.61) for the doublestenting (crush plus crossover from provisional) and main-branch-only stenting groups, respectively. Additional stenting on the side branch in the provisional-stenting group was required in 31% of lesions. Rates of MACEs were similar in the two groups (15.8% in the crush group vs 15% in the provisional-stenting group) [10].
Ferenc et al. published results of a randomized study, which assigned 101 patients with a coronary bifurcation lesion to routine T-stenting with a SES in both branches and 101 patients to provisional T-stenting with SES placement in the main branch followed by kissing-balloon angioplasty. Angiographic follow-up revealed stenosis of the side branch of 23.0 ± 20.2% after provisional T-stenting (19% with a side branch stent) and of 27.7 ± 24.8% after routine T-stenting (p = 0.15). The 1-year overall incidence of TLR was 10.9% after provisional and 8.9% after routine T-stenting (p = 0.64) [11].
Colombo et al. assigned patients randomly to two groups receiving either stenting of both branches or stenting of the main branch with provisional stenting of the side branch. In total, 85 patients were enrolled and only a SES was used. The restenosis rate at 6 months was not significantly different between the double-stenting (28.0%) and the provisional side-branch stenting (18.7%) groups [12].
Pan et al. compared single stenting versus double stenting for coronary bifurcations in a randomized study in 91 patients with true coronary bifurcation lesions. All patients received rapamycin-eluting stents at the main vessel, covering the side branch. A total of 44 patients were randomized to receive a second stent at the sidebranch origin (a T-stent and modified T-stent technique was used). At 6-month angiographic re-evaluation, restenosis of the main vessel was observed in one (2%) patient from the singlestent group and in four (10%) from the double stent group, and restenosis of the side branch appeared in two (5%) and six (15%) patients, respectively [13].
Yamashita et al. published results of 92 patients with bifurcation lesions treated with a two-stent strategy versus a one-stent strategy in the main branch and balloon angioplasty of the side branch. In this study, BMSs were used. At 6-month follow-up, the angiographic restenosis rate in the two-stent group was 62% and was 48% in the one-stent group, and the TLR rates (38 vs 36%, respectively) were similar in the two groups. There was no difference in the incidence of 6-month total MACE (51 vs 38%) [14].
The provisional side-branch intervention strategy (provisional strategy) is preferred for most bifurcation lesions because no single study, to our knowledge, has shown the benefit of systematic two stenting over this strategy. The British Bifurcation Coronary Study and Gao et al. were the only studies reporting data demonstrating that a systematic two-stent technique results in higher in-hospital and major adverse cardiovascular event rates at follow-up; however, this difference in both studies was largely driven by acute myocardial infarction.
Double-stent techniques for coronary bifurcation lesions
In a number of coronary bifurcation lesions, both the main vessel and the side branch need stent coverage.
A total of 424 patients were randomized to crush and culotte stenting in the Nordic study. At 6-month follow-up there were no significant differences in MACEs between the groups (crush: 4.3%, culotte: 3.7%; p = 0.87). The rates of procedure-related increase in biomarkers of myocardial injury were 15.5% in the crush versus 8.8% in the culotte group (p = 0.08). The angiographic end points of in-segment and instent restenosis of the main vessel and/or side branch after 8 months were found in 12.1 versus 6.6% (p = 0.10) and in 10.5 versus 4.5% (p = 0.046) in the crush and the culotte groups, respectively [15].
Hoye et al. identified 231 consecutive patients treated with DES implantation with the crush technique, with SESs and paclitaxel-eluting stents (PESs), for 241 bifurcation lesions. The in-hospital MACE rate was 5.2%. At 9 months, ten (4.3%) patients had experienced an event consistent with possible postprocedural stent thrombosis; however, in this study, left main stem cases were included. Survival free of MACEs was 83.5% and independent predictors of MACE were left main therapy (odds ratio: 3.79, 95% CI: 1.76–8.14; p = 0.001) and the treatment of patients with multivessel disease (odds ratio: 4.21, 95% CI: 0.95–18.56; p = 0.058) [16].
Ge et al. analyzed 181 consecutive patients who were treated with DESs with the crush technique. The authors demonstrated that compared with the absence of final kissing balloon, the crush-stenting technique with final kissing balloon was associated with more favorable long-term outcomes. Restenosis rate of the side branch was lower in the final kissing group than in the nonkissing-balloon group (11.1 vs 37.9%; p < 0.001). In this study, the intervention without kissing balloon and diabetes were predictors of TLR. The authors reported three (1.7%) cases of intraprocedural and five (2.8%) cases of post-procedural stent thrombosis. Premature discontinuation of dual antiplatelet therapy and older age was associated with the occurrence of post-procedural stent thrombosis [17].
Ge et al., in 2005, analyzed 182 consecutive patients who underwent crush or T-technique intervention in bifurcation lesions with DESs (SESs or PESs). When final kissing balloon postdilatation was performed, crush-group patients had a significantly lower late lumen loss (0.23 vs 0.37 mm; p = 0.02) and restenosis rate (8.6 vs 26.5%; p = 0.04) in the side branch at angiographic follow-up after 6–8 months. At 1-year clinical follow-up, the crush group compared with the T-stent group had lower rates of TLR (16.5 vs 32.8%; p = 0.02) [18].
