Review Article - Interventional Cardiology (2010) Volume 2, Issue 1
Management of restenosis after drug-eluting stent placement for unprotected left main disease
- Corresponding Author:
- Imad Sheiban
University of Turin, Division of Interventional Cardiology
Tel: +39 11 633 6026
Fax: +39 11 633 5572
E-mail: isheiban@yahoo.com
Abstract
Keywords
angioplasty, drug-eluting stent, restenosis, stenting, ULMCA, unprotected left main
Since the late 1970s coronary artery bypass grafting (CABG) has traditionally been considered the reference treatment for left main coronary artery disease [1,2]. Percutaneous coronary intervention (PCI) for unprotected left main (ULM) disease was first attempted by Andreas Gruntzig as early as 1977 using experimental balloon angioplasty catheters. The risk of elastic recoil was soon recognized to be a major obstacle in this segment of vital importance [3,4]. The introduction of bare-metal stents (BMS) provided important immediate and mid-term results by reducing peri-procedural risks (e.g., the need for emergency CABG), restenosis and target lesion failure. Nonetheless, intrastent proliferation limited BMS benefits with the ensuing risk of target lesion revascularization (TLR) [5,6]. Drug-eluting stents (DES) have been shown to significantly reduce the risk of restenosis and, in some institutions, it has become common practice to implant DES in the ULM [7–9]. In the last few years we have witnessed constant improvements in medical approaches to coronary artery disease (e.g., new therapies for diabetes and dyslipidemia) along with the development of new technologies by the medical industry (e.g., stent platforms and polymers). Despite these improvements, DES restenosis in the ULM is an emerging problem for interventionalists. If we consider that restenosis in such a delicate location may produce severe myocardial ischemia, the treatment of such lesions may influence patient prognosis. ULM restenosis management is thus an intriguing challenge for interventional cardiologists. The aim of this review is to summarize the state of the art in this particular field of research and to describe the outcome and optimal management of such patients to date.
Incidence & prevalence of ULM restenosis
Unprotected left main restenosis rates have been described in many randomized and retrospective studies investigating thousands of subjects, thus demonstrating the progressive diffusion of the percutaneous approach in this segment. It has been shown that after 15 months of clinical follow-up, significant intra-stent proliferation is present in up to 16% of subjects, 7% of whom require target vessel revascularization (TVR) [10]. In the scientifically rigorous and randomized SYNTAX trial, 12‑month major adverse cardiac event (MACE) rates reached 17.8% with repeat revascularization rates of 13.7% [11]. A recent meta-analysis including 1278 patients undergoing PCI with DES in ULM shows similar results, thus confirming the importance of the phenomenon [12]. When a systematic angiographic followup was performed, in-lesion restenosis is present in up to 42% of patients (median follow-up: 276 ± 57 days), with TVR rates of up to 38%. We also demonstrated that TLR was ischemia‑driven in only 14% of patients.
When analyzing the localization of restenosis, late loss was significantly greater within the left circumflex ostium compared with the parent vessel of the left main coronary artery bifurcation. As expected, late loss continued to increase between 3- and 9-months followup [13]. Mehilli et al. recently reported on the efficacy of paclitaxel-eluting stents (PES) and sirolimus-eluting stents (SES) in the prevention of ULM restenosis [14]. In this randomized study, 607 patients with symptomatic coronary artery disease undergoing PCI for ULM were randomized to receive a PES or SES. Angiographic restenosis was 16.0% with PES and 19.4% with SES (RR: 0.82; 95% CI: 0.57–1.19; p = 0.30), thus concluding that both of these DES provided comparable clinical and angiographic outcomes.
The Failure In Left Main Study (FAILS) was the first ever evaluating the epidemiology of ULM restenosis and its best treatment [15]. Despite small numbers and a retrospective design, the FAILS provided original details regarding the presentation of such patients. Almost 70% of them were elective angiographic controls or presented with silent ischemia or stable angina. However, an unstable presentation was present in over 30% of cases, suggesting that restenosis is not a benign entity even in the ULM.
