Review Article - Interventional Cardiology (2020) Volume 12, Issue 5
Migraine in patients with Patent Foramen Ovale: is there a link?
- Corresponding Author:
- Federico Cacciapuoti
Department of Internal Medicine
"L. Vanvitelli" University of Campania
Naples, Italy
E-mail: fulvio.cacciapuoti@gmail.com
Received Date: August 10, 2020, Accepted Date: August 24, 2020, Published Date: August 30, 2020
Abstract
Background: PFO is a hole between right and left atrium, that is normally present in human fetus, but that sometimes persists in adulthood. Migraine is a neurological disorder frequent in adult patients having Patent Foramen Ovale (PFO). Methods and Results: A variety of clinical manifestations, such as migraine (with or without aura), TIA or cryptogenetic stroke can be present in adult patients with PFO persistence. Echographic findings for diagnosis and percutaneous closure with an Amplazer or other devices for migraine improvement were described. Nevertheless, while some studies report a significant improvement of migraine after PFO closure, other trials refer uncertain or negative results on migraine symptoms after the placement of Amplazer or other devices inducing PFO closure. Conclusion: These uncertain results indicate the relationship between PFO and migraine not is clear and the evidences obtained till now testify both for causal or casual account between two events.
Keywords
Migraine; Patent Foramen Ovale (PFO); Right-to-left shunt; Contrast medium; Microbubbles; Amplazer or other devices
Abbreviation List
PFO: Patent Foramen Ovale; TIA: Transient Ischemic Attack; TTE: Trans-Thoracic Echocardiography; TEE: Trans-Esophageal Echocardiography; TCDE: Trans-Cranial-Doppler Echography; LV: Left Ventricle; 5-HT:5 Hydroxy-Tryptamine; MIST: Migraine Intervention with STARflex Techonogy; PRIMA: Percutaneous closure in migraine with Aura; PREMIUM: Prospective Randomized investigation to Evaluate Incidence of headache reduction in subjects with Migraine and PFO Using the AMPLAZER PFO occlude the medical Management.
Introduction
Migraine is a neurological disorder, frequently marked by recurrent headache with throbbing pain interesting one side of the head that may extend to both sides. That usually lasts from four hours to three days. It is often accompanied by nausea, vomiting and sensitivity to light or sound, and is sometimes preceded by aura and followed by fatigue [1]. Some migraneurs will have many or all the symptoms of migraine with “aura”. Aura consists of one or more focal neurological symptoms, such as visual sensory or speech disturbances. This occurs in about 15-30% of migraineurs and happens shortly before a migraine attack. They range from seeing sparks, bright dots, and zig-zags to tingling on one side of the body or on inability to speak clearly and usually last 20-60 minutes [2]. Migraine is three-times more common in women than in men and its prevalence peaks at 40 years of age [3]. migraine are reported in Table 1 [4,5].
| Possible causes of migraine and their most common triggers | |
|---|---|
| Causes | Triggers |
| Genetic predisposition | Physical or mental stress |
| Disorders of CNS | Some foods (cheese, alcohol, etc.) |
| Irregularity in brain’s vascular system | Several stimuli (cigarette smoke, perfume, hormones, etc.) |
| Abnormalities of brain chemicals | Others |
Table 1. Some causes and triggers for migraine.
Patent Foramen Ovale
Apart the risk factors for migraine reported in Table 1. Patent Foramen Ovale (PFO) were indicated as an important cause of migraine headaches. PFO is present more than two-fold in patients with migraine with aura in comparison to those without aura [6].
