Perspective - Imaging in Medicine (2012) Volume 4, Issue 1
Motor imagery after stroke: where next?
Nikhil Sharma*Human Cortical Physiology & Stroke Neurorehabilitation Section, NINDS, NIH, Building 10, Room 7D50, Bethesda, MD 20892, USA
- Corresponding Author:
- Nikhil Sharma
Human Cortical Physiology & Stroke Neurorehabilitation Section
NINDS, NIH, Building 10, Room 7D50, Bethesda, MD 20892, USA
E-mail: sharmanik@ninds.nih.gov
Abstract
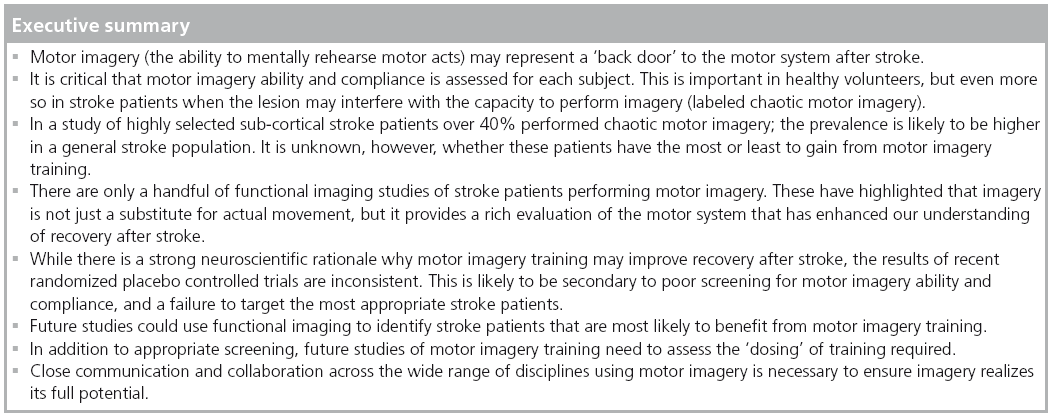
There is considerable interest in using motor imagery to improve recovery after stroke. While motor imagery has a strong neuroscientific rationale, there are significant obstacles to its use and gaps in our knowledge that need to be addressed. Together these may explain the inconsistent results seen in recent randomized placebo-controlled trials of motor imagery training in stroke patients. The first section of this article discusses why assessment of motor imagery ability is crucial when applying motor imagery to stroke patients. Then in the context of current models of recovery after stroke, the second section highlights gaps in the neuroscientific rationale behind the use of motor imagery training. The third section explores the recent randomized trials of motor imagery training in stroke patients and discusses why the findings are inconsistent. Finally, I propose future areas of research that may prove fruitful and will allow motor imagery to fulfill its potential.
Keywords
functional imaging ▪ motor imagery ▪ motor recovery ▪ rehabilitation ▪ stroke
Motor imagery (the ability to mentally rehearse motor acts) is an integral part of the motor system. While it can be applied in a wide range of situations, for instance to train athletes [1], it is the application of motor imagery to stroke patients that I will focus on here. Stroke remains the leading cause of long-term disability and over 795,000 people suffer a stroke in the USA every year [2]. Most stroke patients have persistent deficits in fine motor skills impairing daily activities and independence. Yet even years after stroke, the human brain is capable of reorganizing to improve motor performance [3–6]. Motor imagery may be able to influence this neuroplastic process and therefore reduce the burden of disability in select patients [6–8]. However, there are a number of obstacles when using motor imagery in stroke patients. First, there is a difficulty in objectively identifying patients who can (or cannot) perform motor imagery after a stroke. Second, we have very little information regarding the neural substrates of motor imagery after stroke. I will argue here that these obstacles are likely to have contributed significantly to the lack of functional imaging studies in stroke patients [7] and the inconsistent results derived from clinical trials of motor imagery training [9–11].
Previously, we have suggested that motor imagery may represent a ‘back door’ to the motor system after stroke [7]. In other words it could be used to access the motor system when movement is not possible. Motor imagery is an attractive task as it incorporates voluntary drive (i.e., the subject is actively engaged in the task), which is important in rehabilitation [12]. It is not, in principle at least, dependent upon residual motor function. In other words stroke patients are able to use motor imagery to perform movements that they can no longer physically execute [13]. Furthermore, there is evidence to suggest that motor imagery is a realistic substitute to actual movement [14–16], making it an attractive potential intervention after stroke [6–8].
