Research Article - Clinical Investigation (2022) Volume 12, Issue 11
LEVEL OF KNOWLEDGE ABOUT BLOOD BORNE DISEASE IN NURSES WORKING IN TERTIARY CARE HOSPITAL
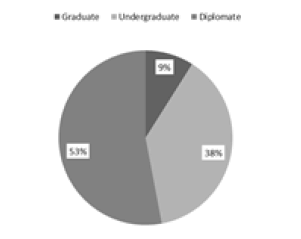
57 (53.3%) nurses are diplomate, 10 (9.3%) are graduates, and 40 (37.4) are undergraduates (Figure 2).
The duration of nurses is different for different ages with a mean 8.170, median 5.00, mode 1.0, and standard deviation of 7.3978 (Table 2).
Table 2. Duration of service in years
| Duration in years | Frequency | Percent |
|---|---|---|
| 0.1 | 1 | 0.9 |
| 0.3 | 2 | 1.9 |
| 1 | 14 | 13.1 |
| 2 | 8 | 7.5 |
| 2.5 | 1 | 0.9 |
| 3 | 13 | 12.1 |
| 4 | 5 | 4.7 |
| 5 | 10 | 9.3 |
| 6 | 8 | 7.5 |
| 7 | 5 | 4.7 |
| 8 | 2 | 1.9 |
| 9 | 5 | 4.7 |
| 10 | 5 | 4.7 |
| 12 | 2 | 1.9 |
| 13 | 2 | 1.9 |
| 15 | 2 | 1.9 |
| 16 | 1 | 0.9 |
| 17 | 1 | 0.9 |
| 18 | 3 | 2.8 |
| 19 | 3 | 2.8 |
| 20 | 5 | 4.7 |
| 21 | 2 | 1.9 |
| 22 | 2 | 1.9 |
| 23 | 3 | 2.8 |
| 26 | 1 | 0.9 |
| 33 | 1 | 0.9 |
| Total | 107 | 100 |
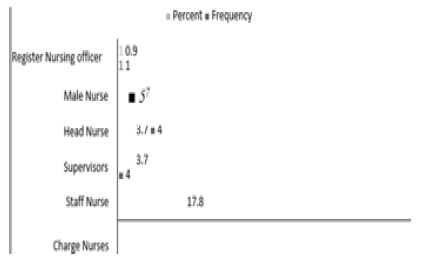
There are 74 (69.2%) charge nurses, 19 (17.8%) are staff nurses, 4 (3.7%) are supervisors, 4 (3.7%) are head nurses, 5 (4.7%) are male nurses and 1 (0.9%) are registered, nursing officer (Figure 3) [9].
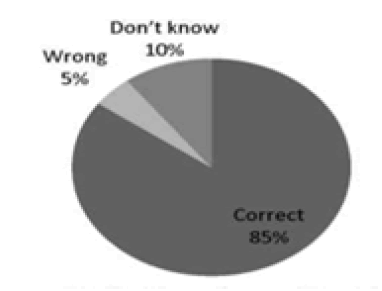
91 (85 correctly defined the term blood-borne disease, and 5 (4.7%) cannot be defined %) nurses (Figure 4). Correctly and 11 9 (10.3%) did it know about this definition.
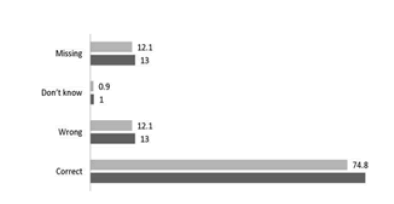
80 (74.8%) nurses knew about the name and causative agents of blood-borne diseases, 13 (12.1%) wrongly answered, 1 (.9%) did not know about it, 13 (12.1%) are missing (Figure 5).
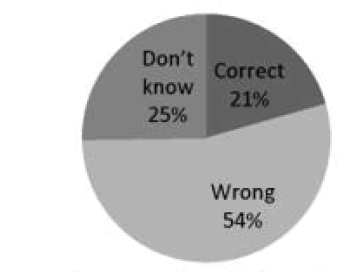
22 (20.6%) nurses correctly answered about the source of infection of blood-borne disease, 58 (54.2%) wrongly answered, and 27 (25.2%) did not know about the source of infection of the blood borne diseases (Figure 6).
