Research Article - Interventional Cardiology (2020) Volume 12, Issue 4
Medical Malpractice in Interventional Cardiology: Identifying Patterns and Areas for Improvement
Ashley Szabo Eltorai*Department of Anesthesiology, Division of Cardiac Anesthesia, Yale University School of Medicine, Connecticut, USA
- *Corresponding Author:
- Ashley Szabo Eltorai
Department of Anesthesiology
Division of Cardiac Anesthesia
Yale University School of Medicine
Connecticut, USA
E-mail: ALS124@case.edu
Received date: June 27, 2020; Accepted date: July 13, 2020; Published date: July 20, 2020
Abstract
Introduction: The feared possibility of involvement in a medical malpractice lawsuit ultimately becomes reality for many physicians in high-risk specialties including cardiology. In a survey of cardiologists and fellows, 15.9% of those from the United States and 13.5% from China stated they were influenced by the fear of malpractice litigation in at least half of all cases they managed daily. A study of 40,916 physicians covered by a large nationwide professional liability insurer from 1991 to 2005 found that the percentage of cardiologists facing a malpractice claim each year is between 7.5%-10%, above the average across all physicians. This study analyzes interventional cardiology malpractice claims by specific procedure and allegation types.
Methods: Seventy-nine cardiology malpractice claims involving procedures were identified in a major nationwide legal database (over 200,000 cases) called VerdictSearch. An exemption was obtained from the Yale University Institutional Review Board. Baseline patient characteristics, reasons for lawsuit, and case outcomes were recorded. Statistical analysis included percentage distributions and Fisher’s exact test.
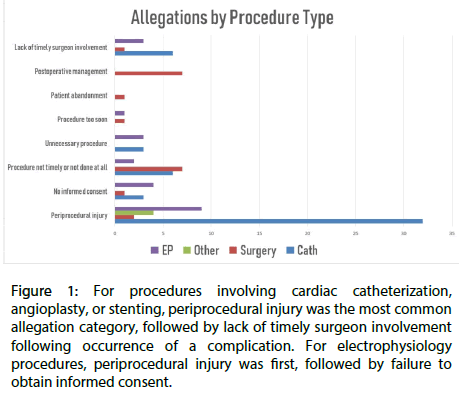
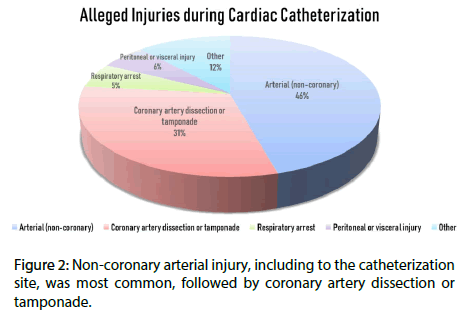
Results: A defendant verdict was reached in 64.6% of cases; plaintiƒ verdict, 21.5% (with average payout $5,212,719.79); and settlement, 13.9%. Death was the injury in 48.1% of cases and did not influence the likelihood of a plaintiƒ verdict. Of the 53.2% of cases involving cardiac catheterization, angioplasty, or stenting, periprocedural injury was alleged in 83.3%, lack of informed consent in 7.1%, failure to perform the correct procedure in a timely manner or at all in 14.3%, and performance of an unnecessary procedure in 7.1% (Figure 1). The most common injury type was arterial (non-coronary), including injury to the catheterization site, followed by coronary artery dissection or tamponade (Figure 2). Electrophysiology procedures were the next most common category, and receiving a defendant verdict was significantly less likely for these cases than any other type. A cardiothoracic or vascular surgeon was named as a co-defendant in 25.3% of cases. In 12.6% of cases, cardiologist failure to obtain timely surgical consultation or ensure backup surgeon availability during procedure performance was alleged.