This perspective has four sections. The first section discusses why it is critical that we objectively assess motor imagery ability in each individual rather than at the group level. The second section discusses the neuroscientific rationale behind the use of motor imagery training in the context of the current models of recovery after stroke. The third section will discuss the recent randomized trials of motor imagery training in stroke patients and discuss why the findings are inconsistent. Finally I will propose areas that I feel need to be investigated over the next decade in order for motor imagery to fulfill its potential.
Assessing motor imagery ability in stroke patients
Motor imagery is entirely covert and therefore it is difficult (though not impossible) to confirm whether the subject is doing what is asked of them. A central question in the use of motor imagery in stroke patients is ‘how do I know that the subject is performing motor imagery?’
To add to this there are different types of imagery (i.e., visual imagery, third person imagery, for examples see [17]). Instructions to the subjects therefore need to be precise. The situation becomes more complex after a stroke when the lesion itself may disrupt the networks required to perform motor imagery. It is perhaps an understatement to say that assessing motor imagery ability and compliance in stroke patients is difficult.
One approach is to use the similarities between motor imagery and actual movement to our advantage. Motor imagery produces similar autonomic changes to movement, with significant increases in heart and respiratory rates observed [14,15,18]. However, it is the accuracy and close temporal coupling between motor imagery and actual movement that is paramount in my opinion, that is, the time taken to mentally perform an action closely mirrors the actual movement [16,19]; this can be preserved after stroke [20]. Importantly, this forms part of Jeannerod’s definition of motor imagery, “the mental rehearsal of a first person action-representation without movement that is confined by the principles of motor control” [21]. The clause restricting motor imagery to comply with the rules of motor control is crucial in successfully applying it to stroke patients as it can be used to objectively check ability and monitor compliance.
Monitoring compliance is particularly important after stroke as depending upon the lesion location, the capacity to perform motor imagery may be disrupted [7]. However, in other chronic disease states temporal coupling is often preserved; in Parkinson’s disease asymmetrical bradykinesia is mirrored during motor imagery [22], as is the performance in chronic fatigue syndrome [23]. Depending on the lesion location after stroke, the ability to perform motor imagery accurately and/or the temporal coupling may be affected. For instance, lesions in the parietal lobe can reduce motor imagery accuracy [24,25], whereas temporal uncoupling may occur after parietal [26] or frontal lobe damage [13], but can be preserved after cerebellar stroke [27].
We use the term ‘chaotic motor imagery’ for cases when the subject ‘breaks the rules’. Chaotic motor imagery is defined as an inability to perform motor imagery accurately, or if accuracy is preserved, the demonstration of temporal uncoupling [7,28–31]. We have designed a simple and rapid assessment that is capable of objectively screening for chaotic motor imagery in individuals (Chaotic Motor Imagery Assessment). Full details of this assessment have been published elsewhere and it is freely available on request [28–31]. The Chaotic Motor Imagery Assessment assesses motor imagery accuracy and then explores the close temporal coupling between motor imagery and actual movement to identify patients performing chaotic motor imagery [7,28– 32]. Importantly, the Chaotic Motor Imagery Assessment assesses whether each patient is performing chaotic motor imagery rather than looking for differences at the group level. An interesting alternative is the Controllability of Motor Imagery Scale [33]; subjects follow a series of instructions, each specifying a single mental movement of a limb, and at the end the subject must assume the position produced by the combination of movements. Those unable to do so are excluded, providing objective evidence of motor imagery ability. Although the use of alternative strategies such as visual imagery is not addressed, it remains a useful assessment.
How prevalent is chaotic motor imagery?
In a study of subcortical stroke patients we reported that 40% of subjects performed chaotic motor imagery [31]. What is surprising is that these subjects were highly selected and had small subcortical lesions that one would not have predicted to interfere with motor imagery ability based upon lesion studies [13,24–26]. In an unrestricted patient population the number of subjects demonstrating chaotic motor imagery ability is likely to be much higher. Therefore in my opinion, owing to the heterogeneous nature of stroke lesions, the first step in assessing motor imagery compliance should be to ask ‘can this patient perform motor imagery?’
Subjective measurements or even objective measures [20,34] of the quality or nature of motor imagery performed at the group level overlook the critical question of whether the individual subjects can perform motor imagery [14,35–37]. Inherently these questionnaires assume that the subject can perform motor imagery. While these measurements are very important and provide useful information, in the specific context of screening for motor imagery ability after stroke, I feel that a dichotomic approach to motor imagery is necessary; able versus unable is required at the subject level at the first instance. Often the lack of significant difference between groups of patients is taken to imply that all subjects were able to perform motor imagery. Of course a ‘lack of a difference’ does not provide any information supporting the statement that all subjects can perform motor imagery. It may be argued that testing at the group level confirms that the number of patients performing chaotic motor imagery is likely to be equal in both interventions. While this may be the case, looking for differences at the group level may provide false comfort as the p‑value would remain nonsignificant even if 40% of the stroke patients included were unable to perform motor imagery. If we are investigating motor imagery, failing to identify a large number of subjects who cannot perform the task makes interpreting the results (or lack thereof) impossible. It should be explicitly stated that subjects performing chaotic motor imagery may have the most to gain from imagery training. Therefore, depending upon the hypothesis being tested, they may not need to be excluded but just identified.