Figure 6: Source of infection of blood-borne diseases.
30 (28.0%) Nurses Correctly answered about the risk factors of blood-borne disease, 24 (22.4%) wrongly answered and 53 (49.5%) don’t know the risk factors of these diseases (Table 3).
Table 3: Risk factors of blood-borne diseases.
| Frequency | Percent | |
|---|---|---|
| Correct | 30 | 28 |
| Wrong | 24 | 22.4 |
| Don’t know | 53 | 49.5 |
| Total | 107 | 100 |
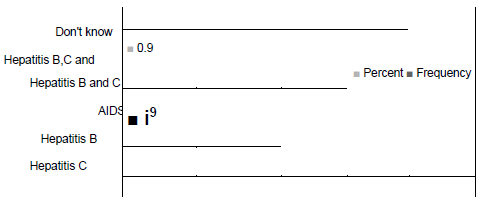
The majority of nurses answered that hepatitis C is the most common blood-borne disease in Pakistan that is 38 (35.5%), 13 (12.1%) answered hepatitis B, 2 (1.9%) answered AIDS, 23 (21.5%) answered both hepatitis B and C, 1 (.9%) answered about hepatitis B, C and AIDS and 30(28.0%) don’t know about these diseases (Figure 7).
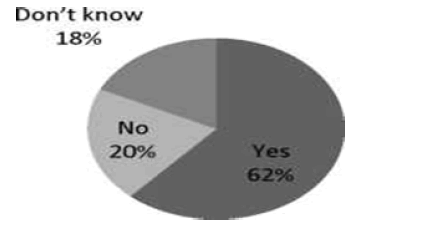
66 (61.7%) answered that these diseases can be transmitted by blood. 22 (20.6%) answered that these diseases cannot be transmitted besides blood. 19 (17.8%) don’t know about the transmission of these diseases besides blood (Figure 8).
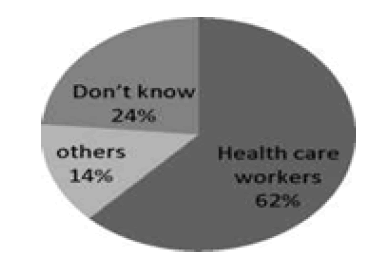
66 (61.7%) answered that healthcare workers are more susceptible to blood-borne diseases, 25 (23.4%) don’t know about the more susceptible person, 15 (14.0%) answered others are more susceptible than healthcare workers (Figure 9).
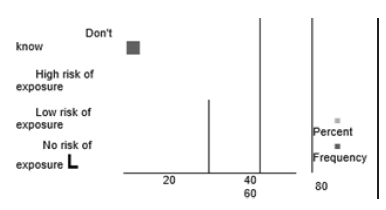
Only 2 (1.9%) answered that their work has no risk of exposure to contracting blood-borne infection, 30 (28.0%) answered that has a low risk of exposure, 62 (57.9%) answered that has a high risk of exposure, 13 (12.1%) don’t know about its exposure (Figure 10).
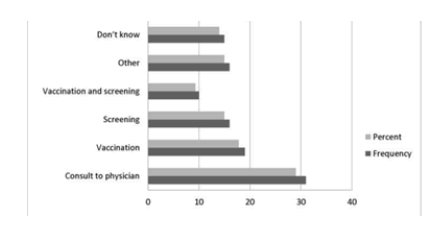
21 (19.6%) answered that Hepatitis B is preventable. 2 (1.9%) answered that Hepatitis C is preventable, 3 (2.8%) answered about AIDS, 8 (7.5%) answered that Hepatitis B and C both are preventable, 34 (31.8%) answered that all blood borne diseases are preventable, 39 (36.4%) don’t about it (Figure 11).