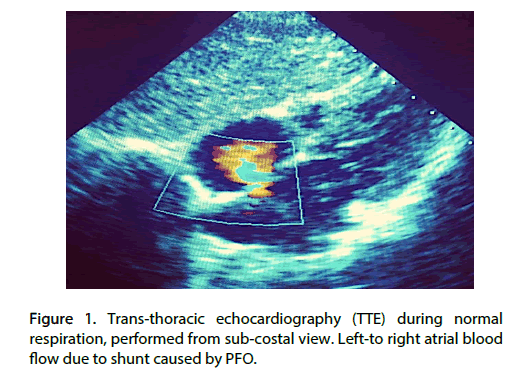
PFO is a congenital heart defect defined such as an opening in the mild portion of the interatrial septum, at the junction of the septum premium to septum secundum [7,8]. PFO is seen from subcostal view (Figure 1). Mostly, spontaneous closure occurs before the birth or in the first two months of life. However, approximately 20-25% of healthy adults in the general population has a PFO and is asymptomatic. But, when the right atrial pressure increases more than the pressure in the left atrium, temporarily (Valsalva maneuver, cough) or persistently (abdominal compression), the blood flow inverted and runs from right to left atrium through PFO. This leads the venous blood flow towards cerebral circulation. The paradoxical (reversed) circulation can cause several cerebral accidents, such as migraine TIA, or cryptogenetic stroke [9-11].
Figure 1: Trans-thoracic echocardiography (TTE) during normal respiration, performed from sub-costal view. Left-to right atrial blood flow due to shunt caused by PFO.
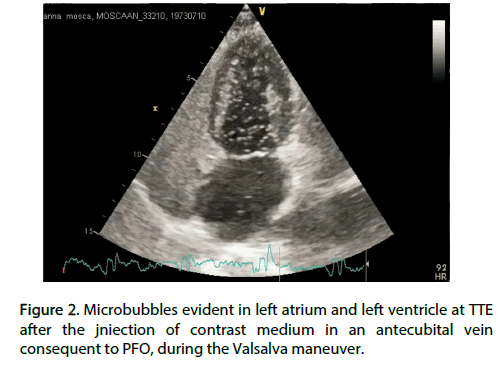
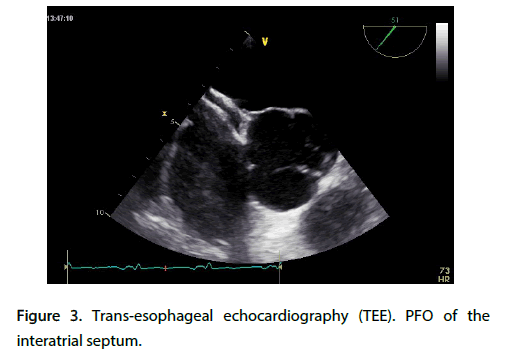
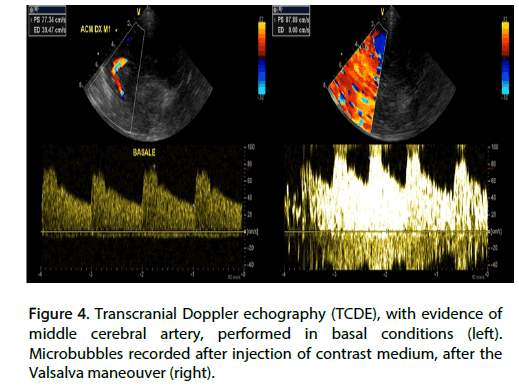
Noninvasive diagnosis of PFO is done by the ultrasound method, using trans-thoracic echocardiography (TTE), trans-esophageal echocardiography (TEE) or trans-cranial doppler echography (TCDE). TTE is performed side by side with agitate saline injection in a brachial vein of a contrast medium during the Valsalva maneuver or cough. PFO is evidenced through the demonstration of microbubbles in LV coming from right-to-left atrium (Figure 2) [12]. But, the gold standard echo-technique for to point the paradoxical blood-passing is TEE. PFO is seen in Figure 3 [13]. TCDE is the technique suitable to visualize the passing of microbubbles in the brain arteries in the presence of right-to-left shunt. The evidence of microbubbles in the middle cerebral artery before and after injection of contrast medium suggests the presence of intracardiac shunt, such as in Figure 4 is seen [14].
Figure 3: Trans-esophageal echocardiography (TEE). PFO of the interatrial septum.
In this review, we illustrate the relationship between PFO and migraine. Concerning this, it must be added that PFO was found in about 40% to 60% of people suffering migraine in comparison to 20% 30% of population without PFO.