Predictors of ULM restenosis
Several clinical studies identified the predictors of adverse events in patients undergoing ULM stenting with DES. On univariate analysis, Parsonnet classification of surgical risk, use of intra-aortic balloon pump, presence of shock at entry, lesion located in the distal LM, nonelective PCI, troponin elevation at entry, thrombolysis in myocardial infarction flow grade before and after PCI, reference vessel diameter, left ventricular ejection fraction and the use of DES were recognized as significant predictors of adverse events. On multivariate analysis, Parsonnet classification, troponin elevation at entry, lesions located at a distal site, reference vessel diameter and the use of DES were independent predictors of major adverse cardiovascular events [16]. Multiple metaanalyses have shown that bifurcational disease, multivessel and double-vessel stenting are also important covariates of adverse outcomes.
While data regarding the predictors of restenosis in ULM are rather limited, many authors have described those in all coronary lesions [17–20]. Further studies will be useful in order to better asseses which are the characteristics that lead to a relapse of disease in such a delicate localization.
Diagnostic appraisal
Both Price et al. [13] and Palmerini et al. warned that restenosis was frequently asymptomatic, thus recommending serial angiographic follow- up. This view was reiterated by Baim et al. who cautioned: “Without that safety net, one would expect an up-tick in late mortality events resulting from unrecognized restenosis in this critical location”. A critical ULM stenosis needs immediate diagnosis and therapy because of poor prognosis due to significant decrease of myocardial perfusion.
Clinical and instrumental data may be helpful in order to identify patients with a critical ULM restenosis. Coronary angiography has been universally accepted as the gold standard for the quantification of coronary artery disease. A significant ULM restenosis is defined as a stenosis of greater than 50% at coronary angiography. It leads to a poor prognosis at long-term follow-up. The prognosis of patients with mild-to-moderate (<50% diameter stenosis) ULM narrowing is still unknown [19].
Ostial lesions as well as bifurcational lesions involving the proximal left anterior descending or circumflex, may be difficult to assess angiographically. Intravascular ultrasound permits detailed, high-quality, cross-sectional imaging of coronary arteries and therefore should be considered in the assessment of patients with angiographically ambiguous or inconclusive ULM disease.
Multislice computed tomography (MSCT) is a promising technique for noninvasive coronary evaluation. Current MSCT technology, in combination with optimal heart rate control, allows reliable noninvasive evaluation of selected patients after ULM stenting. The literature suggests that MSCT is safe to exclude left main intrastent restenosis and therefore might be an acceptable diagnostic alternative in future [21].
Medical management
The treatment of ULM restenosis is based on patient symptoms/signs of ischemia, coronary anatomy, surgical risk, PCI feasibility and overall life expectancy. Considering that the natural history of restenosis is far more malignant than stable coronary disease, such patients should be treated more aggressively. Isolated medical therapy (MT) should be reserved for high-risk patients ineligible for revascularization. The demonstration of a fractional flow reserve greater than 0.80 is another indication for MT alone. Improvements in MT have benefited both surgical and medical groups, but in view of the overall survival advantage of CABG in most angiographic and clinical subsets, current American College of Cardiology/American Heart Association guidelines state: “the benefit of surgery over medical treatment in patients with significant ULM stenosis”. The benefits of CABG compared with MT emerge beyond 1 year, as perioperative mortality and morbidity in the CABG group become offset by mortality from coronary artery disease in the medical group. However CABG and PCI, together with MT, reduce morbidity and mortality and improve quality of life.
Lifestyle changes can reduce cardiovascular risk factors, improve quality of life, and lower cardiovascular morbidity and mortality. They provide additional benefit over and above MT and/or revascularization procedures and should be strongly recommended to all patients.
