Review Article - Interventional Cardiology (2013) Volume 5, Issue 3
Minimizing radiological exposure to pregnant women from invasive procedures
- Corresponding Author:
- Ian C Gilchrist
Penn State Hershey Medical Center,
Heart & Vascular Institute, Hershey,
PA 17033, USA
Tel: +1 717 531 5888
Fax: +1 717 531 7969
E-mail: icg1@psu.edu
Abstract
Keywords
coronary artery disease, interventional cardiology, pregnancy, radiation, radiation protection, stent, valvular heart disease
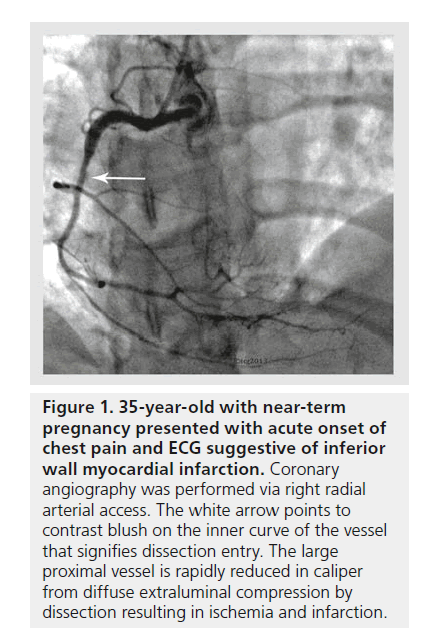
The vast majority of pregnancies are relatively uneventful. Pregnancy-associated cardiovascular disease (CVD) may occur from hypertension [1], cardiomyopathy [2], fibromuscular dysplasia (dissections), acquired or congenital heart disease [3], acquired coronary disease, electrophysiological instability and thrombo-embolic disease (Figure 1). The contribution of underlying etiologies varies around the world, with hypertension and acquired valvular heart disease more prevalent in the less developed regions of the world. In western countries, the mortality from hypertensive disease has dropped and disorders, such as rheumatic fever, have all but disappeared, although an aging maternal population is now reaching into the early years of acquired coronary disease [4].
Figure 1. 35-year-old with near-term pregnancy presented with acute onset of chest pain and ECG suggestive of inferior wall myocardial infarction. Coronary angiography was performed via right radial arterial access. The white arrow points to contrast blush on the inner curve of the vessel that signifies dissection entry. The large proximal vessel is rapidly reduced in caliper from diffuse extraluminal compression by dissection resulting in ischemia and infarction.
Pregnancy can both bring out or destabilize otherwise well-compensated disease. The gravid state can be associated with a set of clinical syndromes or diseases otherwise not present in the nonpregnant state. Pre-existing disease states may be well known and have been well characterized with imaging before pregnancy, resulting in expected care and little need for further diagnosis. On the other hand, occult pre-existing diseases may first manifest under the pregnant state, or disease induced by pregnancy may result in a work-up that requires consideration for radiographic imaging.
This review will focus on sources exposure to ionizing radiation during pregnancy and describe techniques to reduce the amount of radiation delivered to the parturient and the fetus.
What types of cardiovascular imaging are performed during pregnancy?
Advances in imaging technology are occurring rapidly and the potential tool chest for both diagnostic and interventional needs is expanding. With every iteration of technology come improvements in image quality and safety profile. Within the x-ray-dependent technologies, image-intensifier advances and digital processing make images sharper, while requiring less radiation. Likewise, a variety of other nonradiologic technologies have emerged that appear safer than x-ray and can often augment or substitute for traditional diagnostic and interventional x-ray needs.
▪ Technology that does not use x-ray ionizing energy Echocardiography
Indications
Echocardiography (ECHO) allows for safe and noninvasive assessment of heart structure and function. Both transthoracic and transesophageal ECHO can be safely performed at any stage of pregnancy. Its development has been indispensable and has markedly reduced the overall need for x-ray exposure to diagnose valvular heart disease and characterize the status of myocardial function. Shunts can be detected and pulmonary artery pressure can be derived. In addition, ECHO allows for volume-status assessment and may obviate the use of right-heart catheterization to determine ventricular filling pressures.
ECHO can also be carried out transthoracic, transesophageal and intracardiac during invasive procedures. Its use extends beyond just diagnostic considerations and into interventional procedures, where it can be used for imaging or monitoring without radiation exposure. Pacing and defibrillator leads can be managed using ECHO as well as cardiac biopsy procedures instead of tradition fluoroscopy [5]. It can also be used to guide drainage needles, such as for pericardial tamponade, obviating the need for x-ray exposure under many circumstances [6].
Intracardiac ECHO
Compared with transesophageal ECHO, which may be poorly tolerated by parturients and may require administration of intravenous sedation that could be potentially harmful to the fetus, intracardiac ECHO appears particularly suited to the parturient. It can be inserted via femoral venous approach with local anesthesia only and provides comparable images of cardiac structures. Thus, the avoidance of intravenous sedation or general anesthesia required for transesophageal ECHO is highly preferable for the fetus and pregnant women.
Danger to the fetus
At present time, and with decades of safe use, there appears to be no untoward effects of ECHO to the fetus. The use of echocardiographic contrast, for example perflutren lipid microspheres (pregnancy category B [101]), should only be carried out as clearly indicated.
Cardiac MRI
Indications
Cardiac MRI offers superior imaging of cardiac structure and function. It is particularly useful for the assessment of viability, myocardial scars and in adult congenital heart disease.
Danger to the fetus
The present risks of MRI to the parturient are similar to nonpregnant patients. There are two possible risks to the fetus resulting from the use of MRI during pregnancy – teratogenic and acoustic damage. At the present time, there are no published adverse effects resulting from MRI to parturients or the fetus. Due to limited available evidence on MRI safety during the time of organogenesis, it is reasonable to limit use of MRI during the first trimester. The general recommendation is that at any time during pregnancy, cardiac MRI should be performed only when the risk–benefit ratio is justified [7]. None-theless, the quality of images and the diagnostic accuracy of cardiac MRI is superior to almost all other imaging modalities that utilize radiation. Gadolinium is used at times to enhance contrast in MRI. Its use during pregnancy should be avoided and used only if absolutely required. Gadolinium crosses the placenta and is a category C drug [101]. Gadolinium has been shown to be teratogenic in animals [7–9].