PFO and migraine
An increased pressure in the right atrium in the presence of PFO favors the blood-passing from pre-pulmonary to systemic circulation. That induces a right-to-left shunt (paradoxical passage) of platelets with their Serotonin content and other vasoactive amines from venous to arterial circulation. Serotonin (present in the platelets) is removed by pulmonary monoamine oxidase enzyme when the blood flow normally reaches the pulmonary circulation. For rightto- left shunt, Serotonin (jointed at the brain arterial circulation) may irritate the trigeminal nerve, triggering migraine. Concerning the connection of the monamine neurotransmitter and migraine, it must be added that Serotonin antagonizes Triptans that abort migraine attacks, favoring these [15]. Concordantly, a small study has demonstrated that aspirin, an antiplatelet drug that reduces the formation of platelet-fibrin complexes, improves migraine [16]. Finally, Mazal and Rachmilewitz evidenced that an antiserotonin agent, Pirotifen, reduces platelet ’ s aggregability in migraine patients and improves this neurological disorder [17]. The nociceptive effect of Serotonin on meningeal covering of trigeminal nerve was recently still reported [18]. Conclusively, the relation between PFO and migraine is explained by the effect of some vasoactive substances (such as 5HT), normally removed in the pulmonary circulation that, in the presence of right-to-left shunt, can bypass lungs filter and enter in cerebral circulation, inducing migraine attack [19]. Another mechanism related to the relationship of PFO with migraine is that transient hypoxemia due to the paradoxical shunt of blood through the PFO causes microinfarcts in the brain, leading to brain-irritation [15]. It was also added that some data suggest the prevalence of migraine with aura in PFO-patients, depends on the size of right-to-left shunt. This resulted in the hypothesis that substances that circumvent the pulmonary filter, can cross the shunt and cause arterial vasoconstriction, precipitating migraine with aura [19]. With regard to aura in PFO-patients, it must also add that the prevalence of PFO in migraine with aura ranges between 41% and 89%, whereas it is between 7% and 34% in migraneurs without aura [20].
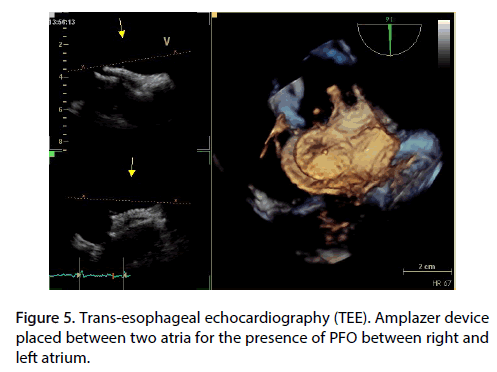
On the grounds of all considerations before reported, the PFO closure has been proposed as non-medical, therapeutical procedure to avoid or reduce migraine-attacks. But, whereas some studies found an improvement of migraine after PFO closure, other trials did not find significant differences in migraine attacks between before and after PFO closure. In accordance with the first statement, a case-control study refers on a causal relation between migraine (especially with aura) and PFO and reports a migraine improvement after the PFO closure with Amplazer (Figure 5) or another device placed at point of interatrial shunt [21]. Concordantly, other reports underline also a significant reduction of migraine attacks in patients with PFO submitted to its closure [22,23]. On the contrary, other reports, such as Migraine Intervention with STARflex Technology (MIST) [24], Percutaneous closure of PFO in Migraine with Aura (PRIMA) [25], and Prospective Randomized Investigation to Evaluate Incidence of Headache Reduction in Subjects with Migraine and PFO Using the AMPLAZER PFO occlude to Medical Management (PREMIUM) [26] trials did not find a significant effects on migraine from PFO closure. These contrasting results depend from some observations. Primarily, paradoxical cerebral embolism in PFO-patients is presumed only, but unrecorded [28]. Furthermore, no consistent link between migraine attack and ischemic (cryptogenic) stroke was found in PFO-patients after Valsalva maneuver [27].
Figure 5: Trans-esophageal echocardiography (TEE). Amplazer device placed between two atria for the presence of PFO between right and left atrium.