The MT of ULM restenosis consists of:
▪ Aspirin and antianginals: platelets antiaggregant agent (acetylsalicylic acid [75–325 mg/day], and/or thienopyridines [clopidogrel/ticlopidine]) and nitrates;
▪ b-blockers and blood pressure control (target <130/80 mmHg): b-blockers (resting heart rate: target 55–60/min), angiotensin-converting enzyme inhibitors in diabetics or patients with impaired left ventricular systolic function and should also be considered in all patients with vascular disease and at least high normal blood pressures, calcium-channel blockers;
▪ Cholesterol management and cigarette cessation: lipid-lowering agents such as statins (to achieve an low-density lipoprotein <100 mg/dl);
▪ Dietary improvements and diabetes control (good glycemic control with glycohemoglobin <7.0%);
▪ Education and exercise.
In the FAILS, MT was reserved to a very limited cluster of patients. Only four subjects were considered ineligible for both surgery and PCI, considering their prohibitive risk profile (i.e., age, diabetes, renal insufficiency, other comorbidities, etc.). Mid-term outcome of the isolated MT was obviously very poor, including cardiac death (25%) and a ULM TLR (25%) at 2 years follow-up.
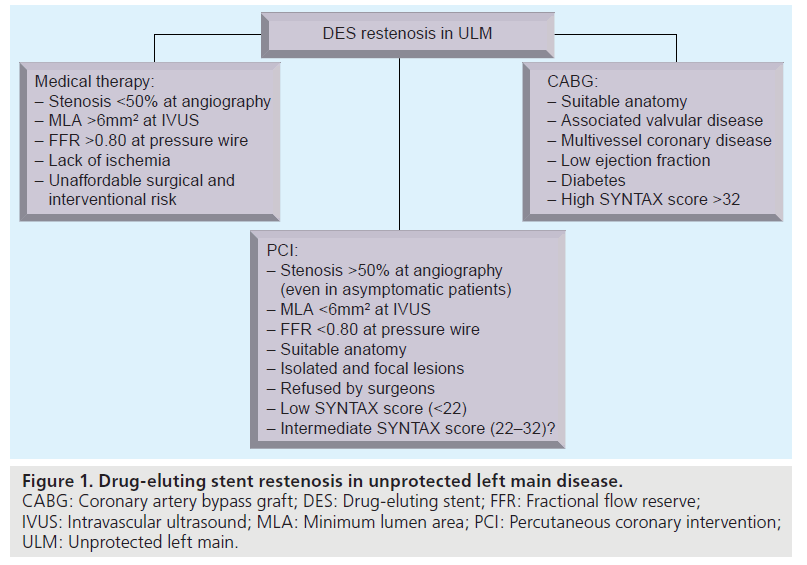
To date, several trials have demonstrated a survival benefit in patients treated by means of CABG or PCI over MT. According to recent guidelines the current standard of care for treatment of ULM stenosis is CABG. However, the strategy of revascularization (CABG or PCI) and MT should be viewed as complementary, rather than opposing, strategies. Indeed, considering the prognostic relevance of ULM disease, our opinion is that MT alone should be offered only when revascularization is strictly contraindicated (Figure 1).
Percutaneous management
Unprotected left main restenosis can often be managed by means of PCI. The decision to perform PCI instead of surgery is usually considered in the following conditions:
▪ Unsuitable anatomy for surgery (size and quality of coronary vessels and/or conduits for grafting);
▪ Suitable anatomy for stenting;
▪ Increased risk for surgery (comorbidities, age and EUROscore);
▪ Absence of significant valvular disease requiring surgery;
▪ Preference by the patient for a percutaneous approach.