▪ Imaging technologies that use x-ray Ionizing radiation risks to the fetus owing to cardiac procedures
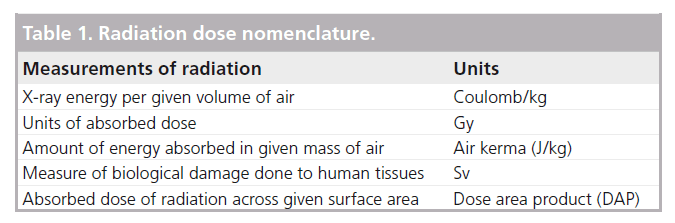
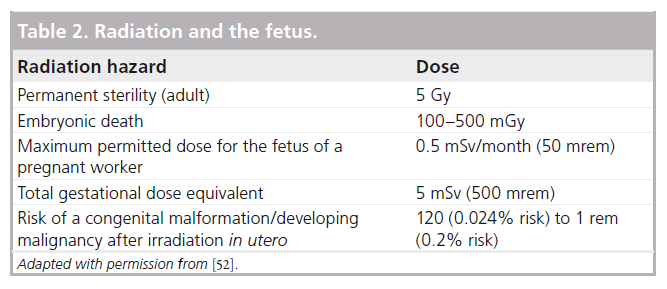
While avoidance of unnecessary ionizing radiation during pregnancy is important, fear of potential radiation risk should not be a deterrent to the use of life-saving procedures. Estimated radiation dose from cardiac catheterization remains far lower than exposure reported to cause teratogenicity. The mean exposure to the unshielded abdomen is approximately 3 mGy for a combination of coronary angiography and stent procedure. Only 20% of the exposure actually reaches the fetus owing to tissue attenuation of the radiation [10]. Doses greater than 50 mGy are associated with congenital malformation and growth retardation [11], and only at dosages greater than 100 mGy should termination of pregnancy be considered on the basis of exposure [12]. Radiation dose nomenclature is summarized in Table 1.
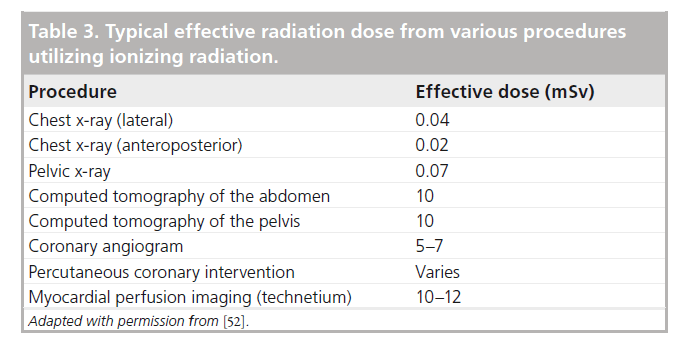
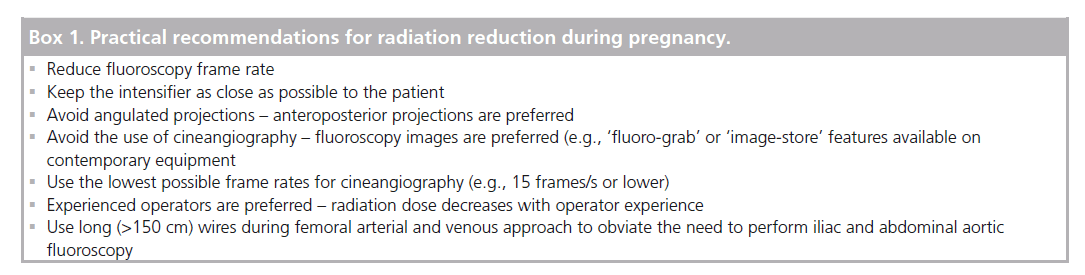
If there is a need for x-ray energy use during pregnancy, the radiation dose can be markedly reduced by using low fluoroscopy frame rates and careful collimation. Cineangiography and magnification result in higher x-ray dosages than simple fluoroscopy and lower magnification. With newer digital equipment, simple fluoros-copy can often be saved and high-dose cineradiography can be avoided. As long as the fetus is not directly within the x-ray beam for cardiac procedures, the exposure of the fetus occurs mainly through indirect (scatter) radiation. Therefore, placing external shielding to protect the fetus is very ineffective [13], although it does reduce exposure to the staff. The fetal radiation dose cannot be directly measured and is therefore estimated [14]. It is encouraging that the overall doses to the fetus are low. Nonetheless, the safest approach is to avoid radiation during pregnancy and, if radiation exposure is needed, carefully evaluate the risk–benefit ratio of such procedures (Tables 2 & 3) [12].
Ionizing energy exposure is significantly higher if the fetus enters the field of the primary x-ray beam. This might occur with a difficult approach from the femoral artery or vein. Likewise, placement of a vena cava filter or potential procedures, such as aortic repair or valve implantation, which require large-vessel cannulation from the femoral region might impart more radiation to the fetus [15]. While this would be a significant increase from the dosage expected from a routine cardiac catheterization using the transradial approach, careful management should still allow completion well within critical limits.
Iodinated contrast use during pregnancy
Based on decades of use, administration of iodinated contrast media during pregnancy appears to be safe. To date, there are no published reports of mutagenic or teratogenic fetal outcomes after administration of iodinated contrast media. Free iodide present in the contrast medium, when administered to the mother, can lower fetal and, after delivery, neonatal function of the thyroid gland. It appears prudent to check neonatal thyroid function during the first week postpartum. In addition, it is worthwhile to note that very small quantity of iodinated contrast dye is excreted in breast milk, and minute amounts are then absorbed through neonate’s gastrointestinal system. This minuscule, yet hypothetical, associated risk is considered to be too small to advise against breast-feeding in the 24 h following iodinated contrast administration [9].
Left-heart catheterization & angiography
Indications
Diagnostic coronary angiography continues to represent the gold standard for diagnosis of coronary artery disease. Pregnancy is not a contra-indication for left heart catheterization – it can be performed at any time during pregnancy. Radial arterial access is preferable to femoral access due to earlier ambulation, increased patient comfort and significant reduction in access-related bleeding complications [10]. In addition, during the procedure, left lateral decubitus position can be more easily maintained with radial access. Cardiologists should strictly follow the as low as reasonably achievable (ALARA) principle so as to limit radiation exposure to the mother and the fetus.
Right heart catheterization
Indications
In recent years, routine use of pulmonary artery catheters has significantly decreased in the USA [16]. The decrease in use has, at least in part, been due to the fact that equally helpful information from the significantly more invasive pulmonary artery catheter can be obtained noninvasively by transthoracic or transesophageal ECHO [17]. However, it is important to emphasize that Fick and thermodilution cardiac output measurements cannot be measured without the pulmonary artery catheter. Analogously, right-heart catheterization is prerequisite for vasoreactivity testing in pulmonary hypertension. In parturients with severe pre-eclampsia and eclampsia, especially in the presence of pulmonary edema or renal insufficiency, pulmonary artery catheterization may be extraordinarily valuable in assessing volume status. This is due to the development of diastolic dysfunction, which complicates noninvasive estimation of left ventricular filling pressures. Nevertheless, in a broad range of clinical scenarios, ventricular filling pressures are fairly accurately assessed noninvasively by transthoracic [17,18] and transesophageal ECHO [19–21].
Computed tomography angiography
Indications
Cardiac structure and function and coronary artery anatomy can be noninvasively assessed with multidetector computed tomography (CT) scanners. Compared with the early scanners, modern machines with advanced dose-reduction algorithms have produced remarkable reduction in the radiation dose.