In addition, in patients suffering of migraine with aura who undergo transcatheter closure of PFO, the presence of aura and residual right-to-left shunt appears to influence the amount of migraine benefits [28]. Paradoxically, the PFO closure can also precipitate or exacerbate migraine. In fact, the procedure involves implanting a double disc device across the septum, which one disc in each atrium. The disc placed in the left atrium can activate platelets downstream from the lungs, favoring the migraine attacks [29]. On the other hand, multiple uncertaines rise from those trials which would demonstrate the inefficacy of percutaneous closure of PFO. In fact, in PRIMA study no significant difference was found between the migraine groups treated with percutaneous Amplazer and those receiving medical therapy [25]. Likewise, PFO closure in the PREMIUM trial failed to demonstrate a significant reduction of headache frequency among patients with migraine refractory to medications. In addition, the procedure was related to some complications, such as atrial fibrillation, hematomas and transient hypotension [26].
Finally, referring to the low effectiveness of percutaneous closure only and to the greater validity of medical therapy, MIST study pointed out that the risk of recurrent stroke was significantly lower in group treated with PFO closure plus antiplatelet therapy than in patients receiving antiplatelets alone [24]. Another interesting phenomenon, that further confirms the disagreement between PFO closure and migraine improvement, is the observation of an exacerbation of pre-existing migraine with aura after PFO closure. This paradoxical phenomenon would report to the chemical composition of Amplazer, which is made by Ninitol, an alloy of Nickel and Titanium. Specifically, Nickel allergy p induces excessive inflammation, platelet’s activation and release of Serotonin, with migraine and aura [30].
Conclusion
In accordance with Reisman and Fuller [31], we conclude that certain PFO-patients have a dramatic response to closure of PFO with an Amplazer device, with significant reduction or complete elimination of migraine headache.
On the contrary, in others the PFO closure has uncertain, aggravating or paradoxal results. At moment, the causes of these diverse behaviours are unknown. Future studies performed in wide range of PFO-populations are requested to elucidate if the relationship between migraine and PFO is causal or simply casual.
Conflict of interest
There is no conflict of interest
Funding
There is no funding support
References
- Olesen J, Bendtsen L, Goadsby P, et al. Headache Classification Committee of the International Headache Society. The international classification of headache disorders. Cephalalgia. 38: 1-11 (2018).
- De Lange JM, Cutrer FM. Our evolving understanding of migraine with aura. Curr Pain Headache Rep. 18: 453 (2014).
- Silberstein SD. Migraine. Lancet. 363: 381-391 (2004).
- Maleki N, Becerra L, Borsook D. Migraine: maladaptative brain responses to stress headache. Headache. 52(S2): 102-106 (2012).
- Sauro KM, Becker WJ. The stress and migraine interaction. Headache. 49(9): 1378-1386 (2009).
- Schwedt TJ, Demaerschalk BM, Dodiek DW. Patent foramen ovale and migraine: a quantitative systematic review. Cephalalgia. 28: 531-540 (2008).
- Sadler WL. Langman’s.: Medical Embriology 11th ed. Philadelphia, PA: Wolters Kluewer Lippincott Williams & Wilkins (2010).
- McCarthy K, Ho SAR. Defining the morphologic phenotypes of atrial septal defects and interatrial communications. Images Paediatr Cardiol. 5(2): 1-24 (2003).
- Azarbal B, Tobis J, Chan V, et al. Association of interatrial shunts and migraine headaches: impact of trans catheter closure. J Am Coll Cardiol. 45(4): 489-492 (2005).
- Lamy C, Giannesini C, Zuber M, et al. Clinical and imaging findings in cryptogenetic stroke patients with and without patent foramen ovale: the PSO-ASA Study. Stroke. 33: 706-711 (2002).
- Di Tullio MR, Sacco RL, Sciacca R, et al. Patent foramen ovale and the risk of ischemic stroke in a multiethnic population. J Am Coll Cardiol. 49(7): 797-802 (2007).
- Mojadidi MK, Winoker JR, Roberts SC, et al. Accuracy of conventional trans-thoracic echocardiography for the diagnosis of intracardiac right-to-left shunt: a meta-analysis of prospective studies. Echocardiography. 31(9): 1036-1048 (2014).