An accurate angiography with the standard projections is required to asses the exact localization of disease (ostium, shaft or bifurcation). The images also reveal the pattern of restenosis (focal, diffuse or proliferative). PCI can be performed with balloon angioplasty (conventional or drug-eluting balloons) or with stent implantation. While a BMS intra-DES is a very rare occurrence, a second DES placement is a more frequent technique. A rare approach to ULM restenosis is the use of debulking devices such as cutting balloon or coronary atherectomy. Such devices may be indicated in the case of calcified lesions. PCI has to be associated with optimal MT in order to maximize the benefits. In the literature there is no data regarding the optimal duration of double antiplatelet therapy after DES placement for a ULM restenosis. Considering the critical localization of disease, stent thrombosis would be a sudden catastrophic event. It appears prudent to err on the side of prolonging thienopyridines (in the absence of bleeding) until there is good evidence supporting shorter duration of therapy. The choice between angiographic and clinical follow-up should be left at the operator’s and referring physician’s discretion, but often takes into account patient’s preference and comorbidities. Currently there is no evidence that a systematic angiographic follow-up improves patient prognosis. Nonetheless, in most cases, angiographic follow-up is recommended irrespective of symptoms or signs of ischemia 6–12 months after index PCI.
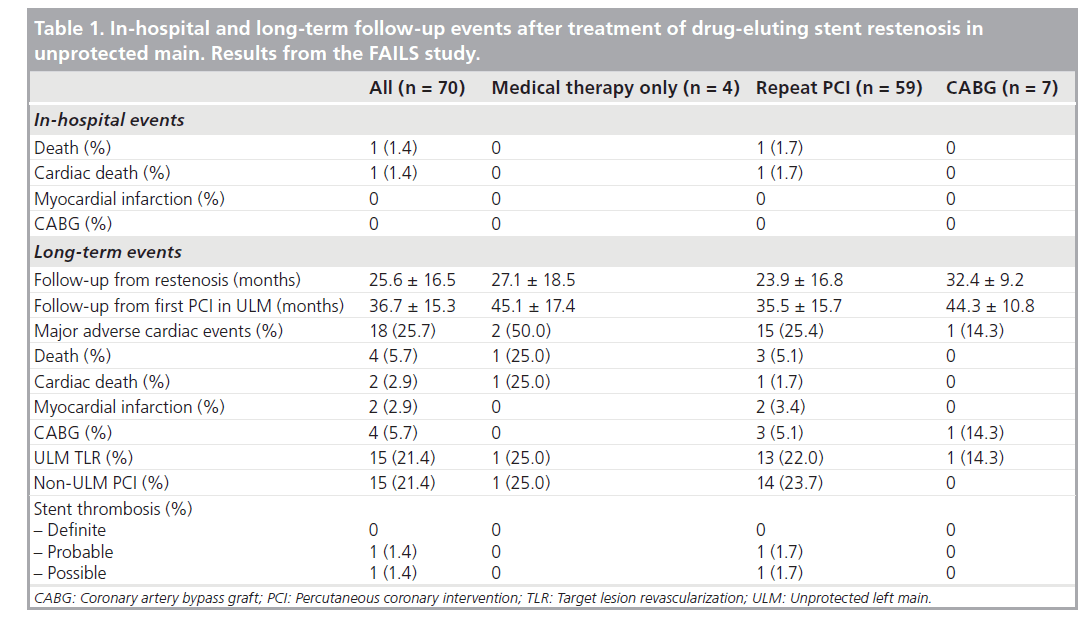
To date there are very few data regarding the interventional approach to DES restenosis in ULM. The FAILS study retrospectively enrolled 70 patients presenting with significant angiographic restenosis [15]. These subjects were identified from a total sample of 718 patients with ULM treated with DES. The primary end point was the long-term rate of MACE such as death, myocardial infarction (MI) or TLR. Of the overall population, 5% died before 6 months without any angiographic followup (2.5% suddenly). Angiographic follow-up was ultimately performed in 62.8% subjects, being clinically driven in 16.6% and routinely performed even in the absence of symptoms/ signs of myocardial ischemia in 46.2%. The 70 restenotic cases were treated by means of MT only (5.7%), repeat PCI (84.3%) and CABG (10%). Among the 59 patients treated interventionally (repeat PCI group), 57.6% underwent a new DES implantation. In contrast to the previous baseline procedure, PES were used predominantly, followed by SES. The immediate outcome was quite favorable (Table 1), with one (1.7%) death in the PCI group. No patient had periprocedural MI or needed urgent CABG. Long-term follow-up data were available in 100% of restenotic subjects after an average of 25.6 ± 16.5 months since diagnosis of restenosis (36.7 ± 15.3 months of follow-up from the first PCI with DES in the ULM), with 44.3% of subjects undergoing repeat PCI having repeat angiographic follow-up after 8.1 ± 8.3 months. The MACE rate was 25.7%, with death in 5.7%, MI in 2.9%, TLR in 21.4% (including CABG in 5.7%) and PCI on other vessels in 21.4%. Finally, one case of possible stent thrombosis, one of probable stent thrombosis and no cases of definite stent thrombosis were identified. The major findings of the FAILS were twofold:
▪ Significant ULM DES restenosis is often characterized by a stable clinical condition;
▪ After 24 months of clinical follow-up from the diagnosis of restenosis, MACE rates appear quite favorable in both the interventional and surgical therapy groups.