Why could motor imagery improve recovery after stroke?
At the very core of virtually any application of motor imagery to stroke patients (or other patient populations such as those with Parkinson’s Disease [32]) are underlying assumptions about its neural substrates. The assumption is that motor imagery activates the same neural substrates as actual movement after stroke and can therefore be used as an alternative. While the similarities between the neural substrate of motor imagery and actual movement have been documented [7,38–44], there is very little information about the neural substrates of motor imagery in stroke patients. And yet, only by understanding the neural substrate of motor imagery after stroke can we establish in whom it may beneficial. Furthermore, our understanding of the neural substrates of actual movement after stroke is far from complete.
The spontaneous recovery of function after stroke has been studied widely since the emergence of techniques able to probe the human brain in vivo (e.g., functional MRI, EEG, magnetoencephalography and PET) [5]. It has become clear that the primary motor cortex is central to the changes in motor performance, even in healthy volunteers [45]. The models of motor recovery after stroke are almost exclusively based upon actual movement (for more in-depth reviews of this area see [3–6]). Numerous studies now suggest that spontaneous recovery of motor function is accompanied by reorganization in areas remote from the structural damage [5,46–52]. It is the interplay between the two primary motor cortices that has received the most attention [47,51–57]. While in healthy volunteers simple hand movements activate the opposite primary motor cortex (BA4), after stroke, movement of the paretic hand activates a widespread bilateral motor network that includes both primary motor cortices [47,51,53–55]. In other words both the hemisphere affected by the stroke (ipsilesional) and the unaffected hemisphere (contralesional) show movement-dependent changes in blood oxygen level dependence signal. Overall, it appears that the greater the movement-dependent change in activation within the ipsilesional primary motor cortex, the better the recovery of motor performance [47,51,53–55,58]. Thus, stroke patients who have made a near-complete recovery appear to have neural networks that closely resemble healthy volunteers. It stands to reason that interventions capable of normalizing this movementdependent hemispheric imbalance between the motor cortices could improve motor function and a number of studies support this [6,59–68].
The central assumption behind the use of motor imagery training after stroke is that it can drive the imbalance between primary motor cortices to a more physiological state, thus improving motor function. Therefore, one would assume that motor imagery involves the motor cortex; surprisingly the answer is not clear. In healthy volunteers the reported involvement of the primary motor cortex during motor imagery is inconsistent [7,38]. The reports range from no activation of the primary motor cortex [39,40] to transient involvement [41], while others have reported activation less than [42,43] or equal to actual movement [44]. As I have previously discussed elsewhere, a large number of these inconsistencies may be related to difficulties in screening and monitoring compliance [7], but other factors have also emerged. For example, whether subjects are performing predominantly visual imagery or kinesthetic imagery may [69] or may not influence BA4 activity [70]. It has also been suggested that the lack of BA4 activation is a result of suppression by the supplementary motor area [71] but whether this is task dependent is not clear. Motor imagery involves the posterior subdivision of BA4 (labeled BA4p) rather than the anterior subdivision (BA4a), which may also explain some inconsistencies [28]. So is the motor cortex involved in motor imagery?
Despite the variable results, in my opinion there is sufficient evidence to suggest that with appropriate screening of subjects, clear instructions and monitoring of compliance, motor imagery involves the primary motor cortex. This is important because given our current models of motor recovery after stroke there would be little or no neuroscientific rationale for using motor imagery if it did not involve BA4.
Having established that there is a neuroscientific basis for using motor imagery in stroke patients, how are the neural substrates of motor imagery affected by stroke and how do they compare to actual movement? Despite the extensive use of motor imagery in stroke patients across disciplines, we have very little information to answer this question. There are only a handful of studies. Unfortunately, case reports/series of functional imaging of motor imagery after stroke cannot be generalized [72,73] and are of limited use.