Danger to the fetus
In experienced centers with quality-control protocols, the total radiation dose delivered with coronary CT angiography can be lowered to equivalent or even lower doses than with traditional invasive coronary catheterization. However, in the absence of meticulous attention to detail, CT can deliver markedly larger radiation dose compared with cardiac catheterization. The advantage of cardiac CT is that it allows the visualization of cardiac structures not visible by coronary angiography. However, these can be imaged using ECHO without the use of ionizing radiation. In addition, the amount of intravenous contrast dye required for coronary CT angiography is greater than for diagnostic catheterization. If coronary intervention is needed, it cannot be performed at the time of CT imaging and would expose the parturient and the fetus to one additional procedure and even more radiation exposure. Therefore, for the vast majority of clinical conditions, invasive coronary angiography remains the preferred method for coronary artery disease diagnosis. In addition, highly experienced operators can obtain diagnostic-quality coronary angiography images with the use of only fluoroscopy, thus avoiding cineangiography. Such refined techniques reduce radiation exposure to the mother and fetus well below any dose achievable with cardiac CT.
Nuclear imaging studies
Indications
Testing for cardiac ischemia along with diagnosing pulmonary embolism can be done with a variety of nuclear tracers such as thallium or technetium. While these may play a role in the general population, their role in the pregnant population is limited.
Danger to the fetus
These tracers will potentially cross into the fetus and the risks associated with their use during key developmental stages are unknown. In addition, the overall radiation dose is often relatively large as far as medical testing is concerned. Alternative imaging techniques that provide at least as good diagnostic precision with less risk to the fetus, exist for most of the diagnostic tests that use radioactive tracers. This technique should be avoided unless other alternatives are exhausted [22].
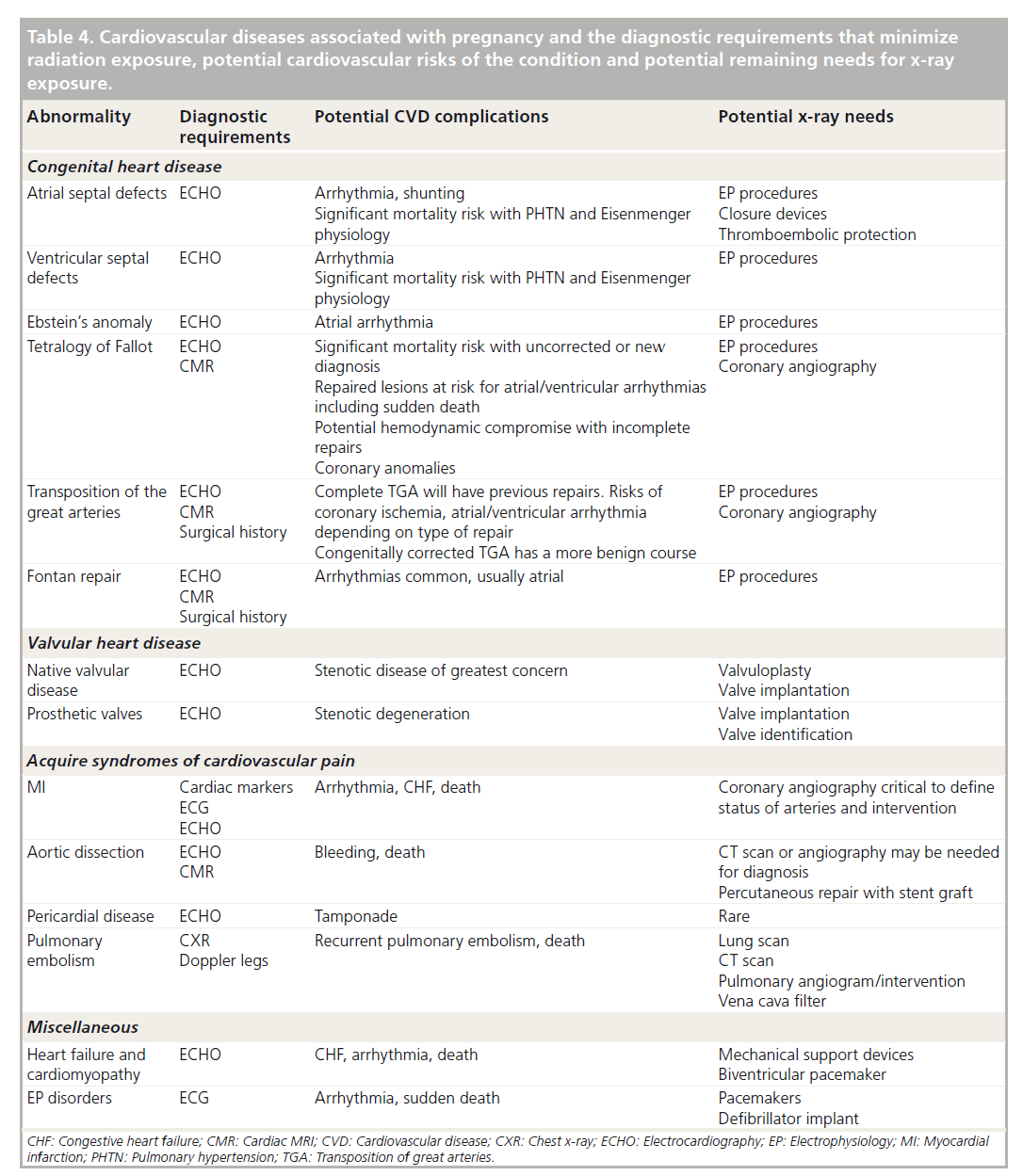
Treatment and diagnostic modalities for various cardiac conditions during pregnancy are summarized in Table 4. Practical recommendations for radiation reduction during pregnancy are shown in Box 1.
Table 4. Cardiovascular diseases associated with pregnancy and the diagnostic requirements that minimize radiation exposure, potential cardiovascular risks of the condition and potential remaining needs for x-ray exposure.
Transradial approach to reduce risks of invasive procedures
Technologic improvements in imaging technology, both within the ionizing radiation field and alternative imaging approaches, have resulted in serial improvements, but the recent widespread introduction of transradial cardiac catheterization techniques have provided another important advance to improve the safety of these procedures [23]. Advances in catheter technology and reduction in equipment size now allow the vast majority of invasive coronary procedures, whether diagnostic or interventional, to be carried out by the radial artery [24]. Owing to its anatomical position and relatively smaller size compared with the traditional femoral artery, use of transradial approaches markedly reduce vascular complications and associated bleeding events in patients [25]. As bleeding events are independent predictors of major cardiac events and death associated with interventional procedures, this is a major improvement for the general population of cardiac patients. In particular, the acute myocardial infarction (MI) patient appears to benefit, with significant reduction in death rates when transradial, rather than transfemoral, access is used [26–28].
Women, in particular, are an independent risk versus men for the development of bleeding and vascular complications after invasive cardiovascular procedures. This risk persists even with bleeding-reduction strategies, including the use of appropriately dosed newer antithrombotic medicines [29]. In addition, the most serious of the femoral-access complications, the retroperitoneal bleed, is more common in women. Overall, women appear to have bleeding or vascular complication rates twice those of men [30]. Regardless of whether this risk is based on a simple difference in anatomical size of the femoral arteries or modification of the vascular wall and hemostatic system by different hormonal milieu, the risk of vascular complications and associated bleeding can be markedly reduced through the use of transradial catheterization. Highly experienced operators and centers can achieve remarkable reductions in bleeding complications using the femoral approach, in particular with the use of closure devices and the use of bivalirudin [31].