Chen et al. published study results conducted in 311 patients with true bifurcation lesions, which were randomly divided into classical and double-kissing crush groups. The incidence of stent thrombosis was 3.2% in the classical crush group (5.1% without and 1.7% with final kissing- balloon inflation) and 1.3% in the doublekissing crush group. The cumulative 8-month MACE rate was 24.4% in the classical crush group and 11.4% in the double-kissing crush group (p = 0.02). The TLR-free survival rate was 75.4% in the classical crush group and 89.5% in the double-kissing crush group (p = 0.002) [19].
BMSs for coronary bifurcation lesions
There are no large prospective randomized trials addressing long-term clinical outcome after the placement of BMSs versus balloon dilatation or surgery and different stenting techniques. The majority of the information is based on reports from registries and retrospective data [20–27]. A limitation in the treatment of bifurcation stenoses with BMSs is the high rates of restenosis, in particular with the two-stent strategy. The restenosis rate was 25–62% in the two-stent group versus 12.5–48% in the single-stent group, and the TLR rate was 24–43% in the two-stent group versus 8–36% in the single-stent group.
DESs for coronary bifurcation lesions
The introduction of DESs in the treatment of coronary bifurcation lesions has been considered to have improved operational outcomes and to decrease the need for repeated revascularization. In the Arterial Revascularisation Therapies Study II, event rates were similar in bifurcation and nonbifurcation lesions [1]. Moreover, Erglis et al. from the Nordic Study Group demonstrated that stenting of both bifurcation branches with either the culotte or crush techniques yielded relatively low restenosis rates [15].
Brar et al. recently published a meta-analysis of six randomized controlled trials [28]. Each of these trials compared a provisional versus a two-stent strategy for the treatment of bifurcation lesions. The results demonstrated that in a total of 1641 patients, there was no difference in efficacy, measured target vessel revascularization or percentage diameter stenosis between provisional T-stenting and the routine two-stent strategy for the treatment of bifurcation lesions. While death and stent thrombosis occurred at similar rates in both treatment groups, myocardial infarction was more common with the two-stent strategy. The relative and absolute reduction in myocardial infarction with provisional stenting was 43 and 3.0%, respectively (p = 0.01). The higher rate of myocardial infarction with the two-stent strategy was consistent with the results of individual trials.
Kissing balloon
Adriaenssens et al. reported that in their series of 134 bifurcation lesions in 132 patients treated with the culotte technique, final kissing balloon tended to have a protective effect against stent thrombosis [29]. In addition, after the crush technique, final kissing balloon significantly reduced the side-branch late lumen loss (0.24 ± 0.50 mm vs 0.58 ± 0.77 mm; p < 0.001) at 9 months angiographic follow-up [16]. In all modern bifurcation trials (e.g., the British Bifurcation Coronary Study [BBC] ONE trial and the CACTUS trial), kissing balloon after use of complex two-stent techniques has been mandatory.
Unprotected left main coronary artery bifurcation treatment
Although the introduction of DESs has significantly improved the outcome of patients with unprotected left main coronary artery (ULMCA) stenosis treated with PCI [30–35], there are still major drawbacks associated with bifurcation lesions in the setting of ULMCA stenosis [36,37]. Although it is generally believed that ULMCA bifurcation lesions treated with PCI carry a worse prognosis than ostial and midshaft lesions, the evidence for this notion is based on a small number of studies that enrolled a limited number of patients [38,39].
A recently published observational study on ULMCA stenosis involving 19 high-volume Italian centers enrolled 1111 patients with ULMCA stenosis treated with DESs (334 patients had ostial or midshaft lesions and 777 had bifurcations). The adjusted hazard ratio of the risk of 2-year MACEs of patients with bifurcations versus patients without bifurcations was 1.50 (p = 0.024). However, the authors observed that there was a significant difference between patients with bifurcations treated with two stents and those without bifurcations (p = 0.001), but not between patients with bifurcations treated with one stent and those without bifurcations (p = 0.38). The results of this study suggest that not all ULMCA bifurcations should be considered in the same way, and that those patients who can be treated with one stent, irrespective of lesion location, have more favorable outcomes.
Plaque modification before stenting
The issue of restenosis in complex anatomies such as bifurcated coronary lesions remains unclear. In our opinion, plaque debulking with directional coronary atherectomy or modification with a scoring device before stent deployment could minimize arterial injury and subsequent neointimal proliferation, and could prevent restenosis formation. We believe that plaque modification with a scoring device or directional coronary atherectomy before stenting minimizes plaque shifting between the main branch and side branch and thus could help to avoid sidebranch stenting as well as giving better stent apposition with reduced inflation pressure, even if very long stents are deployed.