We examined well-recovered subcortical stroke patients and as expected, movementdependent activation of the paretic hand appeared normal [31]. By contrast, motor imagery- dependent activation (in the same subjects) highlighted an abnormal hemispheric imbalance within BA4p. Importantly the degree of imbalance correlated with the degree of residual motor impairment [31]. This study, among others, provides further evidence of the importance of BA4p in the recovery process [47,49]. Using structural equation modeling we also reported abnormal interactions between widespread cortical regions, which were again more prominent during motor imagery than actual movement [30]. Again the differences during motor imagery correlated with residual motor impairment. These studies suggest that motor imagery provides additional important information that is functionally relevant but not apparent during studies of actual movement. However, it should be noted that these studies included both subacute and chronic patients, but more importantly all patients had recovered considerable motor function.
There are very few studies of motor imagery in more severely affected stroke patients. A study designed to investigate a magnetoencephalography- based brain–computer interface by Buch et al. reported that completely hemiparetic chronic stroke patients were able to successfully learn to modulate μ‑rhythm (thought to originate from the sensorimotor cortex) to control a cursor and orthotic device [74]. It should be noted that while the study was not intended to focus on motor imagery, and other cognitive processes may have modulated μ‑rhythm, it highlighted a number of important points. While four stroke patients increased μ‑modulation within the ipsilesional motor cortex, training resulted in two patients increasing μ‑rhythm within the contralesional motor cortex. This result should not be overinterpreted but this finding potentially contradicts the current models of recovery after stroke, highlighting the importance of studying the more severely affected stroke population. Buch and colleagues have recently shown that modulation of μ-rhythm depends upon structural and functional connectivity in both ipsilesional and contralesional parietofrontal pathways [75]. Kimberley et al. studied seven stroke patients using motor imagery and reported greater ipsilesional activation within BA4 in the stroke patient group compared with actual movement [76]. There are two important caveats to both of these studies. Neither screened the subjects for motor imagery ability or monitored compliance. In addition, both studies included stroke patients with cortical lesions whereas the models of recovery are largely based upon patients with subcortical lesions.
It should be noted that severely affected stroke patients are often the focus of studies involving brain–computer interfaces and motor training, despite there being virtually no information regarding the underlying neural substrates.
Motor imagery training after stroke
Given the paucity of information regarding the neural substrates of motor imagery, patient selection in motor imagery trials has been largely unrestricted. It is perhaps not surprising that to date there are inconsistent results when motor imagery training has been applied to stroke patients. In recent years there has been a move beyond case reports and randomized placebo controlled trials have emerged.
In a randomized controlled design, Page et al. studied a group of 32 chronic stroke patients (>1 year, mean 3.6 years, no details of lesions given) [11]. The motor imagery tasks used were daily activities (e.g., reaching for and grasping a cup) and the dose of motor imagery was relatively small (30 min per day for 2 days for 6 weeks). Nevertheless they found that motor imagery training versus relaxation (both were combined with a limited amount of physical practice) resulted in significant reductions in arm disability as measured with the Action Research Arm Test and Fugal-Meyer Assessment (upper extremity section). In an elegant study Liu et al. studied the affects of motor imagery training in subacute stroke patients (n = 35, on average 12.2 days poststroke) [10]. They found a significant improvement in both trained and untrained tasks in the motor imagery group (vs conventional rehabilitation). Subjects received daily training for 1 h for 3 weeks (15 h total).
In contrast to the aforementioned studies a recent larger randomized trial found that motor imagery failed to have a beneficial effect on motor performance. Ietswaart et al. studied subacute patients with suspected stroke (<4 months) [9]. A total of 39 patients received 45 min of training versus an attentional control (n = 31) or ‘normal care control’ (n = 32) for 3 days a week for 4 weeks. The authors found that despite adequate powering of the study, they found no effect of training.
It is important to consider why Ietswaart et al. failed to demonstrate a benefit of motor imagery training [9], whereas Page et al. [11] and Liu et al. [10] did. The study by Ietswaart et al. is different from the other studies in a number of ways. For instance, Ietswaart et al. admit that the study aimed to address whether motor imagery training would be effective in all patients with suspected stroke. Thus the patient population included was perhaps more diverse than the other two studies (of note, details of the lesion were lacking). While the patient population in Ietswaart et al. was at a much earlier stage of recovery (<4 months) than Page et al., it was comparable to Liu et al. implying time poststroke is less important. The ‘dose’ of motor imagery varied widely across the three studies. Patients in Liu et al. received the most training (15 h in total), whereas Ietswaart et al. received less (total of 9 h with additional 4 h of independent training) and subjects in Page et al. only received 6 h. However, it should be noted that the intervention in Ietswaart et al. also included action observation and mirror therapy as well. Therefore the dose of supervised motor imagery training was approximately 6 h in total. We do not know whether action observation and mirror therapy are complimentary in this context. It appears therefore that the ideal dose of motor imagery training is critical (i.e., duration, frequency and overall length of training) and needs to be established.