Almost 70% of patients with a diagnosis of significant DES restenosis in ULM were elective angiographic controls or presented with silent ischemia or stable angina, but an unstable presentation of ULM restenosis was found in over 30% of cases, suggesting that restenosis is not a benign entity even in the ULM. Nonetheless, repeat PCI is often possible and successful in these subjects. Notably, paclitaxel- eluting stents were used more frequently for repeat PCI, possibly because of availability subsequent to SES, larger sizes and preference for different DES strategy [8]. Regarding the mid-term clinical outcome (>2 years of median follow-up after the diagnosis of restenosis), this study showed low mortality and MI rates in patients treated with PCI and CABG. Differences in MACE, death, MI and TLR rates between these two groups are, however, limited by the small size of the CABG group, and should be viewed as hypothesis-generating only. It should also be borne in mind that follow- up intervention results are largely dependent on the initial patient characteristics and interventional approach, as, for instance, in the FAILS multiple stents were commonly implanted, limiting the role of subsequent CABG.
The interventional approach to restenosis after DES placement in left main stem is technically feasible and safe. Despite encouraging immediate and mid-term results supplementary data from larger trials are definitely required.
Surgical management
To date, few data are available about the surgical management of DES restenosis in ULM. For coronary artery disease with ULM stenosis, CABG is traditionally regarded as the “standard of care” due to well-documented evidence, from meta-analysis of randomized trials and registry data, of durable survival advantage, despite an increasing trend to use DES for ULM stenosis.
Surgical management of ULM restenosis should be considered in the following conditions:
▪ Suitable coronary anatomy
▪ Diabetic patients
▪ Concomitant multivessel disease
▪ Low left ventricular ejection fraction
▪ Valvular disease requiring surgery
▪ Acceptable surgical risk and overall life expectancy
Gorlin first reported that CABG resulted in a significant improvement in 10‑year survival compared with MT in patients with significant ULM stenosis, an observation confirmed in three randomized trials and numerous observational studies over the next two decades. Although both the MT and surgical techniques used in these studies are outdated by today’s standards (e.g., aspirin, statins and internal mammary artery [IMA] grafts were not widely used), a meta-analysis of these trials demonstrated a significant relative risk reduction in mortality with CABG of approximately 66% at 5 years with the benefit extending to 10 years. Even so, the trials probably underestimated the real survival benefit of CABG surgery because the trial patients were relatively low risk, only 10% of surgical patients received an IMA graft (which leads to superior long-term graft patency and a clear survival benefit), and analysis on an intention-to-treat basis ‘discounted’ the survival advantage of CABG in the 40% of the medical group who crossed over to surgery. Indeed, in the prospective study of ULM stenosis, in which 1484 patients in the Coronary Artery Surgery Study (CASS) registry were followed for up to 16 years, the overall median survival for CABG patients was 13.3 years versus 6.6 years for MT. Since these pivotal studies, improvements in MT have benefited both surgical and medical groups, but in view of the overall survival advantage of CABG in most angiographic and clinical subsets.
In the last decade, six groups from Europe and the USA have reported CABG results in cohorts of at least 300 patients with ULM stenosis. Cumulatively, these studies included almost 11,000 patients of whom around a third (range: 5–57%) underwent urgent surgery with an average in-hospital mortality of 2.8% and 30‑day mortality of 3–4%. In the SYNTAX trial [12], 12‑month MACE rates reached 17.8% in the PCI group and 12.1% in the CABG group, with repeat revascularization rates of 13.7 and 5.9%. Moreover, Seung et al. compared in a nonrandomized fashion PCI versus CABG and found that after 33 months they did not differ significantly for death rates or the composite of death, MI or stroke. However, DES were associated with higher rates of TLR (9.7 vs 1.6%). Similar results were also reported by other authors. Despite their inherent limitations, the results of ongoing trials with randomized and registry cohorts evaluating DES with CABG should provide evidence-based guidance in selecting the preferred form of treatment for ULM stenosis in the future.
Recently, the FAILS reported on seven patients treated by means of surgery for significant ULM restenosis [15]. Patients undergoing surgery were significantly older (69.7 ± 8.9 vs 64.8 ± 12.7 years) and had lower ventricular ejection fraction (45.0 ± 7.1% vs 53.9 ± 9.5%). However, there were no diabetic subjects (0 vs 31% in the PCI group) and EUROscore was significantly lower (5.0 ± 1.9 vs 7.1 ± 13). At 27 months after the restenosis diagnosis, MACE rates were 14.3 versus 25.4%, respectively. Cardiac death, MI and ULM TLR were respectively 0 versus 1.7%, 0 versus 3.4% and 14.3 versus 22%.
Outcomes of repeat PCI for ULM restenosis are not well defined. Every single case should be collegially discussed between surgeons and interventionalists. However, it is reasonable to recommend CABG, in the absence of contraindications to surgery, as standard of care for most patients with ULM stenosis because of its substantial survival advantage and freedom from repeat intervention. PCI is a reasonable alternative in subjects presenting isolated ULM stenosis or who are ineligible for CABG.
Conclusion & future perspective
Restenosis after DES placement in the ULM has become an intriguing challenge for interventionalists. Although current guidelines recommend a surgical approach to ULM, in the last few years it has been demonstrated that PCI is safe and feasible, with similar shortand mid-term survival and MI rates. However, recurrent revascularizations are still a major issue. To date there is a substantial lack of data in the literature regarding the optimal management of DES restenosis in ULM. There is only a multicentric retrospective study, the FAILS, describing the outcome of 70 restenotic cases over more than 700 patients that had a DES implanted in the left main stem. After 24 months of clinical follow-up from the diagnosis of restenosis, MACE rates appeared quite favorable in the interventional group. Surgery should be reserved for patients presenting concomitant multivessel disease, valvular disease, low ejection fraction, diabetes and suitable anatomy for grafting. Finally, it has been demonstrated that optimal MT should be associated with a revascularization strategy in order to provide significant benefits in the treatment of DES restenosis in ULM. Our opinion is that in the next 5–10 years ULM restenosis will be managed more and more frequently by the means of interventional cardiology. PCI outcomes will improve along with the development of new technologies (e.g., stent platforms and polymers) and the optimization of MT.
Executive summary
▪ Drug-eluting stent (DES) restenosis in the unprotected left main (ULM) is an emerging problem for interventionalists.