Tsuchikane et al. reported registry data of 99 patients with bifurcation lesions, who received directional coronary atherectomy before stenting. Simple stenting was achieved in 97 patients. The 9-month binary restenosis rates in the main branch and side branch were 1.1 and 3.4%, respectively. TLR was performed only in two patients [40].
We performed a single-center substudy (Nordic I, II+ Riga bifurcation registry) with the purpose of demonstrating the safety and efficacy of plaque modification with a scoring device prior to main-vessel stenting and/or side-branch treatment in bifurcation lesions [41]. We compared cutting balloon (n = 209) versus noncutting balloon (n = 347) interventions in bifurcation lesions. Primary end points were cardiac death, myocardial infarction, stent thrombosis, TLR and target vessel revascularization after 8 months. Our results showed that TLR was lower in the cutting balloon group (5.3%; n = 11) compared with the noncutting balloon group (11.0%; n = 38; p = 0.021).
These results are very promising and we believe that plaque debulking before stenting, especially in complex bifurcated lesions, can avoid the need for complex stenting and may provide a good long-term outcome in patients within the first year [40,41].
Implication of intravascular ultrasound, optical coherence tomography & fractional flow reserve for coronary bifurcation treatment
In bifurcation lesions, restenosis occurs predominantly at the ostium of the side branch. Increased neointimal hyperplasia or chronic stent recoil together with stent underexpansion at the side-branch ostium cannot be excluded as the causes of restenosis in bifurcation lesions.
Costa et al. analyzed 40 patients with bifurcation lesions who underwent crush stenting with a SES under intravascular ultrasound (IVUS) guidance. ‘Incomplete crushing’, defined as incomplete apposition of the side-branch or main-vessel stent struts against the main-vessel wall proximal to the carina, was observed in more than 60% of nonleft main lesions. The authors concluded that in the majority of bifurcation lesions treated with the crush technique, the smallest minimum stent area appeared at the side-branch ostium, which contributed to a higher restenosis rate at this location [42].
Intravascular ultrasound analyses have specifically excluded bifurcation segments from the assessment of incomplete stent apposition [43,44], because the prominent artifacts generated by the stent struts and the low resolution preclude detailed assessment of the complex geometry of a bifurcation. The unique high resolution of optical coherence tomography (OCT) has enabled in vivo visualization of coronary vessels and stent struts at micro-scale levels to assess local vessel responses and perform strut-level evaluation to examine strut apposition and coverage. While the PCI of bifurcations still remains associated with high restenosis and thrombosis rates in both BMS and DES interventions, evaluation of stent strut apposition immediately after stent deployment in OCT-guided PCI and stent strut coverage at follow-up is critical, especially in long, calcified and bifurcation lesions.
Kyono et al. published the subanalysis of Optical Coherence Tomography for Drug Eluting Stent Safety (ODESSA), a prospective randomized trial designed to evaluate the healing of overlapped DES versus BMSs (SESs, PESs, zotarolimus-eluting stents (ZESs) and Liberté BMSs) [45]. Bifurcation segments with side-branch diameters larger than 1.5 mm by angiography were analyzed and demonstrated a variable pattern of strut coverage in the bifurcation among stent technologies, with a high percentage of PES floating struts remaining uncovered at 6-month follow-up. There were 12,656 struts in 61 bifurcation segments (PES: 16, SES: 14, ZES: 23, Liberté BMS: eight) from 46 patients obtained at 6 months. PESs had the highest rate of uncovered struts in side-branch ostium (PES: 60.1%, SES: 17.0%, ZES: 13.2%, BMS: 12.3%; p < 0.0001), whereas SESs demonstrated the highest rate of uncovered struts opposite to the ostium (PES: 3.8%, SES: 14.0%, ZES: 1.5%, BMS: 0.0%; p = 0.0025).
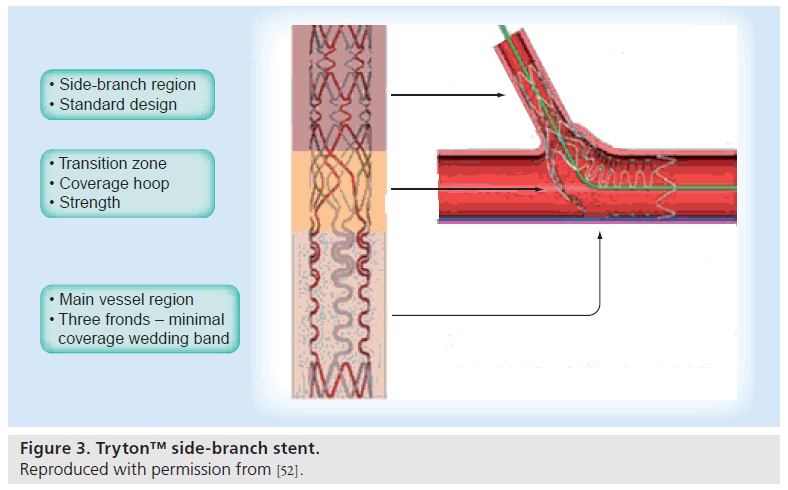
Another study analyzed nine patients treated with the Tryton stent, who underwent postprocedural OCT examination [46]. The total percentage of malaposed struts per patient was 18.1 ± 8.7%; however, the prevalence of malaposed struts was significantly higher at the level of the bifurcation (33.3%) than in both the proximal segment and the distal segment (18.5 and 9.8%, respectively; p = 0.011).