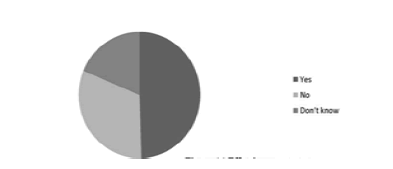
53(49.5%) answered that blood-borne diseases have effective treatment, 34 (31.8%) answered that they are not treatable, 20 (18.7%) don’t about it (Figure 12) (Table 4).
Table 4. Correct Answers
| Category | Frequency | Percent |
|---|---|---|
| Don’t know | 13 | 12.1 |
| Satisfactory | 20 | 18.7 |
| Good | 63 | 58.9 |
| Excellent | 11 | 10.3 |
| Total | 107 | 100 |
Discussion
Bloodborne pathogens are microorganisms such as viruses or bacteria that are carried in the blood and can cause disease in people. There are many different blood-borne pathogens, including malaria, syphilis, and brucellosis, and most notably Hepatitis B (HBV), Hepatitis C (HCV), and the Human Immunodeficiency Virus (HIV) [20]. It is important to know the ways exposure and transmission are most likely to occur in a particular situation, like nurses providing first aid to a patient in the casualty ward, handling blood samples in the laboratory, cleaning up blood from a hallway, etc. Healthcare workers, emergency response and public safety personnel, and other workers can be exposed to blood through needle sticks and other sharps injuries, mucous membranes, and skin exposures. But nurses are more important in this situation because nurses are the main force that comes in contact with patients on a routine basis. Some of those patients might have blood-borne diseases like HIV, Hepatitis B & C, etc which will be easily transferred to these nurses. These infections are major threats to healthcare workers specially nurses. Knowledge about Hepatitis B, C, and AIDS is crucial for healthcare workers because of the increasing incidence of these infections [21].
In this Study, About 90% of nurses know about the term blood-borne disease and only 10% don’t know about this term. Only 28% of nurses know about the risk factors of getting these infections which is very disastrous. Our findings are similar to those found in national and international reports [22].
Many of them said Hepatitis C is more common in Pakistan. And about the transmission other than blood. More than 60 percent know that healthcare workers are more susceptible to getting these deadly infections a finding that is comparable with some Egyptian studies [23]. There is no vaccine available for the prevention of hepatitis C and AIDS. Still, 22.4% claimed the availability of a vaccine that can protect against hepatitis C and AIDS.
Vaccination against HBV is important for healthcare providers. In the current study, more than 30% of nurses do not know about HBV vaccinations in contrast to a lower percentage (20%) of nurses in a similar study from Palestine [24]. This reflects poor national hospital policies to implement compulsory vaccination for employed nurses to prevent them from being infected by Bloodborne pathogens. As we are aware of the dangers of contaminated needles and the deadly diseases they can transmit. In our study, less than 40% of nurses knew about needle safety even though needle pricks are one of the significant modes of transmitting hepatitis B and C in the world. In contrast to studies conducted by Labrangue LJ, Rheajane AR, and Tizon MM. where this ratio is much higher 85% [25]. Nurses often sustain needle stick and sharp object injuries during clinical practice as is evident from other studies. Efforts are needed to correct unacceptable nurses ‘performance, especially when the mismatch between knowledge and practice is witnessed. In the current study, there was no significant correlation between knowledge and practice. However, a statistically significant positive correlation was found between knowledge and practice in the other studies' findings that reflect the better performance of nurses based on their knowledge. This contradictory finding might be explained by the lack of adherence to IC practices because of the absence of supervision and corrective actions [26-39].
Conclusion
Both the knowledge and the practices of nurses working in the selected Ayub teaching Hospital in terms of Blood borne disease measures were fair. In our study, about 70% of nurses have reasonable knowledge about blood-borne infections. But 30% have inadequate knowledge about these infections. Some nurses in the hospital refused to participate in the study because of their fear of situation assessment; an attitude that needs to assure patient and healthcare workers' safety. They do not know about the mode of transmission of these viruses. These sources, risk factors, vaccination, and treatment. There is a great risk of getting bloodborne infections from these nurses the infected patients.