Discussion: Comprehensively reviewing interventional cardiology malpractice claims can elucidate common contributory factors to adverse outcomes and practice improvement opportunities. This study ’ s results suggest, for instance, that securing appropriate cardiothoracic surgical backup prior to a catheterization, angioplasty, or stent procedure would significantly decrease the number of lawsuits. Diligence in the informed consent process should also be prioritized, as this area generated allegations in 7.1% of cases. Though VerdictSearch is a large, nationwide legal database, its content is limited to those attorneys, courts, and states who choose to report cases. However, any selection biases may be bidirectional and ultimately cancel each other out, since the attorney on the prevailing side of every case theoretically has equal incentive to report it to a public database so the verdict can be used as a marketing tool for that attorney. By uniquely stratifying cardiology malpractice claims within a large nationwide database by specific procedure types and allegations, this study points to factors that commonly contribute to adverse patient outcomes and enables cardiologists to reflect upon opportunities for clinical practice improvement.
Keywords
Malpractice; Legal; Complications
Introduction
The feared possibility of involvement in a medical malpractice lawsuit ultimately becomes reality for many physicians in high-risk specialties such as cardiology. In a survey [1] of cardiologists and fellows, 15.9% of those from the United States and 13.5% from China stated they were influenced by the fear of malpractice litigation in at least half of all cases they managed daily. A study [2] of 40,916 physicians covered by a large nationwide professional liability insurer from 1991 to 2005 found that the percentage of cardiologists facing a malpractice claim each year is between 7.5%-10%, above the average across all physicians. These findings mirrored another study [3] in which 8.6% of cardiologists faced a claim each year, compared with 6.6% of general internists and 18.9% of cardiothoracic surgeons.
In another large analysis [4], the period from 2006 to 2015 brought an overall increase in the number of malpractice claims and annual indemnity payments for cardiologists. Even though 98% of claims were either decreased, denied, dismissed, or settled outside of court, the process of undergoing a malpractice lawsuit is undoubtedly stressful and consumes both time and financial resources.
While a small number of prior studies have investigated medical malpractice in cardiology, the current study, focused upon a large nationwide database of malpractice claims, is the first to stratify them by specific procedure types within interventional cardiology and analyze the alleged injury mechanisms in each case. It was hypothesized that cases resulting in plaintiff death would be more likely to have plaintiff verdicts. For cases involving cardiac catheterization, the most common injury type was hypothesized to be arterial injury, including to the catheterization site.
Materials and Methods
Malpractice cases were located with VerdictSearch (http:// verdictsearch.com), a national database of over 2,00,000 cases whose outcomes are reported by involved attorneys. An exemption was obtained from the Yale University Institutional Review Board (New Haven, Connecticut, United States) since the data are publicly available. The database was queried for all cases within the category “Medical Malpractice ” plus subcategory “ cardiac care, ” “ cardiac surgery, ” or “ heart surgeon ” to include the maximum number of procedural cases among cardiologists, including those involving cardiac surgeons and cardiologists as co-defendants. Cases were excluded if no cardiac procedure was performed.
Statistical AnalysisThe following data were recorded for each case: patient age and gender when the event occurred (if only a decade range was given, such as “80s,” then the median age within that range, in this case “85,” was used), event year, procedure type, types of physicians named as defendants, case outcome with respect to the cardiologist (for mixed verdicts, if the cardiologist was found liable, then the case was entered as “plaintiff”; if the cardiologist was not found liable, then it was entered as “defendant”), dollar amount of settlement or plaintiff award if applicable, and alleged types of injury and negligence. Allegations were classified into the following categories: periprocedural injury, failure to perform the correct procedure in a timely manner or at all, performing a procedure too soon, performing an unnecessary procedure, lack of informed consent, and patient abandonment. Up to three categories were recorded per case.
Data were entered into Microsoft Excel 2016 (Microsoft Corporation, Version 16.0.9126.2295). Mean patient age and monetary values of plaintiff awards and settlements were calculated. Percentage distributions were obtained for patient gender, medical specialty sued, procedure type, injury type, and legal outcome of case. Fisher’s exact test was employed to look for significant associations between injury type and likelihood of defendant or plaintiff verdicts.