The inclusion of physical practice is another key difference between the studies. In contrast to the study Ietswaart et al., Page et al. and Liu et al. both included a degree of physical practice. The finding by Liu et al. that motor imagery training is more effective than conventional rehabilitation is remarkable in this regard. This raises a critical question: is some form of physical practice required for motor imagery training to be effective? Although evidence is sparse, motor imagery training can independently improve motor performance and produce cortical plastic changes [77], suggesting physical practice is not required but the studies in stroke patients suggest it may be useful.
Where next?
There is a considerable wealth of data supporting the use motor imagery after a stroke, both as a means to evaluate the current state of the motor system and to influence it through training. The few imaging studies of motor imagery after stroke have highlighted that it is not just a substitute to actual movement, but provides a rich evaluation of the motor system. However, it is clear that screening for motor imagery ability is important to both imaging studies and trials of motor imagery training. In the presence of inconsistent results from the randomized trials we need a paradigm shift and need to gather more information to help guide future clinical trials. We need to accept that motor imagery training, like virtually all other interventions after stroke, is likely to be most effective in a subgroup of stroke patients. In other words we need to target the stroke patients that are most likely to benefit from motor imagery training.
Functional imaging studies are likely to provide the necessary information while informing our understanding of the recovery process. There should be a clear focus on using motor imagery to evaluate the neural substrates in the more severely affected stroke population in both the subacute and chronic stage of recovery. Not to say that higher functioning patients would not benefit from further investigation, but as we have virtually no information in the severely affected patient population this is a priority. It is particularly important that functional imaging studies employ adequate measures to screen subjects and monitor compliance. I know of groups who have tried to carry out such work, only to find the data unusable because these precautions were not taken. Not only will this help identify the patients who will benefit from motor imagery training, but it is also likely to change our understanding of the recovery process after stroke.
The randomized trials have highlighted that further work is desperately needed to understand the effect of motor imagery training dose and to establish the effect that additional physical practice has when combined with motor imagery training. Although more randomized trials of motor imagery training may address these points, they would require a large number of patients and if negative may not move the field forward. Establishing the impact of these factors on a surrogate marker such as cortical reorganization (measured using any number of techniques, functional MRI, magnetoencephalography, EEG, transcranial magnetic stimulation) induced by motor imagery training in stroke patients is likely to be more fruitful and allow a more focused clinical trial in the future. Imaging trials therefore need to explore whether the cortical changes induced by motor imagery training are augmented by both the dose of imagery training and the addition of physical practice. This will allow targeting of the most appropriate patients in future randomized placebo control trials of motor imagery training. Of course in the real world, future rehabilitation will not be confined to single interventions. For instance, guided by functional imaging studies, we may find that motor imagery training is effective during the early stages of recovery when movement is difficult but the addition of physical movement produces more desirable effects later on.
In addition to further experiments, and perhaps more importantly, we will require communication and collaboration between research groups. This is particularly important as motor imagery is being used by an ever-increasing number of disciplines. It is important to develop a consensus on the methods and direction of future motor imagery research. For instance, an agreement on the ideal battery of motor imagery tools for screening would be tremendously useful for all involved. Close collaboration would also be required to develop the networks needed to carry out multicenter trials in the future. How this is achieved is not clear but perhaps a cross-discipline motor imagery workshop or small conference would be an appropriate first step.
Acknowledgements
The author would like to thank AD Fourkas for providing comments on an earlier version of this manuscript.
Financial & competing interests disclosure
N Sharma is supported by a competitive NRSA fellowship (NIH). The author has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Murphy SM. Imagery interventions in sport. Med. Sci. Sports Exerc. 26(4), 486–494 (1994).
- Lloyd-Jones D, Adams RJ, Brown TM et al. Heart disease and stroke statistics – 2010 update. Circulation 121(7), e46–e215 (2010).
- Sharma N, Cohen L. Recovery of motor function after stroke. Dev. Psychobiol. doi:10.1002/dev.20508 (2010) (Epub ahead of print).
- Dimyan MA, Cohen LG. Neuroplasticity in the context of motor rehabilitation after stroke. Nat. Rev. Neurol. 7(2), 76–85 (2011).
- Cramer SC. Repairing the human brain after stroke: I. Mechanisms of spontaneous recovery. Ann. Neurol. 63(3), 272–287 (2008).
- Cramer S. Repairing the human brain after stroke. II. Restorative therapies. Ann. Neurol. 63(5), 549–560 (2008).