Recommendation
Healthcare facilities should focus on increasing nurses’ awareness of strict adherence to Infection Control standards and implement training and preventive programs to minimize the risk of needlestick injuries. All nurses should be vaccinated against HBV. It is recommended to implement educational, highly structured informative inservice programs aiming at Nurses' education about blood-borne infections. This should be followed by post-training evaluations to assess the outcome and level of practice of Healthcare Workers based on their knowledge before and after the training intervention. All Healthcare workers should be encouraged to seek vaccination against HBV to reduce the risk of its sequel recommendations.
References
- Bloodborne Pathogens and Needlestick Prevention.
- Maltezou HC et al. Strategies to increase influenza vaccine uptake among health care workers in Greece. Scand J Infect Dis.40(3):266-68(2008).
- Bagheri NS, Allegranzi B, Syed SB, et al. Healthcare associated infection in Africa: a systematic review. Bull World Health Organ.89:757-65(2011).
- World Health Organization. The first global patient safety challenge: ‘Clean care is safer
care’.Geneva,Switzerland:WHO. - El-Zanaty Fa and Way A. Egypt demographic and health survey 2008. Egyptian: Ministry of Health. Cairo: El-Zanaty and Associates, and Macro International. (2009).
[Google Scholar] [Crossref]
- Kane A, Lloyd J, Zaflran M, et al. Transmission of hepatitis B, hepatitis C and human immunodeficiency viruses through unsafe injections in the developing world: model-based regional estimates. Bull World Health Organ. 77(10):801-07(1999).
[Google Scholar] [Crossref]
- Ahmad K. Hepatitis B in: Viral Hepatitis: An overview: proceedings of seminar, AFIP Rawalpindi, Pakistan. (l998).
[Google Scholar] [Crossref]
- World Health Organization. The World Health Report, Box 44. Geneva, Switzerland: World Health Organization. (2002). [Google Scholar] [Crossref]
- Shriyan A, Annamma RR. Incidence of occupational exposures in a tertiary healthcare centre. Indian J Sex Transm Dis. 33(2):91-7(2008).
- Boualle'gue O, Naija W, Said H, et al. P233: incidence of ICU acquired nososcomial infections in university hospital of sahloul (Sousse-Tunisia). Antimicrob. Resist Infect Control. 2:233(2013).
[Google Scholar] [Crossref]
- Cole M. Infection control: world’s apart primary and secondary care. Br J Community Nurs.12:301(2007).
- World Health Organization. The world health report 2002: reducing risks, promoting healthy life. World Health Organization: (2002).
[Google Scholar] [Crossref]
- Garner JS. Guideline for isolation precautions in hospitals. Infect Control Hosp Epidemiol. 17(1):53-80(1996).
- Siegel JD, Rhinehart E, Jackson M, et al. The healthcare infection control practices advisory committee, 2007. Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings.
[Google Scholar] [Crossref]
- Stein AD, Makarawo TP, Ahmad MF. A survey of doctors’ and nurses’knowledge, attitudes and compliance with infection control guidelines in Birmingham teaching hospitals. J Hosp Infect. 54(1):68-73(2003).
- Hanafi MI, Mohamed AM, Kassem MS, et al. Needlestick injuries among health care workers of University of Alexandria Hospitals. East Mediterr Health J.17(1):26-35(2011).
[Google Scholar] [Crossref]
- Enein EA, Younis N, M El, et al. Standard precautions: a KAP study among nurses in the dialysis unit in a University Hospital in Alexandria, Egypt. J Egypt Public Health Assoc.86(1-2):3-10(2011).
- Eskander HG, Youssef W, Morsy M, et al. Intensive care nurses’ knowledge & practices regarding infection control standard precautions at a selected Egyptian Cancer Hospital. J Educ Pract. 4:160-74(2013).
[Google Scholar] [Crossref]
- NA Ismail, AM AF, WH El. Safe injection practice among healthcare workers, Gharbiya, Egypt. J Egypt Public Health Assoc. 80:563-83(2005).
[Google Scholar] [Crossref]
- Gounden YP, Moodley J. Exposure to human deficiency virus among healthcare workers in South Africa. Int J Gynaecol Obstet. 69:265-70(2000).
- Mujeeb SA. Unsafe injections: a potential source of HCV spread in Pakistan. J Pak MED Assoc.51: 1-3(2001).