Fractional flow reserve (FFR) is an easily obtainable physiological parameter that is stenosis specific and reflects both the degree of stenosis and the myocardial territory supplied by the specific artery [47]. When evaluating the functional significance of ostial side-branch stenoses, it must be remembered that coronary angiography often leads to an overestimation (and less often to an underestimation) of the functional significance of ostial-branch lesions; however, measurement of the FFR can overcome the limitations of coronary angiography for assessing whether any lesions are difficult to visualize or are functionally significant. Koo et al. performed a study testing a strategy of DES placement in the main branch, with provisional treatment of the diseased side branch only if the FFR was under 0.75. When the FFR was under 0.75, the study protocol required kissing-balloon angioplasty. During a median follow-up of 6 months, patients whose treatment had been guided by FFR had excellent outcomes, similar to the outcomes of the group of patients whose sidebranch treatments were guided by angiography. Interestingly, not one patient in the FFR group required a stent in the side branch after balloon angioplasty [48].
Especially dedicated bifurcation stents
When restenosis occurs, it is typically found in the side-branch ostium [49], which might result from incomplete coverage of the ostium or suboptimal expansion at the ostium [50]. Several types of dedicated bifurcation stents have been designed with the notion that they will provide adequate coverage of the main branch and the ostium of the side branch.
The SLK-View™ stent (Advanced Stent Technologies, CA, USA) is a stainless-steel flexible slotted-tube stent with a side aperture located between the proximal and distal sections to facilitate access to the side branch after deployment of the stent in the main branch. Ikeno et al. studied 81 patients with 84 de novo coronary artery bifurcation lesions [51]. Patients underwent SLK-View stent implantation with subsequent kissing balloon postdilatation. The procedural success rate was 97.6%. Binary restenosis rate at 6-month follow-up was 28.3% for the main vessel and 37.7% for the side branch. The TLR rate at 6 months was 21%.
The Tryton Side-Branch Stent (Tryton Medical, Inc., MA, USA) is a balloon-expandable cobalt chromium BMS, designed specifically to scaffold the ostium of the side branch (Figure 3). In particular, the proximal portion of the stent consists of three fronds that allow facile wiring of the main vessel. After deploying the stent in the side branch, any stent can be placed in the main branch to complete the bifurcating architecture [52].
Figure 3: Tryton™ side-branch stent. Reproduced with permission from [52].
The Tryton I First-In-Man (FIM) trial assessed the safety and performance of the Tryton Side- Branch Stent when used with a standard DES to treat bifurcation lesions within the coronary circulation in a total of 30 patients. In this trial, the Tryton Side-Branch Stent demonstrated acceptable procedural success (93.3%) and clinical safety up to 6 months after the index procedure with a MACE rate of 9.9%. A single case of angiographic restenosis was noted due to a lesion proximal to the main-vessel stent (TLR: 3.3%). No restenosis in the side branch was observed [52].
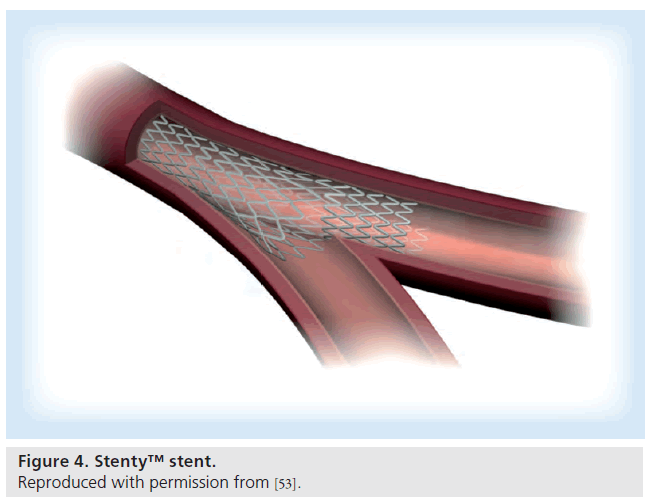
The Stentys™ coronary stent (Stentys SAS, Paris, France) is a provisional, self-expanding nitinol drug-eluting (paclitaxel) or BMS designed to treat bifurcations with significant side branches [53]. The stent shape is adapted to the bifurcation anatomy after implantation, owing to the stent’s self-expanding nitinol Z-shaped mesh that is linked by small interconnections that can be disconnected by balloon angioplasty to provide access to the side branch and full ostium coverage (Figure 4). In OPEN I – a multicenter, prospective single-arm study – 40 patients were enrolled and clinically followed up for 4 years. Procedural success was achieved in 39 out of 40 cases (95.5%). The MACE at 30 days was 5.1% as a result of one non-Q-wave myocardial infarction occurring following the procedure and one ischemia-driven revascularization event 6 days after the procedure [54].