- Sharma N, Pomeroy VM, Baron JC. Motor imagery: a backdoor to the motor system after stroke? Stroke 37(7), 1941–1952 (2006).
- Lotze M, Cohen LG. Volition and imagery in neurorehabilitation. Cogn. Behav. Neurol. 19(3), 135–140 (2006).
- Ietswaart M, Johnston M, Dijkerman HC et al. Mental practice with motor imagery in stroke recovery: randomized controlled trial of efficacy. Brain 134(Pt 5), 1373–1386 (2011).
- Liu KP, Chan CC, Wong RS et al. A randomized controlled trial of mental imagery augment generalization of learning in acute poststroke patients. Stroke 40(6), 2222–2225 (2009).
- Page SJ, Levine P, Leonard A. Mental practice in chronic stroke: results of a randomized, placebo-controlled trial. Stroke 38(4), 1293–1297 (2007).
- Lotze M, Braun C, Birbaumer N, Anders S, Cohen LG. Motor learning elicited by voluntary drive. Brain 126(4), 866–872 (2003).
- Johnson SH. Imagining the impossible: intact motor representations in hemiplegics. Neuroreport 11(4), 729–732 (2000).
- Roure R, Collet C, Deschaumes-Molinaro C, Delhomme G, Dittmar A, Vernet-Maury E. Imagery quality estimated by autonomic response is correlated to sporting performance enhancement. Physiol. Behav. 66(1), 63–72 (1999).
- Jeannerod M, Frak V. Mental imaging of motor activity in humans. Curr. Opin. Neurobiol. 9(6), 735–739 (1999).
- Decety J, Jeannerod M, Prablanc C. The timing of mentally represented actions. Behav. Brain Res. 34(1–2), 35–42 (1989).
- Kosslyn S, Ganis G, Thompson W. Neural foundations of imagery. Nat. Rev. Neurosci. 2(9), 635–642 (2001).
- Oishi K, Kasai T, Maeshima T. Autonomic response specificity during motor imagery. J. Physiol. Anthropol. Appl. Human Sci. 19, 255–261 (2000).
- Malouin F, Richards C, Desrosiers J, Doyon J. Bilateral slowing of mentally simulated actions after stroke. Neuroreport 15(8), 1349–1353 (2004).
- Malouin F, Richards CL, Durand A, Doyon J. Reliability of mental chronometry for assessing motor imagery ability after stroke. Arch. Phys. Med. Rehabil. 89(2), 311–319 (2008).
- Jeannerod M. Mental imagery in the motor context. Neuropsychologia 33(11), 1419–1432 (1995).
- Dominey P, Decety J, Broussolle E, Chazot G, Jeannerod M. Motor imagery of a lateralized sequential task is asymmetrically slowed in hemi-Parkinson’s patients. Neuropsychologia 33(6), 727–741 (1995).
- De Lange FP, Kalkman JS, Bleijenberg G et al. Neural correlates of the chronic fatigue syndrome – an fMRI study. Brain 127(9), 1948–1957 (2004).
- Tomasino B, Toraldo A, Rumiati RI. Dissociation between the mental rotation of visual images and motor images in unilateral brain-damaged patients. Brain Cogn. 51(3), 368–371 (2003).
- Tomasino B, Rumiati RI, Umilta CA. Selective deficit of motor imagery as tapped by a left-right decision of visually presented hands. Brain Cogn. 53(2), 376–380 (2003).
- Sirigu A, Duhamel JR, Cohen L, Pillon B, Dubois B, Agid Y. The mental representation of hand movements after parietal cortex damage. Science 273(5281), 1564–1568 (1996).
- González B, Rodríguez M, Ramirez C, Sabaté M. Disturbance of motor imagery after cerebellar stroke. Behav. Neurosci. 119(2), 622–626 (2005).
- Sharma N, Jones PS, Carpenter TA, Baron JC. Mapping the involvement of BA 4a and 4p during motor imagery. Neuroimage 41(1), 92–99 (2008).
- Simmons L, Sharma N, Baron J, Pomeroy V. Feasibility study of motor imagery after stroke. Neurorehabil. Neural Repair 22(5), 458–467 (2008).
- Sharma N, Baron JC, Rowe JB. Motor imagery after stroke: relating outcome to motor network connectivity. Ann. Neurol. 66, 604–616 (2009).
- Sharma N, Simmons L, Jones PS et al. Motor imagery after sub-cortical stroke: an fMRI study. Stroke 40(4), 1315–1324 (2009).