▪ When a systematic angiographic follow-up is performed, in-lesion restenosis is present in up to 42% of patients with target vessel revascularization rates of up to 38% (median follow-up: 276 ± 57 days).
▪ Almost 70% of ULM restenosis were elective angiographic controls or presented with silent ischemia or stable angina. Acute coronary syndrome (unstable angina, ST-segment elevation myocardial infarction [STEMI] or non-STEMI) was the admission diagnosis in over 30% of cases.
▪ Parsonnet classification, troponin elevation at entry, bifurcational disease, reference vessel diameter, multivessel and double-vessel stenting and the use of DES were independent predictors of major adverse cardiac events.
▪ The treatment of ULM restenosis is based on patient symptoms/signs of ischemia, coronary anatomy, surgical risk, percutaneous coronary intervention (PCI) feasibility and overall life expectancy.
▪ Revascularization and medical therapy should be viewed as complementary, rather than opposing, strategies. Considering the prognostic relevance of ULM disease, medical therapy alone should only be offered when PCI or coronary artery bypass graft (CABG) are strictly contraindicated.
▪ PCI is indicated in the following conditions: unsuitable anatomy for surgery (size and quality of coronary vessels and/or conduits for grafting), increased risk for surgery (comorbidities, age and EUROscore), suitable anatomy for stenting, absence of significant valvular disease requiring surgery and/or preference by the patient for a percutaneous approach.
▪ CABG is indicated in the following conditions: suitable coronary anatomy, diabetic patients, concomitant multivessel disease, low left ventricular ejection fraction, valvular disease requiring surgery and/or acceptable surgical risk.
▪ Outcomes of repeat PCI for ULM restenosis are not well defined (lack of evidence). Every single case should be collegially discussed between surgeons and interventionalists.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Chaitman BR, Fisher LD, Bourassa MGet al.: Effect of coronary bypass surgery onsurvival patterns in patients with left maincoronary artery disease. Report of theCollaborative Study in Coronary ArterySurgery (CASS). Am. J. Cardiol. 48, 765–777(1981).
- Yusuf S, Zucker D, Peduzzi P et al.: Effect ofcoronary artery bypass graft surgery onsurvival: overview of 10‑year results fromrandomised trials by the Coronary ArteryBypass Graft Surgery Trialists Collaboration.Lancet 344, 563–570 (1994).
- Meier B: The first coronary angioplasties inZurich. In: The Evolution of CardiacCatheterization and Interventional Cardiology.Bertrand M (Ed.). Iatric Press, St Albans,UK, 61–74 (2006).
- O’Keefe JH Jr, Hartzler GO, Rutherford BDet al.: Left main coronary angioplasty: earlyand late results of 127 acute and electiveprocedures. Am. J. Cardiol. 64, 144–147(1989).
- Tan WA, Tamai H, Park SJ et al.; for theULTIMA Investigators: Long-term clinicaloutcomes after unprotected left main trunkpercutaneous revascularization in 279 patients.Circulation 104, 1609–1614 (2001).
- Takagi T, Stankovic G, Finci L et al.: Resultsand long-term predictors of adverse clinicalevents after elective percutaneousinterventions on unprotected left maincoronary artery. Circulation 106, 698–702(2002).
- Park SJ, Kim YH, Lee BK et al.: Sirolimuselutingstent implantation for unprotected leftmain coronary artery stenosis: comparisonwith bare metal stent implantation. J. Am.Coll. Cardiol. 45(3), 351–356 (2005).
- Chieffo A, Stankovic G, Bonizzoni E et al.:Early and mid-term results of drug elutingstent implantation in unprotected left main.Circulation 111, 791–795 (2005).
- Sheiban I, Meliga E, Moretti C et al.:Long-term clinical and angiographicoutcomes of treatment of unprotected leftmain coronary artery stenosis with sirolimuselutingstents. Am. J. Cardiol. 100, 431–435(2007).