- Mojadidi MK, Bogush N, Caceres JD, et al. Diagnosis accuracy of transesophageal echocardiogram for the detection of patent foramen ovale: a meta-analysis. Echocardiography. 31(6): 752-758 (2014).
- Mojadidi MK, Roberts SC, Winoker JS, et al. Accuracy of transcranial Doppler for the diagnosis of intracardiac right-to-left shunt: a bivariate meta-analysis of prospective studies. JACC Cardiovasc Imaging. 7(3). 236-250 (2014).
- Sharma A, Gheewala N, Silver P. Role of patent foramen ovale in migraine etiology and treatment: a review. Echocardiography. 28(8): 913-917 (2011).
- Grotemeyer KH, Schratiaski HW, Schlake HP, et al. Acetylsalicylic acid vs. metoprolol in migraine prophylaxis. A double, blind, cross-over study. Headache. 30(10): 639-641 (1990).
- Mazal S, Rachmiliwitz EA. The effect of an antiserotonin agent pirotifen on platelet aggregability in migraine patients. J Neurol Neurps Psychiatry. 43(12): 1137-1140 (1980).
- Kilin E, Guerrero-Toro C, Zakharov A, et al. Serotoninergic mechanisms of trigeminal nociception: implications for migraine pain. Neuropharmacology. 116: 160-173 (2017).
- Peter W, Simon N. The role of cardiac and pulmonary pathology in migraine: a hypothesis. Headache. 46(3): 429-434 (2010).
- Rigatelli G. Migraine and patent foramen ovale: connecting flight or one-way ticket? Expert Rev Neurother. 8(9): 1331-1337 (2008).
- Anzola GP, Mazzucco S. The patent foramen ovale-migraine connection: A new perspective to demonstrate a causal relation. Neurol Sci. 29: S15-S18 (2008).
- Kanwar SM, Noberia A, De Simone CV, et al. Coincidental impact of transcatheter patent foramen ovale closure on migraine with or without aura A comprehensive meta-analysis. Clin Trials Regul Sci Cardiol. 15: 7-13 (2016).
- Kato Y, Kabayashi T, Ishido H, et al. Migraine attacks after transcatheter closure of atrial septal defect. Cephalalgia. 33: 1229 (2013).
- Dowson A, Mullen MJ, Peatfield R, et al. Migraine intervention with STARFlex technology (MIST) trial. Circulation. 117(11): 1397-1404 (2008).
- Mattle HP, Evers S, Hildick-Smith D, et al. Percutaneous closure of patent foramen ovale in migraine with aura, a randomized controlled trial. Eur Heart J. 37(26): 2029-2036 (2016).
- Tobis JM, Charles A, Silberstein SD, et al. Percutaneous closure of patent foramen ovale in patients with migraine: the PREMIUM trial. J Am Coll Cardiol. 70(22): 2766-2774 (2017).
- Adams HP. Patent foramen ovale: paradoxical embolism or paradoxical data. Mayo Clin Proc. 79(1): 15-20 (2004).
- Ben-Assa E, Rengifo-Moreno P, Al-Bawardi R, et al. Effect of residual interatrial shunt on migraine burden after transcatheter closure of patent foramen ovale. JACC Cardiovasc Interv. 13(3): 293-302 (2020).
- Wilmshurst PT, Nightingale S, Walsh KP, et al. Effect on migraine of closure of cardiac right-to-left shunts to prevent recurrence of decompression illness or stroke or for haemodynamic reasons. Lancet. 356(9242): 1648-1651(2000).
- Wertman B, Azarbal B, Riedl M, et al. Adverse event associated with nickel allergy in patients undergoing percutaneous atrial septal defect or patent foramen ovale closure. J Am Coll Cardiol. 47(6): 1226-1227 (2006).
- Reisman M, Fuller CJ. Is patent foramen ovale closure indicated for migraine? Patent foramen ovale closure for migraine. Circ Cardiovasc Interventions. 2: 468-474 (2009).