News and Views - Imaging in Medicine (2013) Volume 5, Issue 3
New approach to improve x-ray guidance in surgical procedures CT imaging may aid in the prediction of survival in some metastatic melanoma patients Preliminary findings imply microwave tomography suitable to monitor breast cancer treatment response Thalamic atrophy may be a potential biomarker for multiple sclerosis
Sarah Miller*Commissioning Editor, Imaging in Medicine
- Corresponding Author:
- Sarah Miller
Commissioning Editor
Imaging in Medicine
E-mail: s.miller@futuremedicine.com
Abstract
New approach to improve x-ray guidance in surgical procedures
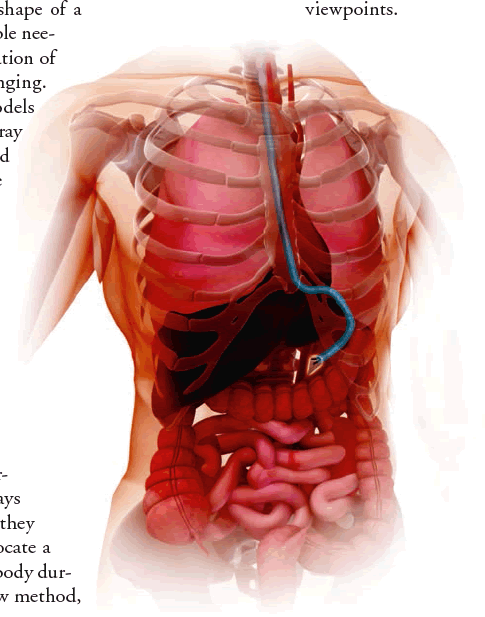
A study presented at the IEEE International Conference on Robotics and Automation (Karlsruhe, Germany) in May has introduced a new method for estimating the shape of a curvilinear device during a minimally invasive surgical procedure using the minimal number of x-ray images (e.g., radiographs or fluoroscopy images). “By minimizing the number of images taken, the level of radiation exposure to the patient is minimized. Accurate estimation of such devices is essential to reduce the risk of possible tissue damage,” explained the study’s lead author Edgar Lobaton, Assistant Professor in the Department of Electrical and Computer Engineering at North Carolina State University (NC, USA), when speaking to Imaging in Medicine.
At present, accurate and continuous estimation of the curvilinear shape of a continuum robot (e.g., a steerable needle or endoscope) over the duration of a surgical procedure is challenging. Currently used kinematics models are imprecise. While multiple x-ray images or CT scans could be used to reconstruct the device’s shape at discrete time points, the risk from ionizing radiation persists. MRI is currently prohibitively expensive for routine use, and other modalities such as 3D ultrasound cannot offer a high enough resolution to accurately track the device.
In response to this problem, Lobaton and his colleagues have developed an algorithm to determine the fewest number of x-rays needed and the angles at which they need to be taken in order to locate a surgical device in the patient’s body during an operation. Using the new method, which has only been used in a simulation environment so far, surgeons enter the procedure type and how precise an estimation they need of the device’s location.
“The technique works by first learning the possible variations on the shape of the device during the execution of the procedure, and then using this model to determine the orientation of an imaging sensor that minimizes uncertainty,” explained Lobaton. “The number of images is selected by ensuring that the expected uncertainty is maintained below the acceptable levels.”
This recently presented study found that obtaining three x-ray images from angles suggested by the new algorithm produced device shape estimation errors significantly lower than using a kinematics model alone or using uniformly spaced viewpoints.
Lobaton and his colleagues now plan to test their method in physical models: “We are working on a physical implementation using phantom tissues. This will allow us to prove the validity of our approach in more realistic scenarios. These techniques could then be used in clinical trials,” detailed Lobaton.
He concluded by telling Imaging in Medicine about how he envisages image guidance in minimally invasive surgery to evolve over the next decade: “In the next 10 years I can imagine an integration between different imaging modalities including noninvasive modalities (such as MRI, x-ray and ultrasound) and imaging data coming for sensors inside the patient (such as an endoscope). We will be able to integrate all this information in real-time providing to the surgeon an accurate 3D model of the patient and a precise localization of the tools used in a procedure. This could enable the use of new methods for enhanced visualization of the imaging data via virtual reality techniques. These advances would lead to safer and more time and cost efficient procedures.”
– Written by Sarah Miller
Sources: Lobaton EJ, Fu J, Torres LG, Alterovitz R. Continuous shape estimation of continuum robots using x-ray images. Presented at: IEEE International Conference on Robotics and Automation. Karlsruhe, Germany, 6–10 May 2013; North Carolina State University news release: http://news.ncsu.edu/releases/ wms-lobaton-xray-2013.
CT imaging may aid in the prediction of survival in some metastatic melanoma patients
Combining the use of CT imaging techniques, along with measurements of baseline lactate dehydrogenase levels in metastatic melanoma patients being treatment with antiangiogenic therapy, has been found, in some instances, to help predict survival.
“This was an exploratory study that was meant to answer a simple hypothesis, that response antiangiogenic therapy could be predicting using CT imaging findings and a serum biomarker,” Andrew Smith of the University of Mississippi (MS, USA) told Imaging in Medicine.
Researchers at the University of Mississippi Medical Center (MS, USA) and at the Ohio State University Comprehensive Cancer Center (OH, USA) analyzed images and data from 46 patients with metastatic melanoma who had been treated with antiangiogenic therapy.