While many industrial countries around the world, including European and Asian countries such as China, have converted to primarily transradial approaches, several challenges have slowed the widespread use of transradial approaches in the USA. In general, operator volume in the USA is lower than other countries and may make learning new technology more difficult. US operators have also tended to favor closure devices to seal femoral arteries over their European counterparts who favor manual compression [32]. Women, in particular, are somewhat more prone to access failure in the radial artery and this question is being examined in the present SAFE PCI trial being conducted in the USA [102]. The overseas experience suggests that despite a slightly reduced access success rate, overall benefit will still favor the transradial approach [33,34]. Perhaps the most important indicator of transradial acceptance is the observation that as the shift to transradial from transfemoral approaches occurs around the world [103], one does not see operators reverting back to the older transfemoral approach, but rather short-term obstacles of learning a new technique appear minor compared with the long-term acceptance of the transradial approach.
For pregnant women, the transradial approach appears especially attractive for arterial procedures [35]. Beyond the reduction in access-site complications and bleeding reductions that all patients can benefit from, the use of the radial artery obviates the risk of radiating the fetus if femoral artery access is problematic [36]. In addition, activity can focus on the upper half of the woman’s body and provide some sense of protection or distancing from the fetus. Transradial procedures also allow more flexibility in positioning. Especially during the second or third trimester with the potential for vena cava compression or just mechanical compression from the enlarged uterus, arterial access at the level of the wrist allows much more freedom to have the patient in different positions, even stomach down, if appropriate and more comfortable for the patient. Left lateral decubitus position is the most preferable for parturients to relieve the pressure of the uterus on the inferior vena cava and maintain preload. It should be noted, however, that the incidence of radial spasm appears to be somewhat higher in younger females. Contemporary equipment such as hydrophilic sheaths and our understanding of the methods for the prevention and treatment of radial artery spasm (e.g., intra-arterial administration of calcium channel blockers) has nearly eliminated the occurrence of radial artery spasm.
While the primary focus of advances in transradial procedures has been on arterial access procedures, the same technical advances can be used in the venous circulation. Right heart catheterization and myocardial biopsy can be readily carried out using a forearm approach [33]. Most commonly, venous access is achieved at the level of the antecubital fossa. Likewise, passage of a temporary pacing catheter is also possible. The basilic vein is large and has a caliper in most to accommodate just about any sized device normally used in the venous system. If the shaft length is adequate, venous thrombectomy devices, vena cava filters and other equipment could all be introduced via the forearm. While the use of the forearm for vascular access does not eliminate the radiation risk, it does move the center of attention away from the pelvis. Bleeding is reduced and vascular complications markedly reduced. Moving access to the forearm from the central venous neck veins also removes the risk of pneumo- and hemo-thorax. It should be noted that in parturients, central venous access above the diaphragm is preferred.
Medicine and technology have made significant advances in imaging and intervention that have reduced or eliminated the need for more traditional sources that cause greater risk to the woman and fetus. The modern introduction of the transradial approaches for both diagnosis and intervention now adds an approach to cardiac catheterization that when needed can be applied with less risk to the patient. In the pregnant patient, the benefits of this newer approach extend beyond the standard benefits to include potentially less fetal exposure to radiation and the ability to improve positional comfort to the patient during the procedure. These transradial techniques cannot only be applied for arterial procedures, but also for venous procedures requiring central venous access. This evolution in cardiac catheterization has been recognized in guidelines suggesting the preferential use of transradial techniques in pregnant patients [10] and recently by the European Society of Cardiology, who stated that a transradial approach should be the default approach for all patients where transradial operators are present [37].
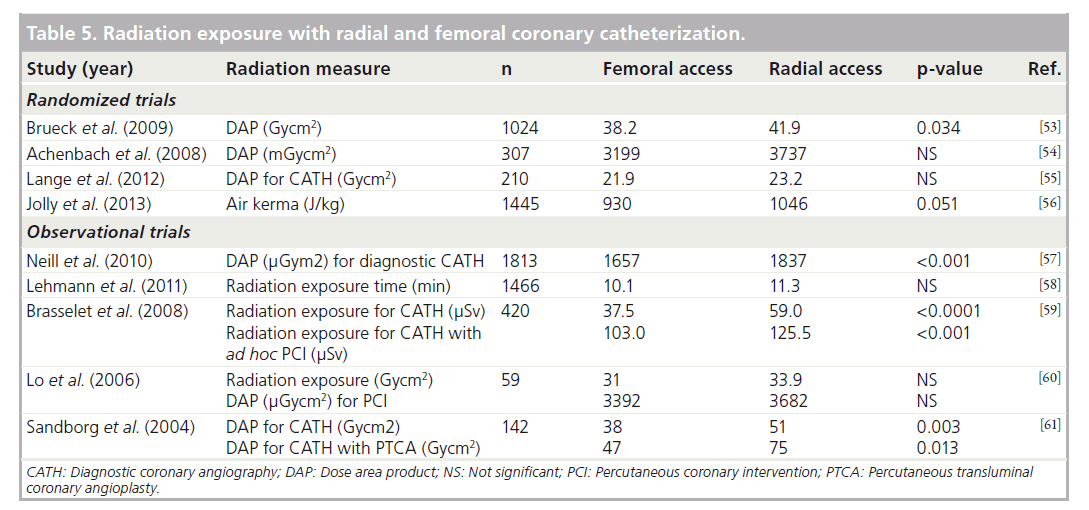
The radiation dose received during radial cardiac catheterization is decreased with higher operator expertise. Left radial approach, compared with right radial approach, is overall associated with somewhat lower radiation doses. It is important to note that fluoroscopy times may be somewhat longer with radial approach compared with femoral approach; cineangiography times are equivalent. The fetus is generally not exposed directly to the x-ray beam during cardiac procedures and mainly receives scatter radiation from the mother. The degree of scatter radiation is similar between the two access routes. Nonetheless, and quite importantly, the radial approach does eliminate the need to perform fluoroscopy of the femoral and iliac vessels and the abdominal aorta that, on occasion, may be required during femoral approach. Representative data with radiation exposure associated with radial exposures are summarized in Table 5. It should be noted that the studies in Table 5 were not performed on parturients and as such may not be directly comparable.
Specific forms of CVD associated with pregnancy
▪ Congenital heart disease
Congenital heart disease may exist in an asymptomatic and/or natural state; it also includes those who may have had congenital heart disease that was surgically repaired or palliated at an earlier age. The surgically corrected patient has not only the possibility of residual effects from the original congenital defect, but also the residual effects from surgical trauma and potentially noncurative surgery that might complicate pregnancy.