[Google Scholar] [Crossref]
- Johnson OE, Asuzu MC, Adebiyi AD. Knowledge and practice of universal precautions among professionals in public and private health facilities in Uyo, Southern Nigeria: a comparative study. Ibom Med J. 6:9-19(2013).
[Google Scholar] [Crossref]
- Vaz K, McGrowder D, Alexander-Lindo R, et al. Knowledge, awareness and compliance with universal precautions among health care workers at the University Hospital of the West Indies, Jamaica. Int J Occup Environ Med. 1:171-81(2010).
[Google Scholar] [Crossref]
- Fashafsheh I, Ayed A, Eqtait F, et al. Knowledge and practice of nursing staff towards infection control measures in the Palestinian Hospitals. J Educ Pract. 6(4):79-90(2015).
[Google Scholar] [Crossref]
- Labrangue LJ, Rheajane AR, Tizon MM. Knowledge of and compliance with standard precautions among student nurses. IJ ANS. 1:84-97(2010).
[Google Scholar] [Crossref]
- Qayyum S, Sattar A, Waqas B. Hospital acquired infections: knowledge about it and its prevention. Professional Med J. 17:168-73(2010).
- Abdulraheem IS, Amodu MO, Saka MJ, et al. Knowledge, awareness and compliance with standard precautions among health workers in North Easteam Nigeria. J Community Med Health Edu. 2:131(2012 )
- Isara AR, Ofili AN. Knowledge and practice of standard precautions amonghealthcare workers in the Federal Medical Centre, Asaba, Delta State, Nigeria. Niger Postgrad Med J. 17(3):204-09(2010).
[Google Scholar] [Crossref]
- Talaat E, Shamia E. Developing a control action plan for infection prevention at the endoscopy unit. J Int Acad Res.2:412-20(2010).
[Google Scholar] [Crossref]
- Uti OG, Agbelusi GA, Jeboda SO, et al. Infection control knowledge and practices related to HIV among Nigerian dentists. J Infect Dev Ctries. 3(8):604-10(2009).
- Agaral M, Thomas P. Prevalence of post op nosocomial infection in neuro surgical patients and associated risk factors-a prospective study. NJI. 94(2):620-25(2003).
[Google Scholar] [Crossref]
- Galal YS, Labib JR, Abouelhamd WA. Impact of an infection-control program on nurses’ knowledge and attitude in pediatric intensive care units at Cairo University hospitals. J Egypt Public Health Assoc. 89(1):22-8(2014).
- Elhoseeny TA, Mourad JK. Assessment of the safety of injection practices and injection-related procedures in family health units and centers in Alexandria. J Egypt Public Health Assoc. 89(2):66-73(2014).
- Kim PW, Roghmann MC, Perencevich EN, et al. Rates of hand disinfection associated with glove use, patient isolation, and changes between exposure to various body sites. Am J Infect Control. 31(2):97-103(2003).
- Gould D. Nurses’ hand decontamination practice: results of a local study. J Hosp Infect. 28(1):15-30(1994).
- Mahmud N, Abdul Sahib S. Assessment of nurses’ practices toward infection control standardized precautions in Azady Teaching hospital in the city of Kirkuk. Iraqi Natl J Nurs Spec. 24:52-8(2011).
[Google Scholar] [Crossref]
- Hamid MZ, Aziz NA, Anita AR, et al. Knowledge of blood-borne infectious diseases and the practice of universal precautions amongst healthcare workers in a tertiary hospital in Malaysia. Southeast Asian J Tropm Med Public Health. 41:1192-99(2010).
[Google Scholar] [Crossref]
- Gijare M. Effectiveness of teaching on infection control practices among health care professionals. Sinhgad J Nurs. 2:5-9(2012).
[Google Scholar] [Crossref]
- Ndikom CM, Onibokun A. Knowledge and behavior of nurses/midwives in the prevention of vertical transmission of HIV in Owerri, Imo, Nigeria: a cross sectional study. J Biomed Cent Nursing.1:1-9 (2007).
[Google Scholar] [Crossref]