Results
Baseline case characteristics
In total, 342 cases were identified in the VerdictSearch database within the category “Medical Malpractice” plus subcategory “cardiac care,” “cardiac surgery,” or “heart surgeon. ” Two hundred two malpractice cases were excluded because they did not include a cardiac procedure, and 18 claimed inappropriate preoperative cardiac clearance for non-cardiac surgery. Of the 140 cases remaining, a cardiologist was not named among the defendants in 61; these cases all included either a hospital or a cardiothoracic or vascular surgeon as defendants. Thus, 79 cases remained in the final analysis. The time range was 1997 to 2014, with the year unavailable for three cases.
Baseline case characteristics were identified (Table 1). The mean plaintiff age was 58.4 years, and 63.3% were male. A defendant verdict was entered for 64.6% of cases and a plaintiff verdict for 21.5% (with average payout $5,212,719.79), while parties in the remaining 13.9% of cases reached a settlement. Death was the alleged injury in 48.1% of cases (38/79). The likelihood of a defendant or plaintiff verdict was not significantly associated with death as the injury type (Fisher exact test statistic=1, p<0.05). The most frequent procedure types involved were cardiac catheterization, angioplasty, and/or stenting (53.2%, 42/79), followed by electrophysiology procedures including ablations and pacemaker/ICD placement or component replacement (21.5%, 17/79). A cardiothoracic or vascular surgeon was named as a co-defendant, along with a cardiologist, in 25.3% of cases (20/79), and an anesthesiologist was named in one case. In 12.6% of cases (10/79), the plaintiffs alleged either cardiologist failure to consult a cardiothoracic or vascular surgeon in a timely manner, or that the cardiologist inappropriately performed a procedure when a surgeon was not available on-call.
| Characteristic | Value | |
|---|---|---|
| Mean Plaintiff Age | 58.4 years | |
| Plaintiff Gender | Male 63.3% | |
| Female 35.4% | ||
| Multiple Plaintiffs 1.2% | ||
| Legal Outcome* | Defendant Verdict | 64.60% |
| Plaintiff Verdict | 21.50% | |
| Settlement | 13.90% | |
| Mean Award Amount | Plaintiff Verdict | $4,150,437.80 |
| Settlement | $39,104,545.45 (Single settlement of $419,000,000.00) | |
| Procedure Type | Cardiology (cardiac catheterization, angioplasty, stent) | 53.20% |
| Electrophysiology (ablation, pacemaker/ICD) | 21.50% | |
| Cardiac surgery | 20.20% | |
| Other** | 5.10% | |
| Specialty Sued | Cardiologist | 100% |
| Cardiothoracic or Vascular Surgeon | 25.30% | |
| Anesthesiologist | 1.30% | |
| Injury Type | Death | 48.10% |
| Brain | 15.20% | |
| Limb | 11.40% | |
| Other | 27.80% | |
*Verdict outcomes were entered with respect to the cardiologist. If a mixed verdict were entered and the cardiologist was found liable, then the case was entered as “plaintiff”; if not, then the case was entered as “defendant.” **Transesophageal echocardiography, percutaneous atrial septal defect closure, pericardiocentesis, or Greenfield filter placement.
Table 1: Baseline case characteristics. Plaintiff gender was not available for one case because it contained multiple plaintiffs. Age was unavailable for two cases.
Malpractice litigation by procedure
Of the 42 cases in this data set that involved cardiac catheterization, angioplasty, and/or stenting, periprocedural injury was alleged in 83.3%, lack of informed consent in 7.1%, failure to perform the correct procedure in a timely manner or at all in 14.3%, and performance of an unnecessary procedure in 7.1% (Figure 1). In addition, in 14.3% of cases (6/42), it was alleged that either the cardiologist failed to consult a cardiothoracic or vascular surgeon in a timely manner, or that the cardiology procedure was performed inappropriately when a surgeon was not available as backup. The average plaintiff award across these cases was $3,048,965.38, and the average settlement was $70,745,833.33 (single settlement of $419,000,000).
Figure 1: For procedures involving cardiac catheterization, angioplasty, or stenting, periprocedural injury was the most common allegation category, followed by lack of timely surgeon involvement following occurrence of a complication. For electrophysiology procedures, periprocedural injury was first, followed by failure to obtain informed consent.