A summary of congenital heart disease and primary mode of diagnosis and potential need for radiologic exposure is shown in Table 4. In general, most diagnosis in the present era can be done without x-ray exposure. Abnormal valves, ventricular function and shunts found within the heart should all be readily apparent with ultrasound techniques whether via a transthoracic or transesophageal approach. Complex structural disease can best be sorted out with cardiac MRI and the modern need for diagnostic cardiac catheterization is obviated.
While diagnosis can usually be made without the introduction of x-ray exposure, the patients with congenital heart disease may have a need for intervention related to either arrhythmia or hemodynamic/embolic complications during pregnancy. Different congenital disorders have distinct risks for these complications. Medical therapy to manage these conditions symptomatically may often suffice, but difficult exceptions may arise. Especially problematic may be previously operated or corrected patients who manifest arrhythmia or hemodynamic instability from incomplete repair while pregnant. These individuals may need invasive electrophysiology evaluation/treatment or potentially closure device placement to treat the condition during the pregnancy [38]. Coronary angiography or intervention might potentially be needed in the case of myocardial ischemia.
▪ Valvular heart disease
The primary concern during pregnancy in valvular heart disease is the stenotic valve. With increased vascular volume and cardiac output, fixed office size encountered with either aortic stenosis or mitral stenosis is the most common valvular disease to symptomatically complicate pregnancy. In the industrial world, congenital aortic stenosis is most common of these, while less developed parts of the world or immigrants may manifest stenosis from prior rheumatic disease. Valvular regurgitation is relatively well tolerated during pregnancy and is less problematic, except in extremely rare cases.
Prosthetic cardiac valves may also complicate pregnancy [39]. ECHO may not be very helpful in precisely defining a particular valve and radiography might play a role in precise identification [40]. Most complicating issues with prosthetic valves involve questions of anticoagulation and endocarditis prophylaxis that usually do not require x-ray imaging.
Diagnosis and evaluation of valvular lesions, whether congenital, acquired or prosthetic, can be done with ECHO without the need for cardiac catheterization. While most situations can be managed medically in these patients, there is a growing field of percutaneous technology for treating valvular disease that could potentially be used in pregnant women. Both aortic [41] and mitral balloon valvuloplasty [42] have been available for several decades to alleviate valvular stenosis and require some degree of radiography for placement of catheters [43].
▪ Syndromes of cardiovascular chest pain
Myocardial infarction
Chest pain and symptoms with significant overlap with those associated with MI occur commonly during pregnancy. On most occasions it is not of cardiac origin and a noncardiovascular etiology can be considered. MI during pregnancy is infrequent and has been estimated to occur in 2.8–6.2 per 100,000 deliveries [44,45]. It occurs most often in the third trimester and in the immediate postpartum period. MIs are frequently associated with maternal use of tobacco, hypertension, diabetes, hyper-lipidemia, family history of coronary artery disease and those of African–American or His-panic ethnicity. Maternal mortality from MI in pregnancy has been estimated at 5.1% [45].
Unlike typical MI, in parturients with MI, coronary anatomy demonstrates atherosclerosis in only 40% of patients (type I MI) with spontaneous coronary artery dissection (type II MI) seen in as high as 27% of patients. Coronary arteries considered ‘angiographically normal’ are encountered in approximately 13% of patients [46]. MI with ‘normal’ coronaries seen on angiography is most often associated with coronary artery spasm or coronary embolism. Coronary artery spasm can either be spontaneous, or can be caused by ergonovine or cocaine. In the antepartum period, coronary atherosclerosis is seen more frequently than coronary dissection, which is encountered more frequently during the peripartum period [46]. The very high rate of spontaneous coronary dissection seen in this population has been thought to be due to the hormonal changes of pregnancy. Owing to the uncertainty of etiology, diagnostic coronary angiography may be needed just to confirm diagnosis as therapy can vary significantly depending on etiology.
Modern therapy for acute MI requires rapid reperfusion of the closed coronary vessel. While some success can be obtained with thrombolytic therapy, much better and dependable success is obtained using percutaneous interventional approaches in the catheterization laboratory using x-ray imaging. Radial arterial approach for percutaneous coronary intervention is preferable due to lowered bleeding complications and association with lower mortality in ST-segment elevation myocardial infarction when compared with femoral arterial access [27].
Many of these therapies have unproven track records in pregnancy or will complicate with enhanced bleeding risk, but the net benefit will favor rapid use of the cardiac catheterization laboratory along with x-ray exposure to salvage as much myocardium acutely as possible. X-ray exposure should be minimized without risking success of the procedure, while fallout from medications needed to optimize the longer-term results will need to be managed by the care team afterwards. Survival of the pregnancy is dependent on cardiac salvage, and rapid care must be provided without delays over potential fetal x-ray exposure. With modern equipment, techniques and shielding, fetal x-ray exposure should be contained well within tolerated limits.
Aortic dissection
It has been estimated that half of aortic dissections and ruptures in women younger than 40 years old are associated with pregnancy [47]. Hormonal effects of estrogen have been proposed as putative factors causing weakening of the aortic media and predisposing it to dissection during pregnancy. This tendency may share common pathophysiology with the propensity for coronary artery dissection. Certain other conditions that have been known to be associated with arterial wall abnormalities, such as bicuspid aortic valve disease, discussed previously, and Mar-fan’s Syndrome, are also associated with aortic dissections.
The initial differential and diagnosis of dissection can be usually made with an echocardio-gram. Imaging may also be done with MRI technology if conditions are suitable. Once the diagnosis has been made, there may be a role for CT scanning to rapidly define the extent of disease despite potential radiation burden. Acute dissection can be highly lethal, and precise diagnosis is important and should take precedence.
While therapy for dissection has historically involved a decision between medical or surgical approaches, this is changing. There are a variety of less invasive or percutaneous approaches that have been used or are being developed to contain dissection and aneurysms. These require femoral access and the use of large catheters with x-ray. As aortic dissection is a lethal disease, the x-ray risk should be negligible in comparison with the potential for benefit in such a rare situation.
Pericardial disease
Pericardial disease with fluid accumulation and potentially tamponade is possible from a wide variety of etiologies. Diagnosis is almost universally done by ECHO. Ultrasound can both define the extent of pericardial fluid and whether tamponade physiology is present.
Therapeutic and diagnostic pericardiocentesis or surgical pericardial window can be safely performed during pregnancy. Classically, percutaneous drainage was done using fluoroscopy, but echocardiographic rather than fluoroscopic guidance is preferred as it eliminates radiation exposure and is safer [48]. Currently, most experienced physicians will perform pericardial drainage with the use of ECHO alone, reserving the use of fluoroscopy to manage unforeseen complications that results in pericardial effusions or tamponade.
▪ Cardiomyopathy & heart failure
Cardiomyopathy complicating pregnancy represents a spectrum of diseases ranging from prior disease decompensated by the hemodynamic stress of pregnancy to disease processes that appear distinctly related to the pregnant state. Assessment of ventricular function can easily be done using ECHO technology without the use of x-ray. Where assessment of etiology is required, estimated pulmonary pressures, valvular status, constrictive/restrictive physiology and potential shunt pathology can all be derived using ultrasound. If coronary artery disease is suspected, the definitive diagnosis would be coronary angiography that can be done if necessary. Given the age of these patients, atherosclerotic coronary disease is unlikely and angiography can be limited. Right ventricular biopsy can also be done under ultrasound guidance to avoid x-ray exposure. It is also possible from a forearm approach in addition to jugular or subclavian veins as an alternative to reduce radiation exposure to a minimum over femoral access.
Acute or severely decompensated myopathies may require more aggressive invasive therapy. This could include intra-aortic balloon pumps, extracorporeal membrane oxygenation or other mechanical support devices. These devices with large bore cannulas do require femoral access and care needs to be taken to limit direct-beam exposure to the fetus. Women who need these devices are extremely ill and consequently radiation exposure to the fetus is unavoidable if both are to survive.
▪ Electrophysiological disease
Cardiac rhythm abnormalities are frequently associated with pregnancy. For the majority of times, it is not pathological and is easily controlled with reassurance or simple medication. Rarely, medical therapy may not be enough and invasive, catheter techniques may be indicated.
Atrial dysrhythmia can be cured with ablation techniques. Electrode placement may require some exposure to fluoroscopy [49]. In a similar fashion, ventricular tachycardia, such as that seen originating in a scar from prior corrective congenital heart surgery, may also be very effectively controlled using ablative techniques. The most common techniques presently use radio frequency. Successful catheter-based ablation in pregnant women has been reported with no or minimal radiation exposure [50].
Device therapy may also be needed during pregnancy. Pacemakers for heart block or more complex defibrillators for terminating potentially lethal dysrhythmia may need placement or replacement during pregnancy. Traditional lead placement is with fluoroscopy, but ultra-sound placement can be used to markedly reduce exposure.
Conclusion
Pregnancy associated CVD that requires radiologic intervention or diagnosis is uncommon. A variety of imaging techniques that do not rely on x-ray radiation, such as ultrasound and MRI, have been developed and appear to be safe in pregnancy. Their use has markedly reduced the need for ionizing radiation. When x-ray is needed, a newer approach to cardiac catheterization, known as transradial cardiac catheterization, has become the procedure of choice, both for its overall safety and efficiency in most patients and especially in the pregnant patient.
Classic diseases of young pregnant patients include acquired valvular disease, congenital cardiac abnormalities and myopathic disorders of the heart. Advances have essentially eliminated the need for x-ray-based diagnosis in these patients, but interventional techniques such as valvulo-plasty, closure devices and percutaneous valve implants that may play a role in some of these patients do require the use of x-ray. Coronary disease, whether related to spontaneous dissection or atherosclerosis as the maternal age advances into the early years of coronary disease, also represents a challenge for which x-ray technologies for both diagnosis and intervention still play a critical role. Finally, disorders of cardiac rhythm, with a need for ablation or device therapy, and invasive control of thromboembolic disease with venous filters, are other areas that may intersect with the pregnant population and require x-ray exposure.
While technologies have developed that do not require the risk of x-ray exposure, treatments and the complexity of disease potentially seen in the pregnant patients also continues to evolve. Diagnosis and treatment that required x-ray in the past may be managed without today, but newer forms of therapy have developed that need the energy of x-ray. For this, future improvements in monitoring [51], imaging technologies, and ongoing respect for the ALARA principle will optimize future care.
Future perspective
An expanding population of patients with congenital heart disease growing up to be adults, and the pressure for women at older reproductive ages to conceive, will continue to foster a population of pregnant patients with CVD. Imaging techniques and interventions will evolve that do not require ionizing radiation, but at the same time new interventions may develop to treat pregnancy-associated heart disease that previously had not been considered and requires ionizing radiation exposures. Augmenting new x-ray imaging technology with improved digital image intensifiers, real-time radiation-exposure monitoring with personal dosimeters that will give instantaneous radiation-exposure feedback and encourage minimizing exposure to ionizing radiation. Strict adherence to ALARA principle will remain the cornerstone of any therapeutic and diagnostic procedure requiring ionizing radiation, as even the most optimistic view of the future management of CVD can not completely eliminate the need for x-ray exposure.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
What types of cardiovascular imaging are performed during pregnancy?
▪ Technology that does not use x-ray-ionizing energy includes echocardiography (ECHO) and cardiac MRI; both are extremely safe during pregnancy and have contributed to the reduced need for x-ray exposure.
▪ Imaging technology that uses x-ray is still necessary, despite advances in less risky imaging technologies. Advances in x-ray imaging have actually reduced the radiation exposure to the fetus to very low levels, while operator-driven techniques can further insure lowest exposure possible. The primary use of x-ray energies include placement of devices, such as vena cava filters and electrophysiologic devices, in addition to coronary angiography and interventions for acute coronary syndromes.
Transradial approach to reduce risks of invasive procedures
▪ Advances in catheter technology and miniaturization of equipment has allowed widespread introduction of transradial approaches to both the central arterial and venous system.
▪ This approach potentially reduces x-ray exposure to the fetus by removing the primary x-ray beam from the pelvic region during vascular access. It also allows for improved the positioning of the pregnant patient on the examining table.
▪ Multiple clinical trials have now shown this approach to be superior to transfemoral approaches with regard to vascular complications and blood loss. In acute myocardial infarction, a survival benefit is seen over transfemoral techniques when carried out by experienced operators.
Imaging of specific cardiovascular diseases associated with pregnancy
▪ A broad range of congenital heart disease can be diagnosed and managed with non-x-ray technologies. This advance has been met with a variety of newer interventional techniques, such as occluder devices and valve implants, that continue to require x-ray technologies. The expanding adult population with surgically treated congenital heart disease has resulted in a growing population of patients with rhythm problems originating within the surgical scars that need therapy by electrophysiologists using x-rays.
▪ Valvular disease can usually be diagnosed adequately without x-ray exposure, but interventions of this disease require x-rays to perform balloon angioplasty, valve placement or potentially replacement. Percutaneous approaches to repairing and replacing valves are rapidly being developed and potentially may play an important role in those women who enter pregnancy with valve disease that might otherwise be lethal.
▪ Evaluation of chest pain syndromes is one area that depends highly on x-ray technologies. In particular, the diagnosis and therapy of myocardial infarction and acute syndromes requires rapid utilization of these x-ray technologies. Aortic dissections likewise can be diagnosed at times with ECHO or MRI, but at times, the clinical situation still may require a CT scan with contrast or an aortogram for definitive diagnosis. Pericardial disorders now can be diagnosed with ECHO and treated with ECHO guidance if pericardiocentesis is needed, essentially eliminating the need for x-ray technologies.
▪ Cardiomyopathy and heart failure from a diagnostic viewpoint can be readily managed with ECHO and MRI technologies. There still may be a role for x-ray guidance for myocardial biopsy if needed and cardiac catheterization if the etiology is uncertain. Likewise, some of the newer interventional techniques, such as mechanical support for the circulation used in extremely sick patients, may still need the application of x-ray techniques.
▪ Electrophysiologic disease is an area that is growing with newer invasive techniques to control rhythm disorders and prevent sudden death. While some catheter placement may be done using alternative technologies, the use of x-ray techniques is still needed in many circumstances, such as ablations and complex pacing–defibrillator devices.
Future of x-ray imaging
▪ Technology using nonionizing energies continues to evolve and replace some uses of x-ray, but medical advances in interventional techniques continue to push the demand for the best quality imaging only available from high-energy x-ray equipment and will continue to do so for the foreseeable future.
▪ Continued attention to limiting x-ray exposure of the patient to that needed for as low as reasonably achievable (ALARA), increased sensitivity of imaging chains and real-time x-ray dose monitoring will enhance medical care in the future.
References
Papers of special note have been highlighted as:
• of interest
•• of considerable interest
- Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet. Gynecol. 113(6), 1299–1306 (2009).
- Sliwa K, Hilfiker-Kleiner D, Petrie MC et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur. J. Heart Failure 12(8), 767–778 (2010).
- Warnes CA, Williams RG, Bashore TM et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation 118(23), e714–e833 (2008).
- Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998 to 2005. Obstet. Gynecol. 116(6), 1302–1309 (2010).
- Abello M, Peinado R, Merino JL et al. Cardioverter defibrillator implantation in a pregnant woman guided with transesophageal echocardiography. Pacing Clin. Electrophysiol. 26(9), 1913–1914 (2003).
- Tsang TS, Enriquez-Sarano M, Freeman WK et al. Consecutive 1127 therapeutic echocardiographically guided pericardiocenteses: clinical profile, practice patterns, and outcomes spanning 21 years. Mayo Clin. Proc. 77(5), 429–436 (2002).
- Kanal E, Barkovich AJ, Bell C et al. ACR guidance document for safe MR practices: 2007. AJR Am. J. Roentgenol. 188(6), 1447–1474 (2007).
- Chen MM, Coakley FV, Kaimal A, Laros RK Jr. Guidelines for computed tomography and magnetic resonance imaging use during pregnancy and lactation. Obstet. Gynecol. 112(2 Pt 1), 333–340 (2008).
- Webb JA, Thomsen HS, Morcos SK. The use of iodinated and gadolinium contrast media during pregnancy and lactation. Eur. Radiol. 15(6), 1234–1240 (2005).
- Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). European Heart J. 32(24), 3147–3197 (2011).
- De Santis M, Di Gianantonio E, Straface G et al. Ionizing radiations in pregnancy and teratogenesis: a review of literature. Reprod. Toxicol. 20(3), 323–329 (2005).
- Streffer C, Shore R, Konermann G et al. Biological effects after prenatal irradiation (embryo and fetus). A report of the International Commission on Radiological Protection. Ann. ICRP 33(1–2), 5–206 (2003).
- Damilakis J, Theocharopoulos N, Perisinakis K et al. Conceptus radiation dose and risk from cardiac catheter ablation procedures. Circulation 104(8), 893–897 (2001).
- Goldberg-Stein SA, Liu B, Hahn PF, Lee SI. Radiation dose management: part 2, estimating fetal radiation risk from CT during pregnancy. AJR Am. J. Roentgenol. 198(4), W352–W356 (2012).
- Gupta S, Ettles DF, Robinson GJ, Lindow SW. Inferior vena cava filter use in pregnancy: preliminary experience. BJOG 115(6), 785–788 (2008).
- Wiener RS, Welch HG. Trends in the use of the pulmonary artery catheter in the United States, 1993–2004. JAMA 298(4), 423–429 (2007).
- Belfort MA, Rokey R, Saade GR, Moise KJ Jr. Rapid echocardiographic assessment of left and right heart hemodynamics in critically ill obstetric patients. Am. J. Obstet. Gynecol. 171(4), 88–92 (1994).
- Dabaghi SF, Rokey R, Rivera JM, Saliba WI, Majid PA. Comparison of echocardiographic assessment of cardiac hemodynamics in the intensive care unit with right-sided cardiac catheterization. Am. J. Cardiol. 76(5), 392–395 (1995).
- Vignon P, Aithssain A, Francois B et al. Echocardiographic assessment of pulmonary artery occlusion pressure in ventilated patients: a transoesophageal study. Crit. Care 12(1), R18 (2008).
- Ommen SR, Nishimura RA, Appleton CP et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 102(15), 1788–1794 (2000).
- Vargas F, Gruson D, Valentino R et al. Transesophageal pulsed Doppler echocardiography of pulmonary venous flow to assess left ventricular filling pressure in ventilated patients with acute respiratory distress syndrome. J. Crit. Care 19(3), 187–197 (2004).
- Baggish AL, Boucher CA. Radiopharmaceutical agents for myocardial perfusion imaging. Circulation 118(16), 1668–1674 (2008).
- Rao SV, Cohen MG, Kandzari DE, Bertrand OF, Gilchrist IC. The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J. Am. Coll. Cardiol. 55(20), 2187–2195 (2010).
- Caputo RP, Tremmel JA, Rao S et al. Transradial arterial access for coronary and peripheral procedures: executive summary by the Transradial Committee of the SCAI. Catheter Cardiovasc. Interv. 78(6), 823–839 (2011).
- Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157(1), 132–140 (2009).
- Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 377(9775), 1409–1420 (2011).
- Romagnoli E, Biondi-Zoccai G, Sciahbasi A et al. Radial Versus Femoral Randomized Investigation in ST-Segment Elevation Acute Coronary Syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) Study. J. Am. Coll. Cardiol. 60(24), 2481–2489 (2012).
- Mamas MA, Ratib K, Routledge H et al. Influence of access site selection on PCIrelated adverse events in patients with STEMI: meta-analysis of randomised controlled trials. Heart 98(4), 303–311 (2012).
- Alexander KP, Chen AY, Newby LK et al. Sex differences in major bleeding with glycoprotein IIb/IIIa inhibitors: results from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) initiative. Circulation 114(13), 1380–1387 (2006).
- Ahmed B, Piper WD, Malenka D et al. Significantly improved vascular complications among women undergoing percutaneous coronary intervention: a report from the Northern New England Percutaneous Coronary Intervention Registry. Circ. Cardiovasc. Interv. 2(5), 423–429 (2009).
- Marso SP, Amin AP, House JA et al. Association between use of bleeding avoidance strategies and risk of periprocedural bleeding among patients undergoing percutaneous coronary intervention. JAMA 303(21), 2156–2164 (2010).
- Kwon SW, Cha JJ, Rhee JH. Prone position coronary angiography due to intractable back pain: another merit of transradial approach compared to transfemoral approach. J. Invasive Cardiol. 24(11), 605–607 (2012).
- Gilchrist IC. Radial approach to right heart catheterization and intervention. Indian Heart J. 62(3), 245–250 (2010).
- Pristipino C, Pelliccia F, Granatelli A et al. Comparison of access-related bleeding complications in women versus men undergoing percutaneous coronary catheterization using the radial versus femoral artery. Am. J. Cardiol. 99(9), 1216–1221 (2007).
