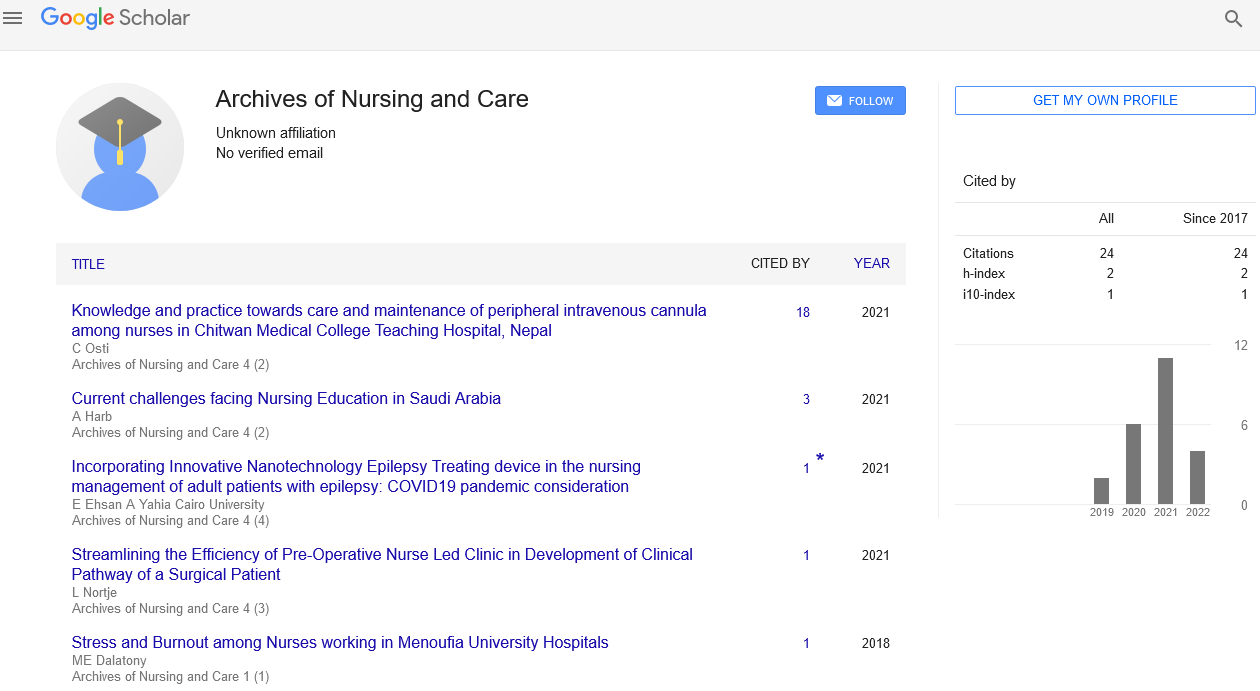
Short Communication - Archives of Nursing and Care (2022) Volume 5, Issue 9
Medical Decision Audit: Transmission of Data on Patients Entering French Nursing Homes with Dementia Does Not Confirm the Diagnosis
Norman Marcon*
Inserm U1219 Bordeaux Population Health Center, Université de Bordeaux, 33076, benin
Inserm U1219 Bordeaux Population Health Center, Université de Bordeaux, 33076, benin
E-mail: norm@kj.com
Received: 04-Dec-2022, Manuscript No. oanc-22-84048; Editor assigned: 06-Dec-2022, PreQC No. oanc-22-84048 (PQ); Reviewed: 20- Dec-2022, QC No. oanc-22-84048; Revised: 26-Dec-2022, Manuscript No. oanc-22-84048 (R); Published: 31-Dec-2022; DOI: 10.37532/ oanc.2022.5(9).109-111
Abstract
In France, there were 855.000 dementia patients. The patients in Lanmeur's rural hospital were a decent sample of those in French nursing homes. The follow-up was handled by neighbourhood general practitioners, as is common in France for nursing homes. The study looked at information that was sent when dementia patients were placed in institutions, including clinical and paraclinical information. Goal: To show that admission letters did indeed allow GPs to diagnose dementia. All dementia patients who were institutionalised were included. We looked for 25 criteria in the admission letters, which were drawn from the French guidelines for diagnosing dementia and Alzheimer's disease (multiple cross-sectional analysis per year). Results. Overall, there were 293 patients. The typical diagnostic tests used Conclusions are a necessary component of the letters of acceptance. The information in admission letters did not allow for the diagnosis of dementia by French standards. We are aware that dementia is underdiagnosed and undertreated in France in accordance with the same standards. What effects did a lack of fundamental knowledge have on the process of repeated diagnosis and the desire for treatment? This has to be evaluated.
Keywords
Medical Subject Headings (MeSH) • Tuberculosis (TB) infectiousness
Introduction
In France, there were 855 000 patients who had dementia. Most of them (40%) were in institutions. According to NINCDS-ADRDA (the National Institute of Neurological and Communicative Disorders and Stroke—Disease Alzheimer's and Related Disorders Association), ANAES (Agence nationale d'Accréditation et d'Evaluation en Santé: the National Agency of Accreditation and Evaluation in Health) guidelines since February 2000 [3] had 25 criteria for a positive and etiological diagnosis of dementia. In France, a geriatrician, psychiatrist, or neurologist was required to start a particular course of treatment. General Physicians then assumed follow-up. A first thorough neuropsychiatric evaluation was strongly advised in the primary phase of diagnosis by a specialist. Only one-third of patients in France received specific dementia therapy, despite there being many reasons for geriatricians. These significant signs and the number are at odds with one another. of particular therapies. Could this discrepancy be a result of general practitioners' practises? If so, what factors might they use to determine diagnoses Approach the population
Those who resided in Lanmeur's rural hospital made up the study's population. Their neighbourhood doctors took care of them.