Cases in this category were not significantly more likely to have defendant or plaintiff verdicts than the rest of the cases in the data set (Fisher exact test statistic 0.2794 at p<0.05). The most common injury type was arterial (non-coronary), including injury to the catheterization site (45.7% of all injuries); next was coronary artery dissection or tamponade (31%) (Figure 2). Neither of those injury types were significantly associated with likelihood of defendant or plaintiff verdicts (Fisher exact test statistic values 0.6278 and 0.3826, respectively, at p<0.05). Periprocedural respiratory arrest and peritoneal or visceral injury each represented 5.7% of all injuries.
Figure 2: Non-coronary arterial injury, including to the catheterization site, was most common, followed by coronary artery dissection or tamponade.
Of the 17 EP cases, nine (52.9%) alleged periprocedural injury, four (23.5%) alleged lack of proper informed consent, two (11.8%) alleged failure to perform the correct procedure in a timely manner or at all, three (17.6%) alleged performance of an unnecessary procedure, and one (5.9%) alleged that a procedure was performed too soon (Figure 1). Allegations of either failure to obtain a surgical consultation in a timely manner, or performance of a procedure in the absence of cardiothoracic surgical backup, were present for 17.6% (3/17) of cases. Receiving a defendant, compared to a plaintiff, verdict was significantly less likely for EP cases than for the rest of the cases in the data set (Fisher exact test statistic 0.0074 at p<0.05). The average plaintiff award was $4,139,335.62, and the average settlement was $1,800,000.00.
Cardiac surgical procedures represented 25.3% of cases. In all but one, a cardiologist and a cardiothoracic or vascular surgeon were co-defendants; in the final case, the hospital and cardiologist were sued. These cases were not significantly associated with increased likelihood of defendant or plaintiff verdicts compared to the rest of the data set (Fisher exact test statistic values 0.6278 and 0.3826, respectively, at p<0.05). The average plaintiff award was $8,050,000.00, and the average settlement was $691,666.67.
Coronary artery bypass grafting (CABG) was the most common procedure represented (50% of cases, 8/16), followed by valvular surgery (31.2%, 5/16) and aortic surgery (12.5%, 2/16). Most lawsuits cited either failure to perform an indicated procedure or postoperative mismanagement (each represented 43.8% of cases), while perioperative injury was cited in two cases; one case each cited lack of informed consent, performing an operation too soon, lack of timely surgical intervention, or patient abandonment (Figure 1). All cases of postoperative mismanagement occurred with either CABG or valvular surgery.
Discussion
In this retrospective study of a major national legal database, cardiology malpractice lawsuits that were tied to performance of a procedure had a 64.6% likelihood of a defendant verdict, and plaintiff verdicts were not more common amongst cases for which death was alleged, contrary to what was hypothesized. These findings resemble those of a small study [5] of 17 cases of retroperitoneal hemorrhage occurring after coronary angiography and intervention, where plaintiff victory occurred in only 14% of lawsuits; even 70% of cases in which the patient died had defendant verdicts. Lack of timely surgeon involvement following complications during cardiac catheterization was the second most frequent allegation type for these procedures, which appears consistent with a large (>26,000- patient) study finding that conservative treatment was elected for 79.2% of cases of retroperitoneal hemorrhage as a complication of cardiac catheterization, even though 39.6% of the patients presented with hemorrhagic shock [6].
Of the cases involving cardiac catheterization, angioplasty, or stenting, the most common injury type was arterial (noncoronary), including injury to the catheterization site, followed by coronary artery dissection or tamponade. While these complications will inevitably occur on occasion, one modifiable aspect of practice entails ensuring surgical consultation in a timely manner or refraining from performing a procedure when a cardiothoracic surgeon is unavailable as backup, as allegations related to these topics existed in 14.3% of cases. Another involves diligence in the informed consent process, an area that generated allegations in 7.1% of cases. One way to improve the informed consent process could entail providing an educational video to patients scheduled for elective cardiac catheterization, as one study [7] found that this improved both patient understanding and satisfaction. Cardiologists can also improve their informed consent processes through awareness of the points that their patients most commonly understand; for instance, 60% of 326 cardiology patients in one survey in England erroneously believed that percutaneous coronary intervention was “curative” [8].