Figure 4: Stenty™ stent. Reproduced with permission from [53].
The Axxess stent (Devax Inc., CA, USA) belongs to this category of dedicated bifurcation lesion stents [55]. It is a self-expanding DES, deployed at the level of the carina, which provides easy access to the distal branches that can subsequently be provisionally treated with PCI depending on the disease status of these branches. The rationale behind this stent is to provide an anatomically tailored treatment for the bifurcation with maximum drug coverage and minimum overlap and deformation of the stent struts. The prospective multicenter Axxess Plus registry enrolled 139 patients in whom, together with the Axxess stent, SESs or PESs were used as additional stents to optimize the procedure, and the side-branch treatment was left to the operator’s discretion. Stenting of the side branch was performed in approximately half of the lesions. Post-hoc analysis demonstrated that the lesions treated with stent deployment in the side branch had better procedural outcomes and better late results with under 10% restenosis of the side branch, compared with more than 20% side branch restenosis in those treated with balloon-only angioplasty [56]. In another study, a total of 302 patients were treated with 299 Axxess stents (99%). Additional stenting of one branch was performed in 21.7% of patients (17.7% in the parent vessel, 4% in the side branch), and of both branches in 64.7%. The cumulative 9-month MACE rate was 7.7%. Subacute and late-stent thrombosis occurred in 0.7% and 0.3% of patients. Total restenosis was 6.4% (3.6% in the parent vessel, 4.3% in the side branch), and late loss was 0.20 ± 0.41 mm in the parent vessel and 0.17 ± 0.34 mm in the side branch. In the Axxess stent segment, percentage neointimal volume obstruction was 4.3 ± 5.2% [57].
Future perspective
▪ Ongoing modern trials
During 2010 we began a prospective, nonrandomized OCT-guided study, where patients with native coronary artery disease with an at least 75% diameter stenosis involving at least two segments of the bifurcation by a visual or angiographic estimate. Lesion pretreatment with a scoring device (cutting balloon) is mandatory followed by OCT imaging and everolimus-eluting stent (Xcience V™, Abbott Vascular, CA, USA) implantation in the main branch with intended provisional T-stenting. Finally, postprocedural result evaluation of both the main and side branch with OCT and IVUS should be performed.
This trial will help us to understand lesion morphology in bifurcations using different intracoronary imaging methods. One of the questions concerns whether OCT will be able to substitute IVUS or whether both methods should be used to complement each other. It is already clear that OCT, owing to its high spatial resolution, allows accurate evaluation of strut apposition and assessment of the ostium of the bifurcation, as well as evaluation of precise stent strut endothelization at follow-up. It is clinically decisive because DES may suppress neointimal growth at the cost of a delayed healing process, with lower rates of endothelial stent coverage, more persistent fibrin deposits and an increased inflammatory response [58,59]. Moreover, when intimal hyperplasia is negated by powerful antiproliferative coating, malapposition may persist for years after stent implantation and create an increased risk of late stent thrombosis [60]. This knowledge of uncovered struts could reduce stent thrombosis in conjunction with prolongation of dual antiplatelet therapy.
For calcified lesions, using the scoring device is suggested, and the necrotic core, which could act as a measurement of plaque vulnerability, is suggested to be covered with stent. It will be interesting to see whether possible adverse events at follow-up periods will correlate with plaque composition. Moreover, it is interesting to compare two different tissue characterization methods: IVUS (iMap™ IVUS Tissue Characterization [Boston Scientific Corp., MN, USA]) and virtual histology (VH)-IVUS (Eagle Eye™, Volcano Therapeutics Inc., CA, USA). Both methods were designed to analyze lesion compositions; however, they evolved differently from different scientific backgrounds.
Another ongoing multicenter prospective two-arm (blinded to grayscale IVUS and VH-IVUS information versus nonblinded) trial is the Bifurcation Lesion Analysis and Stenting (BLAST) randomized study. With regard to VH-IVUS, special attention will be paid to the impact of the un- or partially covered confluent necrotic core against the lumen surface on long-term clinical outcomes. The BLAST study is planned to enroll approximately 220 patients with coronary bifurcation lesions and to treat patients with the onestent technique using DESs with provisional T-stenting or culotte.
▪ Biodegradable stents
Despite the development and progression of metallic stents, their routine use continues to have limitations, such as stent thrombosis, which requires prolonged antiplatelet therapy, and also mismatch of the stent to the vessel size. New directions in coronary PCI include the invention of biodegradable stents. By contrast, biodegradable stents, once they are bioabsorbed, leave behind only the healed natural vessel, allowing restoration of vasoreactivity with the potential of vessel remodeling. Late stent thrombosis is unlikely, since the stent will be gone, and prolonged antiplatelet therapy is not necessary. Already, results of several studies with biodegradable stents have been reported [59] but, still, further research is mandatory.
Biodegradable polymer stents seem very promising for especially complex lesion interventions such as coronary bifurcations, and we believe that adequate lesion pretreatment with a scoring device using intracoronary imaging methods such as IVUS and OCT could provide optimal results; however, further research is required before biodegradable stents can substitute the conventional BMSs or DESs.
Conclusion
Improvements in bifurcation stent techniques, the results from randomized controlled trials and registry data have led to the conclusion that stenting of the main vessel and provisional sidebranch stenting should be the first-line strategy in the majority of lesions. Moreover, plaque modification with a plaque-debulking device may give positive impact on TLR. Possibly, selective use of IVUS, with or without tissue characterization and/or OCT, may play a role in the selection of optimum techniques and final balloon size.
However, the mechanism of side-branch neointimal hyperplasia and the implications of the bifurcation stent technique still require further evaluation to ensure that we understand the long-term outcomes after PCI in this complex lesion subgroup.
Financial & competing interests disclosure
Andrejs Erglis has received grant research support from Abbott Vascular, consulting fees/honoraria from Boston Scientific, and has been affiliated with J&J Cordis and Abbott Vascular. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪ Single stenting versus double stenting in coronary bifurcations is the strategy of choice.
▪ When the double-stent technique is used, final kissing balloon is mandatory.
▪ Introduction of drug-eluting stents in the treatment of coronary bifurcation lesions has decreased restenosis rates and repeat revascularizations.
▪ Modification of plaque morphology before stenting in bifurcation lesions could have special importance.
▪ Implementation of intravascular visualization methods could improve outcomes in coronary bifurcation interventions.
References
Papers of special note have been highlighted as:
▪ of interest
- Tsuchida K, Colombo A, Lefevre T et al.: The clinical outcome of percutaneous treatment of bifurcation lesions in multivessel coronary artery disease with the sirolimuseluting stent: insights from the Arterial Revascularization Therapies Study part II (ARTS II). Eur. Heart J. 28(4), 433–442 (2007).
- Weinstein JS, Baim DS, Sipperly ME, McCabe CH, Lorell BH: Salvage of branch vessels during bifurcation lesion angioplasty: acute and long-term follow-up. Catheter Cardiovasc. Diagn. 22(1), 1–6 (1991).
- Mathias DW, Mooney JF, Lange HW et al.: Frequency of success and complications of coronary angioplasty of a stenosis at the ostium of a branch vessel. Am. J. Cardiol. 67(6), 491–495 (1991).
- Lefevre T, Louvard Y, Morice MC et al.: Stenting of bifurcation lesions: classification, treatments, and results. Catheter Cardiovasc. Interv. 49, 274–283 (2000).
- Medina A, Suarez de Lezo J, Pan M: [A new classification of coronary bifurcation lesions]. Rev. Esp. Cardiol. 59(2), 183 (2006).
- Steigen TK, Maeng M, Wiseth R et al.: Randomized study on simple versus complex stenting of coronary artery bifurcation lesions. The Nordic Bifurcation Study. Circulation 114, 1955–1961 (2006).
- Jensen JS, Galløe A, Lassen JF et al.: Safety in simple versus complex stenting of coronary artery bifurcation lesions. The Nordic Bifurcation Study 14-month follow-up results. Eurointervention 4, 229–233 (2008).
- Hildick-Smith D, de Belder AJ, Cooter N et al.: Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions. The British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation 121, 1235–1243 (2010).
- Gao Z, Yang YJ, Gao RL: Comparative study of simple versus complex stenting of coronary artery bifurcation lesions in daily practice in chinese patients. Clin. Cardiol. 31, 317–322 (2008).
- Colombo A, Bramucci E, Sacca S et al.: Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations. Circulation 119, 71–78 (2009).
- Ferenc M, Gick M, Kienzle RP et al.: Ramdomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur. Heart J. 29, 2859–2867 (2008).
- Colombo A, Moses JW, Morice MC et al.: Randomized study to evaluate sirolimuseluting stents implanted at coronary bifurcation lesions. Circulation 109, 1244–1249 (2004).
- Pan M, de Lezo JS, Medina A et al.: Rapamycin-eluting stents for the treatment of bifurcated coronary lesions: a randomized comparison of a simple versus complex strategy. Am. Heart J. 148, 857–864 (2004).
- Yamashita T, Nishida T, Adamian MG et al.: Bifurcation lesions: two stents versus one stent – immediate and follow-up results. J. Am. Coll. Cardiol. 35, 1145–1151 (2000).
- Erglis A, Kumsars I, Niemela M et al.; for the Nordic PCI Study Group: Randomized comparison of coronary bifurcation stenting with the crush versus the culotte technique using sirolimus eluting stents. Circ. Cardiovasc. Interv. 2, 27–34 (2009).
- Hoye A, Iakovou I, Ge L et al.: Long-term outcomes after stenting of bifurcation lesions with the ‘crush’ technique: predictors of an adverse outcome. J. Am. Coll. Cardiol. 47, 1949–1958 (2006).