- Abrams J, Yee DC, Clark TW. Transradial embolization of a bleeding renal angiomyolipoma. Vasc. Endovascular. Surg. 45(5), 470–473 (2011)
- Sharma GL, Loubeyre C, Morice MC. Safety and feasibility of the radial approach for primary angioplasty in acute myocardial infarction during pregnancy. J. Invasive Cardiol. 14(6), 359–362 (2002).
- Hamon M, Pristipino C, Di Mario C et al. Consensus document on the radial approach in percutaneous cardiovascular interventions: position paper by the European Association of Percutaneous Cardiovascular Interventions and Working Groups on Acute Cardiac Care and Thrombosis of the European Society of Cardiology. EuroIntervention 8(11), 1242–1251 (2013).
- Schrale RG, Ormerod J, Ormerod OJ. Percutaneous device closure of the patent foramen ovale during pregnancy. Catheter Cardiovasc. Interv. 69(4), 579–583 (2007).
- Heuvelman HJ, Arabkhani B, Cornette JM et al. Pregnancy outcomes in women with aortic valve substitutes. Am. J. Cardiol. 111(3), 382–387 (2013).
- Bapat V, Mydin I, Chadalavada S, Tehrani H, Attia R, Thomas M. A guide to fluoroscopic identification and design of bioprosthetic valves: a reference for valve-in-valve procedure. Catheter Cardiovasc. Interv. 81(5), 853–861 (2012).
- Bhargava B, Agarwal R, Yadav R, Bahl VK, Manchanda SC. Percutaneous balloon aortic valvuloplasty during pregnancy: use of the Inoue balloon and the physiologic antegrade approach. Cathet. Cardiovasc. Diagn. 45(4), 422–425 (1998).
- De Souza JA, Martinez EE Jr, Ambrose JA et al. Percutaneous balloon mitral valvuloplasty in comparison with open mitral valve commissurotomy for mitral stenosis during pregnancy. J. Am. Coll. Cardiol. 37(3), 900–903 (2001).
- Ribeiro PA, Fawzy ME, Awad M, Dunn B, Duran CG. Balloon valvotomy for pregnant patients with severe pliable mitral stenosis using the Inoue technique with total abdominal and pelvic shielding. Am. Heart J. 124(6), 1558–1562 (1992).
- Ladner HE, Danielsen B, Gilbert WM. Acute myocardial infarction in pregnancy and the puerperium: a population-based study. Obstet. Gynecol. 105(3), 480–484 (2005).
- James AH, Jamison MG, Biswas MS, Brancazio LR, Swamy GK, Myers ER. Acute myocardial infarction in pregnancy: a United States population-based study. Circulation 113(12), 1564–1571 (2006).
- Roth A, Elkayam U. Acute myocardial infarction associated with pregnancy. J. Am. Coll. Cardiol. 52(3), 171–180 (2008).
- Williams GM, Gott VL, Brawley RK, Schauble JF, Labs JD. Aortic disease associated with pregnancy. J. Vasc. Surg. 8(4), 470–475 (1988).
- Callahan JA, Seward JB, Nishimura RA et al. Two-dimensional echocardiographically guided pericardiocentesis: experience in 117 consecutive patients. Am. J. Cardiol. 55(4), 476–479 (1985).
- Ferguson JD, Helms A, Mangrum JM, Dimarco JP. Ablation of incessant left atrial tachycardia without fluoroscopy in a pregnant woman. J. Cardiovasc. Electrophysiol. 22(3), 346–349 (2011).
- Szumowski L, Szufladowicz E, Orczykowski M et al. Ablation of severe drug-resistant tachyarrhythmia during pregnancy. J. Cardiovasc. Electrophysiol. 21(8), 877–882 (2010).
- Chiriotti S, Ginjaume M, Vano E et al. Performance of several active personal dosemeters in interventional radiology and cardiology. Radiat. Meas. 46(11), 1266–1270 (2011).
- Limacher MC, Douglas PS, Germano G et al. ACC expert consensus document. Radiation safety in the practice of cardiology. American College of Cardiology. J. Am. Coll. Cardiol. 31(4), 892–913 (1998).
- Brueck M, Bandorski D, Kramer W, Wieczorek M, Holtgen R, Tillmanns H. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc. Interv. 2(11), 1047–1054 (2009).
- Achenbach S, Ropers D, Kallert L et al. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter. Cardiovasc. Interv . 72(5), 629–635 (2008).
- Lange HW, Von Boetticher H. Reduction of operator radiation dose by a pelvic lead shield during cardiac catheterization by radial access: comparison with femoral access. JACC Cardiovasc. Interv. 5(4), 445–449 (2012).
- Jolly SS, Cairns J, Niemela K et al. Effect of radial versus femoral access on radiation dose and the importance of procedural volume: a substudy of the multicenter randomized RIVAL trial. JACC Cardiovasc. Interv. 6(3), 258–266 (2013).
- Neill J, Douglas H, Richardson G et al. Comparison of radiation dose and the effect of operator experience in femoral and radial arterial access for coronary procedures. Am. J. Cardiol. 106(7), 936–940 (2010).
- Lehmann R, Ehrlich JR, Weber V et al. Implementation of the transradial approach for coronary procedures is not associated with an elevated complication rate and elevated radiation patient exposure. J. Interv. Cardiol. 24(1), 56–64 (2011).
- Brasselet C, Blanpain T, Tassan-Mangina S et al. Comparison of operator radiation exposure with optimized radiation protection devices during coronary angiograms and ad hoc percutaneous coronary interventions by radial and femoral routes. Eur. Heart J. 29(1), 63–70 (2008).
- Lo TS, Buch AN, Hall IR, Hildick-Smith DJ, Nolan J. Percutaneous left and right heart catheterization in fully anticoagulated patients utilizing the radial artery and forearm vein: a two-center experience. J. Interv. Cardiol. 19(3), 258–263 (2006).
- Sandborg M, Fransson SG, Pettersson H. Evaluation of patient-absorbed doses during coronary angiography and intervention by femoral and radial artery access. Eur. Radiol. 14(4), 653–658 (2004).
- US FDA classification of fetal risks due to pharmaceuticals. www.gpo.gov/fdsys/pkg/FR-2008-05-29/pdf/ E8-11806.pdf
- SAFE-PCI for Women. http://clinicaltrials.gov/ct2/show/NCT01406236
- Ludman PF. National Audit of Percutaneous Coronary Interventional Procedures. Annual Report 2011. www.ucl.ac.uk/nicor/audits/adultcardiacintervention/publicreports/documents/pcireport2012
•• Current guidelines for the treatment of adults with congenital cardiac conditions.
•• Comprehensive guidelines for and excellent review of cardiovascular disease treatment in pregnancy.
• Excellent review of radiation effects during pregnancy with an international viewpoint.
• Excellent description of fetal radiation exposure during pregnancy.
• Important concept review of radiation dose management during pregnancy.
• Review of radial approach to coronary intervention.
• Largest and most important contemporary trial of radial coronary intervention.
•• Consensus document of radiation use in cardiology.
▪ Websites