In the EP cases in this study, a defendant, rather than plaintiff, verdict was significantly less likely compared to other case types. One hypothesis for this finding is that lack of proper informed consent was the second most common allegation type after periprocedural injury for these cases, and it may be more difficult to identify failures in the informed consent process than other categories of poor outcomes due to the lack of objective documentation (that is, consent conversations are usually not recorded, whereas medical complications are more easily tracked with nurses’ documentation of vital signs, patient symptoms, and so forth in real time).
During a medical malpractice trial, the plaintiff must prove that the defendant breached patient care duties by departing from currently held standards [9]. Therefore, the cases in this study can be deemed to reflect the commonly accepted standards of care in cardiology at present, such as the specific expectations for cardiothoracic surgical backup coverage for various cardiology procedures. When specific allegations and case outcomes are scrutinized, pattern identification can support proposed policy changes and other quality improvement modalities. To complicate the issue, the landscape of medical malpractice is ever-changing; as one example, physicians were traditionally advised by legal counsel not to apologize to patients as it implies culpability for a bad outcome, but many have now passed apology laws [10].
Though VerdictSearch is a large, nationwide legal database, it presents study design limitations in that its content is limited to the attorneys, courts, and states who choose to report cases. Undoubtedly, some relevant cardiology malpractice cases were not included, and selection biases may be present with respect to various case features, such as practice setting or plaintiff or defendant demographics. However, the selection biases may be bidirectional and ultimately cancel each other out, since the attorney on the prevailing side of every case theoretically has equal incentive to report it to a public database, so that the verdict can be used as a marketing tool for that attorney [9].
Conclusion
By uniquely stratifying cardiology malpractice claims within a large nationwide database by specific procedure types and allegations, this study points to factors that commonly contribute to adverse patient outcomes and enables cardiologists to reflect upon opportunities for clinical practice improvement. According to this study’s findings, such opportunities include a more diligent informed consent process, improved attentiveness to arterial catheterization sites to avoid injury, and securement of cardiac surgical backup for procedures.
Conflict of Interests
There is no conflict of interest between authors.
References
- Badri M, Abdelbaky A, Yan GX, et al. The impact of medical malpractice litigation on cardiovascular practice in the US and China. Int J Cardiol. 177(1): 48-50 (2014).
- Jena AB, Seabury S, Lakdawalla D, et al. Malpractice risk according to physician specialty. N Engl J Med. 365(7): 629-36. (2011).
- Mangalmurti S, Seabury SA, Chandra A, et al. Medical professional liability risk among US cardiologists. Am Heart J. 167(5): 690-6 (2014).
- Brown PP, Kugelmass AD, Cohen DJ, et al. The frequency and cost of complications associated with coronary artery bypass grafting surgery: results from the United States Medicare program. Ann Thorac Surg. 85: 1980-1986 (2008).
- Voudris K, Vidovich M. Medicolegal Implications of Radial and Femoral Access for Coronary Angiography and Intervention in 2016: Focus on Retroperitoneal Hemorrhage. J Transl Int Med. 4(1): 29-34 (2016).
- Eison A, Kornowski R, Vaduganathan M, et al. Retroperitoneal bleeding after cardiac catheterization: a 7-year descriptive single-center experience. 125(4): 217-22 (2013).
- Lattuca B. Impact of Video on the Understanding and Satisfaction of Patients Receiving Informed Consent Before Elective Inpatient Coronary Angiography: A Randomized Trial. Am Heart J. 200: 67-74 (2018).
- Astin F. Cardiologists' and Patients' Views About the Informed Consent Process and Their Understanding of the Anticipated Treatment Benefits of Coronary Angioplasty: A Survey Study. Eur J Cardiovasc Nurs. 19(3): 260-268 (2020)
- Abbott R, Cohen M. Medico-legal issues in cardiology. Cardiol Rev. 21(5): 222-8 (2013).
- Saitta N, Hodge SD. Efficacy of a physician’s words of empathy: an overview of state apology laws. J Am Osteopath Assoc. 112(5): 302-6 (2012).