- Gao RL, Xu B, Chen JL et al.: Immediate andlong-term outcomes of drug-eluting stentimplantation for unprotected left maincoronary artery disease: comparison withbare-metal stent implantation. Am. Heart J.155(3), 553–561 (2008).
- Serruys PW, Morice MC, Kappetein AP et al.;for the SYNTAX Investigators: Percutaneouscoronary intervention versus coronary-arterybypass grafting for severe coronary arterydisease. N. Engl. J. Med. 360, 961–972 (2009).
- Biondi-Zoccai GG, Lotrionte M, Moretti Cet al.: A collaborative systematic review andmeta-analysison 1278 patients undergoingpercutaneous drug-eluting stenting forunprotected left main coronary artery disease.Am. Heart J. 155(2), 274–283 (2008).
- Price MJ, Cristea E, Sawhney N et al.:Serial angiographic follow-up of sirolimuselutingstents for unprotected left maincoronary artery revascularization. J. Am. Coll.Cardiol. 47(4), 871–877 (2006).
- Mehilli J, Kastrati A, Byrne RA et al.:LEFT-MAIN Intracoronary Stenting andAngiographic Results: drug-eluting stents forunprotected coronary left main lesions studyinvestigators. Paclitaxel- versus sirolimuselutingstents for unprotected left maincoronary artery disease. J. Am. Coll. Cardiol.53(19), 1760–1768 (2009).
- Sheiban I, Sillano D, Biondi-Zoccai Get al.: Incidence and management ofrestenosis after treatment of unprotected leftmain disease with drug-eluting stents:70 restenotic cases from a cohort of 718patients. The Failure In Left Main Study(FAILS). J. Am. Coll. Cardiol. 54(13),1131–1136 (2009).
- Valgimigli M, van Mieghem CA, Ong ATet al.: Short- and long-term clinical outcomeafter drug-eluting stent implantation for the percutaneous treatment of left main coronaryartery disease: insights from the Rapamycin-Eluting and Taxus Stent Evaluated AtRotterdam Cardiology Hospital registries(RESEARCH and T-SEARCH). Circulation111(11), 1383–1389 (2005).
- Lee CW, Park DW, Lee BK et al.: Predictorsof restenosis after placement of drug-elutingstents in one or more coronary arteries. Am. J.Cardiol. 97(4), 506–511 (2006).
- Kastrati A, Dibra A, Mehilli J et al.: Predictivefactors of restenosis after coronary implantationof sirolimus- or paclitaxel-eluting stents.Circulation 113(19), 2293–2300 (2006).
- Park SJ, Hong MK, Lee CW et al.: Electivestenting of unprotected left main coronaryartery stenosis: effect of debulking beforestenting and intravascular ultrasoundguidance. J. Am. Coll. Cardiol. 38, 1054–1060(2001).
- Lee RJ, Shih KN, Lee SH et al.: Predictors oflong-term outcomes in patients after electivestent implantation for unprotected left maincoronary artery disease. Heart Vessels 22(2),99–103 (2007).
- Van Mieghem CA, Cademartiti F, Mollet NRet al.: Multislice spiral computed tomographyfor the evaluation of stent patency after leftmain coronary artery stenting: a comparisonwith conventional coronary angiography andintravascular ultrasound. Circulation 114(7),616–619 (2006).
▪ The SYNTAX study provides very important informations on patients with three-vessel disease or unprotected left main (ULM) stenosis, demonstrating that they can be treated successfully by means of percutaneous coronary intervention.
▪ Biondi-Zoccai et al. conduced a large meta-analysis providing important information about the outcome of patients undergoing ULM stenting.
▪ Systematic angiographic follow-up in patients undergoing ULM stenting showed higher restenosis and target lesion revascularization rates with unclear clinical meaning.
▪▪ The Failure In Left Main Study (FAILS) is the only registry evaluating the management of patients with significant drug-eluting stent restenosis in the ULM.