- Heremans E, Feys P, Nieuwboer A et al. Motor imagery ability in patients with early- and mid-stage Parkinson disease. Neurorehabil. Neural Repair 25(2), 168–177 (2011).
- Naito E. Controllability of motor imagery and transformation of visual imagery. Percept. Mot. Skills 78(2), 479–487 (1994).
- Malouin F, Richards CL, Durand A, Doyon J. Clinical assessment of motor imagery after stroke. Neurorehabil. Neural Repair 22(4), 330–340 (2008).
- Hall C, Martin K. Measuring movement imagery abilities: a revision of the Movement Imagery Questionnaire. J. Mental Imagery 21, 143–154 (1997).
- Guillot A, Collet C. Contribution from neurophysiological and psychological methods to the study of motor imagery. Brain Res. Rev. 50(2), 387–397 (2005).
- Hall CR, Pongrac J, Buckholz E. The measurement of imagery ability. Hum. Movement Sci. 4, 107–118 (1985).
- Lotze M, Halsband U. Motor imagery. J. Physiol. Paris 99(4–6), 386–395 (2006).
- Hanakawa T, Immisch I, Toma K, Dimyan MA, Van Gelderen P, Hallett M. Functional properties of brain areas associated with motor execution and imagery. J. Neurophysiol. 89(2), 989–1002 (2003).
- Hermes D, Vansteensel MJ, Albers AM et al. Functional MRI-based identification of brain areas involved in motor imagery for implantable brain–computer interfaces. J. Neural Eng. 8(2), 025007 (2011).
- Dechent P, Merboldt KD, Frahm J. Is the human primary motor cortex involved in motor imagery? Cogn. Brain Res. 19(2), 138–144 (2004).
- Porro CA, Francescato MP, Cettolo V et al. Primary motor and sensory cortex activation during motor performance and motor imagery: a functional magnetic resonance imaging study. J. Neurosci. 16(23), 7688–7698 (1996).
- Lacourse MG, Orr ELR, Cramer SC, Cohen MJ. Brain activation during execution and motor imagery of novel and skilled sequential hand movements. Neuroimage 27(3), 505–519 (2005).
- Solodkin A, Hlustik P, Chen EE, Small SL. Fine modulation in network activation during motor execution and motor imagery. Cereb. Cortex 14(11), 1246–1255 (2004).
- Karni A, Meyer G, Rey-Hipolito C et al. The acquisition of skilled motor performance: fast and slow experience-driven changes in primary motor cortex. Proc. Natl Acad. Sci. USA 95(3), 861–868 (1998).
- Calautti C, Baron JC. Functional neuroimaging studies of motor recovery after stroke in adults: a review. Stroke 34(6), 1553–1566 (2003).
- Ward NS, Brown MM, Thompson AJ, Frackowiak RSJ. Neural correlates of motor recovery after stroke: a longitudinal fMRI study. Brain 126(11), 2476–2496 (2003).
- Ward NS, Cohen LG. Mechanisms underlying recovery of motor function after stroke. Arch. Neurol. 61(12), 1844–1848 (2004).
- Loubinoux I, Dechaumont-Palacin S, Castel-Lacanal E et al. Prognostic value of fMRI in recovery of hand function in subcortical stroke patients. Cereb. Cortex 17(12), 2980–2987 (2007).
- Cramer SC, Nelles G, Benson RR et al. A functional MRI study of subjects recovered from hemiparetic stroke. Stroke 28(12), 2518–2527 (1997).
- Grefkes C, Nowak D, Eickhoff S et al. Cortical connectivity after subcortical stroke assessed with functional magnetic resonance imaging. Ann. Neurol. 63(2), 236–246 (2008).
- Talelli P, Greenwood RJ, Rothwell JC. Arm function after stroke: neurophysiological correlates and recovery mechanisms assessed by transcranial magnetic stimulation. Clin. Neurophysiol. 117(8), 1641–1659 (2006).
- Calautti C, Naccarato M, Jones PS et al. The relationship between motor deficit and hemisphere activation balance after stroke: a 3T fMRI study. Neuroimage 34(1), 322–331 (2007).
- Ward NS, Brown MM, Thompson AJ, Frackowiak RSJ. Neural correlates of outcome after stroke: a cross-sectional fMRI study. Brain 126(6), 1430–1448 (2003).
- Tecchio F, Zappasodi F, Tombini M, Caulo M, Vernieri F, Rossini PM. Interhemispheric asymmetry of primary hand representation and recovery after stroke: a MEG study. Neuroimage 36(4), 1057–1064 (2007).
- Murase N, Duque J, Mazzocchio R, Cohen L. Influence of interhemispheric interactions on motor function in chronic stroke. Ann. Neurol. 55(3), 400–409 (2004).