- Ge L, Airoldi F, Iakovou I et al.: Clinical and angiographic outcome after implantation of drug-eluting stents in bifurcation lesions with the crush stent technique. J. Am. Coll. Cardiol. 46, 613–620 (2005).
- Ge L, Iakovou I, Cosgrave J et al.: Treatment of bifurcation lesions with two stents: one year angiographic and clinical follow up of crush versus T stenting. Heart 92, 371–376 (2006).
- Chen SL, Zhang JJ, Ye F et al.: Study comparing the double kissing (DK) crush with classical crush for the treatment of coronary bifurcation lesions: the DKCRUSH-1 bifurcation study with drug-eluting stents. Eur. J. Clin. Invest. 38, 361–371 (2008).
- Al Suwaidi J, Berger PB, Rihal CS et al.: Immediate and long-term outcome of intracoronary stent implantation for true bifurcation lesions. J. Am. Coll. Cardiol. 35(4), 929–936 (2000).
- Chevalier B, Glatt B, Royer T, Guyon P: Placement of coronary stents in bifurcation lesions by the ‘culotte’ technique. Am. J. Cardiol. 82, 943–949 (1998).
- Yamashita T, Nishida T, Adamian MG et al.: Bifurcation lesions: two stents versus one stent–immediate and follow-up results. J. Am. Coll. Cardiol. 35(5), 1145–1151 (2000).
- Pan M, Suarez de Lezo J, Medina M et al.: Simple and complex stent strategies for bifurcated coronary arterial stenosis involving the side branch origin. Am. J. Cardiol. 83, 1320–1325 (1999).
- Anzuini A, Briguori C, Rosanio S et al.: Immediate and long-term clinical and angiographic results from Wiktor stent treatment for true bifurcation narrowings. Am. J. Cardiol. 88(11), 1246–1250 (2001).
- Brunel P, Commeau P, Konig R et al.: Assessment of coronary bifurcation lesion treated with stent implantation on parent vessel and with balloon or stent on the side branch. Circulation 98(17), (1998) (Abstract I-639).
- Brunel P, Lefevre T, Darremont O, Louvard Y: Provisional T-stenting and kissing balloon in the treatment of coronary bifurcation lesions: results of the French multicenter ‘TULIPE’ study. Catheter Cardiovasc. Interv. 68(1), 67–73 (2006).
- Rux S, Sonntag S, Schulze R et al.; BISCOR Investigators: Acute and long-term results of bifurcation stenting (from the Coroflex Registry). Am. J. Cardiol. 98(9), 1214–1217 (2006).
- Brar SS, Gray WA, Dangas G et al.: Bifurcation stenting with drug-eluting stents: a systematic review and meta-analysis of randomized trials. EuroIntervention 5, 475–484 (2009).
- Adriaenssens T, Byrne RA, Dibra A et al.: Culotte stenting technique in coronary bifurcation disease: angiographic follow-up using dedicated quantitative coronary angiographic analysis and 12-month clinical outcomes. Eur. Heart J. 29, 2868–2876 (2008).
- Chieffo A, Stankovic G, Bonizzoni E et al.: Early and mid -term results of drug-eluting stent implantation in unprotected left main. Circulation 111, 791–795 (2005).
- Kim YH, Dangas GD, Solinas E et al.: Effectiveness of drug-eluting stent implantation for patients with unprotected left main coronary artery stenosis. Am. J. Cardiol. 101, 801–806 (2008).
- Meliga E, Garcia-Garcia HM, Valgimigli M et al.: Longest available clinical outcomes after drug -eluting stent implantation for unprotected left main coronary artery disease: the DELFT (Drug Eluting stent for Left Main) Registry. J. Am. Coll. Cardiol. 51, 2212–2219 (2008).
- Palmerini T, Marzocchi A, Marrozzini C et al.: Preprocedural levels of C-reactive protein and leukocyte counts predict 9-month mortality after coronary angioplasty for the treatment of unprotected left main coronary artery stenosis. Circulation 112, 2332–2338 (2005).
- Park SJ, Kim YH, Lee BK et al.: Sirolimuseluting stent implantation for unprotected left main coronary artery stenosis: comparison with bare metal stent implantation. J. Am. Coll. Cardiol. 45, 351–356 (2005).
- Seung KB, Park DW, Kim YH et al.: Stents versus coronary-artery bypass grafting for left main coronary artery disease. N. Engl. J. Med. 358, 1781–1792 (2008).
- Colombo A, Moses JW, Morice MC et al.: Randomized study to evaluate sirolimuseluting stents implanted at coronary bifurcation lesions. Circulation 109, 1244–1249 (2004).
- Chieffo A, Park SJ, Valgimigli M et al.: Favorable long-term outcome after drug-eluting stent implantation in nonbifurcation lesions that involve unprotected left main coronary artery: a multicenter registry. Circulation 116, 158–162 (2007).
- Baim DS, Mauri L, Cutlip DC: Drug-eluting stenting for unprotected left main coronary artery disease: are we ready to replace bypass surgery? J. Am. Coll. Cardiol. 47, 878–881 (2006).