The CT images showed tumor devascularization, as measured by changes in morphology, attenuation, size and structure. These measurements combined with serum lactate dehydrogenase levels were found to prediction both progression-free and overall survival more accurately than either imaging or clinical data alone.
Speaking to Imaging in Medicine, Smith explained the importance of estimating likely success of a therapy in individual patients: “Predicting a favorable response to antiangiogenic therapy is encouraging to patients and their providers. People want to know that their struggle with a new therapy is worth the effort. While we wish all cancer therapies worked all the time for all patients, this isn’t the case. So it’s also important to know when a treatment is likely to fail. This avoids unnecessary toxicities and cost and may improve quality of life and survival by giving the patient and their provider a chance to try a different therapy.”
Smith believes that the study “opens a door to further research into predictive biomarkers that can lead to a definitive answer and to development of a robust tool for predicting survival using readily available techniques (CT imaging and serum biomarkers).”
“You don’t have to cure cancer, you just need to outlive it and maintain your quality of life. Imaging will be the check point for making sure that we can accomplish this goal,” Smith concludes.
– Written by Laura McGuinness
Source: American Roentgen Ray Society press release: www.eurekalert.org/pub_ releases/2013–04/arrs-cas041013.php
Preliminary findings imply microwave tomography suitable to monitor breast cancer treatment response
Recent research from a group at Dartmouth College (NH, USA) has demonstrated that microwave tomography could be suitable to determine the response of breast cancer to treatment.
Microwave tomography provides images of the dielectric properties of tissues. It is low cost and does not carry an exposure risk. Paul Meaney and colleagues longitudinally imaged eight women who were being treated with neoadjuvant chemotherapy for locally advanced breast cancer five- to eight-times during their treatment course. At therapy initiation, they identified regions of interest using contrast-enhanced MRI. During subsequent microwave imaging, microwave property values were obtained from the regions of interest and analyzed to assess short-term (30 days) and longterm (4–6 months) dielectric property changes.
In their results, the group details the cases, one with a complete and one with a partial response, in which the observed microwave changes corresponded with pathologically observed treatment response. High conductivity corresponded with tumors and low conductivity with normal tissue. Normalized mean conductivity in regions of interest was significantly different between complete and partial responders (p = 0.004), and normalized conductivity correlated with complete response (0 = 0.002). The authors report that the results were not affected by BMI, age or breast density.
While these results are preliminary, the authors suggest that “both early and late conductivity property changes correlate well with overall treatment response to neoadjuvant therapy in locally advanced breast cancer. This result is consistent with earlier clinical outcomes that lesion conductivity is specific to differentiating breast cancer from benign lesions and normal tissue.” Meaney also explained the implications of the finding: “Microwave tomography could therefore be used to identify women who are not responding to initial therapy and their treatment changed appropriately at an early stage.”
– Written by Francesca Lake
Source: Meaney PM, Kaufman PA, Muffly SL et al. Microwave imaging for neoadjuvant chemotherapy monitoring: initial clinical experience. Breast Cancer Res. 15(2), R35 (2013).
Thalamic atrophy may be a potential biomarker for multiple sclerosis
Recent research published in Radiology has suggested that there may be a possible association between neurodegeneration of the thalamus and the subsequent development of multiple sclerosis (MS). The team responsible for the study, the result of an international collaboration between various institutions, believes that thalamic degeneration could be used as a biomarker for the neurological condition in future.
To obtain their results, the team studied a cohort of 216 patients diagnosed with clinically isolated syndrome, an initial brief neurological episode experienced by 85% of patients with MS. Every week during the study, the volunteers in the cohort were treated once with 30 μg intramuscular interferon b1a. In addition, MRI was used to examine the appearance and progression of T2 lesions and changes in gray matter volume within various areas of the patients’ brains, first at the beginning of the study and then in 6‑month intervals throughout the next 2 years. Once the study was completed, the researchers used regression and mixed-effect model analyses to formulate their results.
The researchers found that during the 2 years, 92 out of the 216 patients (42.6%) in the cohort developed clinically definite MS. After analyzing the results using multivariate regression analysis, only two of the variables, increase in lateral ventricle volumes and decrease in thalamic volumes, were found to be significantly associated with the development of the disease.
Lead researcher Robert Zivadinov (University at Buffalo, The State University of New York, NY, USA) explained the significance of the findings. He informed Imaging in Medicine that the fact that the development of thalamic and central atrophy were the “only MRI variables associated with conversion to clinically definite multiple sclerosis, whereas the cumulative number of new T2 or contrast agent-enhanced lesions was not retained in the analysis model” was particularly significant. In his view, this finding suggests that “monitoring development of thalamic and central atrophy may be relevant for identifying patients at high risk for conversion to clinically definite MS in future clinical trials involving clinically isolated patients, in addition to counting T2 and contrast agent-enhanced lesions or assessing their volumes.”
His team “strongly believes that use of quantitative MRI in MS, and in particular measurement of thalamic atrophy, may become an important way to select MS patients at higher rate of progression. This, in turn, “could lead to better treatment selection” on an individual basis.
Asked about the need for future research in this area, Zivadinov explained to Imaging in Medicine that the team’s “findings should be reproduced in other studies”, as “the measurement of thalamic atrophy may become an ideal MRI outcome” in MS clinical diagnoses. Furthermore, in future, he believes that “the pathophysiology of thalamic involvement should be further studied.”
– Written by Michael Mansbridge
Source: Zivadinov R, Havrdová E, Bergsland N et al. Thalamic atrophy is associated with development of clinically definite multiple sclerosis. Radiology doi:10.1148/radiol.13122424 (2013) (Epub ahead of print).