- Duque J, Hummel F, Celnik P, Murase N, Mazzocchio R, Cohen LG. Transcallosal inhibition in chronic subcortical stroke. Neuroimage 28(4), 940–946 (2005).
- Johansen-Berg H, Dawes H, Guy C, Smith SM, Wade DT, Matthews PM. Correlation between motor improvements and altered fMRI activity after rehabilitative therapy. Brain 125(12), 2731–2742 (2002).
- Di Lazzaro V, Pilato F, Dileone M et al. Modulating cortical excitability in acute stroke: a repetitive TMS study. Clin. Neurophysiol. 119(3), 715–723 (2008).
- Talelli P, Greenwood RJ, Rothwell JC. Exploring theta burst stimulation as an intervention to improve motor recovery in chronic stroke. Clin. Neurophysiol. 118(2), 333–342 (2007).
- Khedr EM, Ahmed MA, Fathy N, Rothwell JC. Therapeutic trial of repetitive transcranial magnetic stimulation after acute ischemic stroke. Neurology 65(3), 466–468 (2005).
- Hummel F, Celnik P, Giraux P et al. Effects of non-invasive cortical stimulation on skilled motor function in chronic stroke. Brain 128(3), 490–499 (2005).
- Hummel F, Voller B, Celnik P et al. Effects of brain polarization on reaction times and pinch force in chronic stroke. BMC Neurosci. 7, 73 (2006).
- Hummel FC, Cohen LG. Non-invasive brain stimulation: a new strategy to improve neurorehabilitation after stroke? Lancet Neurol. 5(8), 708–712 (2006).
- Floel A, Hummel F, Duque J, Knecht S, Cohen LG. Influence of somatosensory input on interhemispheric interactions in patients with chronic stroke. Neurorehabil. Neural Repair 22(5), 477–485 (2008).
- Conforto A, Cohen L, Santos R, Scaff M, Marie S. Effects of somatosensory stimulation on motor function in chronic cortico–subcortical strokes. J. Neurol. 254(3), 333–339 (2007).
- Wu CW, Seo HJ, Cohen LG. Influence of electric somatosensory stimulation on paretic-hand function in chronic stroke. Arch. Phys. Med. Rehabil. 87(3), 351–357 (2006).
- Celnik P, Hummel F, Harris-Love M, Wolk R, Cohen LG. Somatosensory stimulation enhances the effects of training functional hand tasks in patients with chronic stroke. Arch. Phys. Med. Rehabil. 88(11), 1369–1376 (2007).
- Guillot A, Collet C, Nguyen VA, Malouin F, Richards C, Doyon J. Brain activity during visual versus kinesthetic imagery: an fMRI study. Hum. Brain Mapp. 30(7), 2157–2172 (2009).
- Fourkas AD, Ionta S, Aglioti SM. Influence of imagined posture and imagery modality on corticospinal excitability. Behav. Brain Res. 168(2), 190–196 (2006).
- Kasess CH, Windischberger C, Cunnington R, Lanzenberger R, Pezawas L, Moser E. The suppressive influence of SMA on M1 in motor imagery revealed by fMRI and dynamic causal modeling. Neuroimage 40(2), 828–837 (2008).
- Butler AJ, Page SJ. Mental practice with motor imagery: evidence for motor recovery and cortical reorganization after stroke. Arch. Phys. Med. Rehabil. 87(12 Suppl. 1), S2–S11 (2006).
- Johnson-Frey SH. Stimulation through simulation? Motor imagery and functional reorganization in hemiplegic stroke patients. Brain Cogn. 55(2), 328–331 (2004).
- Buch E, Weber C, Cohen LG et al. Think to move: a neuromagnetic brain–computer interface (BCI) system for chronic stroke. Stroke 39(3), 910–917 (2008).
- Buch ER, Shanechi AM, Fourkas AD, Weber C, Birbaumer N, Cohen LG. Parietofrontal integrity determines neural modulation associated with grasping imagery after stroke. Brain doi: 10.1093/brain/awr331 (2012) (Epub ahead of print).
- Kimberley TJ, Khandekar G, Skraba LL, Spencer JA, Van Gorp EA, Walker SR. Neural substrates for motor imagery in severe hemiparesis. Neurorehabil. Neural Repair 20(2), 268–277 (2006).
- Jackson PL, Lafleur MF, Malouin F, Richards CL, Doyon J. Functional cerebral reorganization following motor sequence learning through mental practice with motor imagery. Neuroimage 20(2), 1171–1180 (2003).