- Lee CH, Degertekin M, van Domburg RT et al.: Impact of different anatomical patterns of left main coronary stenting on long-term survival. Am. J. Cardiol. 92, 718–720 (2003).
- Tsuchikane E, Aizawa T, Tamai H et al.: Pre-drug-eluting stent debulking of bifurcated coronary lesions. J. Am. Coll. Cardiol. 50, 1941–1945 (2007).
- Erglis A: Arterial scoring: cosmetic or curative. Presented at: Transcatheter Cardiovascular Therapeutics 2009. San Francisco, CA, USA, 21–25 September (2009).
- Costa RA, Mintz GS, Carlier SG et al.: Bifurcation coronary lesions treated with the ‘crush’ technique. J. Am. Coll. Cardiol. 46, 599–605 (2005).
- Cook S, Wenaweser P, Togni M et al.: Incomplete stent apposition and very late stent thrombosis after drug eluting stent implantation. Circulation 115, 2426–2434 (2007).
- Kimura M, Mintz GS, Carlier S et al.: Outcome after acute incomplete sirolimus eluting stent apposition as assessed by serial intravascular ultrasound. Am. J. Cardiol. 98, 436–442 (2006).
- Kyono H, Guagliumi G, Sirbu V et al.: Optical coherence tomography (OCT) strut-level analysis of drug-eluting (DES) in human coronary bifurcations. EuroIntervention 6, 69–77 (2010).
- Tyczynski P, Ferrante G, Kukreja N et al.: Optical coherence tomography assessment of a new dedicated bifurcations stents. Eurointervention 5, 544–551 (2009).
- Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL: Experimental basis of determining maximum coronary myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after PTCA. Circulation 87, 1354–1367 (1993).
- Koo BK, Park KW, Kang HJ et al.: Physiological evaluation of the provisional side branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur. Heart J. 29, 726–732 (2008).
- Moussa I, Costa RA, Leon MB et al.: A prospective registry to evaluate sirolimuseluting stents implanted at coronary bifurcation lesions using the ‘crush technique’. Am. J. Cardiol. 97(9), 1317–1321 (2006).
- Ormiston JA, Webster MW, El Jack S et al.: Drug eluting stents for coronary bifurcations: bench testing of provisional side-branch strategies. Catheter Cardiovasc. Interv. 67(1), 49–55 (2006).
- Ikeno F, Kim YH, Luna J et al.: Acute and long-term outcomes of the novel side access (SLK-View) stent for bifurcation coronary lesions: a multicenter nonrandomized feasibility study. Catheter Cardiovasc. Interv. 67(2), 198–206 (2006).
- Onuma Y, Muller R, Ramcharitar S et al.: First-In-Man (FIM) study: six month clinical and angiographic outcome, analysis with new quantitive coronary angiography dedicated for bifurcation lesions. EuroIntervention 3, 546–552 (2008).
- Laborde JC, Borenstein N, Behr L, Ramcharitar S: Stentys coronary bifurcation stent. EuroIntervention 3(1), 162–165 (2007).
- Verheye S, Grube E, Ramcharitar S et al.: First-In-Man (FIM) study of the Stentys™ bifurcation stent – 30 days results. EuroIntervention 4, 566–571 (2009).
- Agostoni P, Verheye S: Bifurcation stenting with a dedicated biolimus-eluting stent: x-ray visual enhancement of the final angiographic result with ‘StentBoost Subtract’. Catheter Cardiovasc. Interv. 70, 233–236 (2007).
- Grube E, Buellesfeld L, Neumann FJ et al.: Six-month clinical and angiographic results of a dedicated drug-eluting stent for the treatment of coronary bifurcation narrowings. Am. J. Cardiol. 99, 1691–7 (2007).
- Verheye S, Agostoni P, Dubois CL et al.: 9-month clinical, angiographic, and intravascular ultrasound results of a prospective evaluation of the Axxess self-expanding biolimus A9-eluting stent in coronary bifurcation lesions. J. Am. Coll. Cardiol. 53(12), 1031–1039 (2009).
- Finn AV, Kolodgie FD, Harnek J et al.: Differential response of delayed healing and persistent inflammation at sites of overlapping sirolimus- or paclitaxel-eluting stents. Circulation 112, 270–278 (2005).
- Finn AV, Nakazawa G, Joner M et al.: Vascular responses to drug eluting stents: importance of delayed healing. Arterioscler. Thromb. Vasc. Biol. 27, 1500–1510 (2007).
- Joner M, Finn AV, Farb A et al.: Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J. Am. Coll. Cardiol. 48, 193–202 (2006).
▪ Reports on the Nordic Bifurcation study: pioneering randomized bifurcation study on simple versus complex stenting.
▪ Reports on the Nordic Bifurcation study: pioneering randomized bifurcation study on simple versus complex stenting.
▪ Reports on the British Bifurcation Coronary study – the latest randomized trial on simple versus complex bifurcation stenting.
▪ Describes the randomized study on a simple versus complex bifurcation study.