This was a significant issue because the majority of those individuals had disabilities and required medical transportation for any more specialised testing. In each of those evaluations, doctors divided their attention equally between determining a diagnosis that might alter the course of treatment and the patient's comfort. All of this must be completed in a manner that is both timely and cost-effective for a rural hospital (which in France is primarily a nursing home) and morally and practically beneficial for the patients.
Study location
A 255-bed nursing facility serves as the rural hospital in Lanmeur. According to age, sex, and morbidity ratios, its population has been determined to be typical of nursing facilities in France. Two general hospitals are located nearby in Morlaix (15 km) and Lannion (25 km) as well as a university hospital in Brest (70 km) from Lanmeur.
Incorporation
As an antecedent or diagnosis, we did include all individuals with coded Alzheimer disease or other dementias in ICM 10.
Restrictions
Patients with incorrect coding (Alzheimer's and another kind of dementia in the same record), patients with deceptive coding (paper charts with a different diagnosis or antecedent than in a computerised record), and patients without admission letters were also excluded from the study (letter was considered lost if it was mentioned in the medical records and not found, otherwise we supposed that we had no admission letter). Records in the database were added or removed. The original letter was the only source from which the diagnosis criteria were all taken.
Results
In our database, there were 681 patients. 378 people had dementia when they entered. With 30 cases of Alzheimer's disease and 332 dementias without a known cause, 362 might be included. 69 of those 362 patients were disqualified due to incomplete records. This entails incorrect ICM 10 classification or different coding between manual files and computerised records (average 23.5%, maximum 37.5%, and minimum 20% per year), lost letters or patients without any letters. Less than 10% of the writings were personal and familial history. Only one case had a family history of Alzheimer's disease. Less than 10% of people described having mnestic problems. Evolution, related depression, and neurological clinic anomalies were each identified in 9%, 28%, and 24% of clinical tests, suggesting a diagnosis other than Alzheimer's disease. Scores were barely there; MMS, which was discovered at 11%, was nearly the only one. IADL and other specialty examinations were not administered. Hemoglobinemia (23%), and natremia (13%) were the only values above 10% by biological examination (which is particularly advised to rule out an organic aetiology of dementia). For 43%, specialised guidance was available. The average number of criteria in each message is Only one of the 25 was suggested by ANAES. The median number of criteria has evolved. There was no discernible difference between addressing practitioners or wards.
Conclusion
Despite a slight improvement, no thorough dementia diagnosis checkup was communicated from secondary care to general practitioners in France. When it did, the admission letters did not provide supporting documentation for the dementia diagnosis. With regard to our findings, various hypotheses can be made, including the following: hospitalists perform incomplete initial examinations; their practises do not align with recommended standards; vulnerable populations receive poor medical care (referred to as secondary care); and hospitalists and GPs rarely communicate. Additionally, GP management may face criticism for putting themselves in an uncomfortable situation by referring colleagues. In any case, from the patient's perspective, GPs avoided making this diagnosis in the absence of solid supporting data. What role does this play based on their intent to use particular drugs to treat them or not How does this affect fresh examinations performed for elderly and disabled people at excessive and unnecessary cost? We ought to discuss this subject using two studies: one on the GP's motive using a representative and Mulrow's decision model The GP's sample is to respond to the following questions: Will you continue an antidepressant medication if you experience side effects but lack proof that the diagnosis is reliable? The second study looked at discrepancies between secondary and primary care diagnoses on representative samples of dementia patients who had recently received a secondary care diagnosis and underwent a primary care checkup in accordance with French norms.
Acknowledgment
The author would like to acknowledge his Inserm U1219 Bordeaux Population Health Center, Université de Bordeaux, 33076, benin for their support during this work.
Conflicts of Interest
The author has no known conflicts of interested associated with this paper.
References
- Vukasinovic. Real Life impact of anesthesia strategy for mechanical thrombectomy on the delay, recanalization and outcome in acute ischemic stroke patients. J Neuroradiol. 95, 391-392 (2019).
- Salinet ASM. Do acute stroke patients develop hypocapnia? A systematic review and meta-analysis. J Neurol Sci. 15, 1005-1010 (2019).
- Jellish WS. General Anesthesia versus conscious sedation for the endovascular treatment of acute ischemic stroke. J Stroke Cerebrovasc Dis. 25, 338-341 (2015).
- Rasmussen M. The influence of blood pressure management on neurological outcome in endovascular therapy for acute ischaemic stroke. Br J Anaesth. 25, 338-341 (2018).
- Südfeld S.Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J Anaesth. 81, 525-530 (2017).
- Campbell BCV. Effect of general anesthesia on functional outcome in patients with anterior circulation ischemic stroke having endovascular thrombectomy versus standard care: a meta-analysis of individual patient’s data. Lancet Neurol. 41, 416-430 (2018).
- Wu L. General anesthesia vs local anesthesia during mechanical thrombectomy in acute ischemic stroke. J Neurol Sci. 41, 754-765 (2019).
- Goyal M. Endovascular thrombectomy after large vessel ischaemic stroke: a meta- analysis of individual patient data from five randomised trials. Lancet. 22, 416-430 (2016).
- Berkhemer OA.A randomized trial of intra-arterial treatment for acute ischemic stroke. N Engl J Med. 14, 473-478 (2015).
- Rodrigues FB.Endovascualar treatment versus medical care alone for ischemic stroke: a systemic review and meta-analysis. BMJ 57, 749-757 (2016).
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref