News and Views - Imaging in Medicine (2013) Volume 5, Issue 6
New ultrasonography criteria to reduce risk of mistaken diagnoses of nonviable pregnancies PET imaging predicts inoperable lung cancer outcomes New MRI technique able to diagnose Fabry disease New device has potential to reduce false-positives in breast cancer screening Experts devise method to reduce radiation exposure to children requiring repeat CT scans
Abstract
New ultrasonography criteria to reduce risk of mistaken diagnoses of nonviable pregnancies
New diagnostic criteria for the use of ultrasonography published in the New England Journal of Medicine aim to reduce the possibility of physicians identifying a potentially healthy pregnancy as nonviable. The thresholds have been recommended by a panel of 15 experts from the fields of radiology, obstetrics and gynecology, and emergency medicine, convened by the Society of Radiologists in Ultrasound.
The report’s lead author, Peter M Doubilet of Brigham and Women’s Hospital and Harvard Medical School (MA, USA), said: “When a doctor tells a woman that her pregnancy has no chance of proceeding, he or she should be absolutely certain of being correct. Our recommendations are based on the latest medical knowledge with input from a variety of medical specialties. We urge providers to familiarize themselves with these recommendations and factor them into their clinical decision-making.”
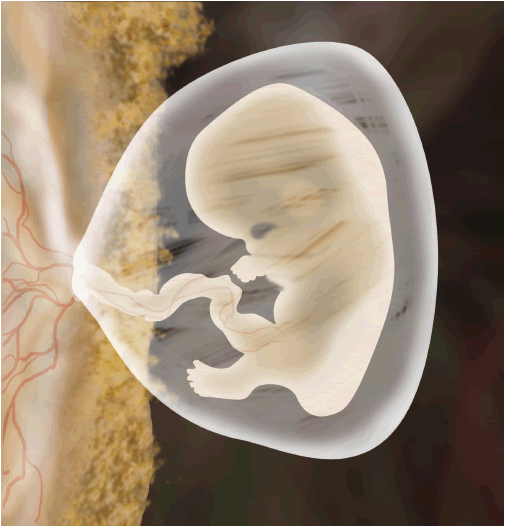
The expert panel made a number of key points, including: the standard for nonviability based on the size of the gestational sac without an embryo should be increased from 16 to 25 mm; the minimum size an embryo can be without exhibiting a heartbeat should be increased to 7 mm, previously if an ultrasound scan revealed that an embryo was larger than 5 mm and did not show a heartbeat it would be classed as nonviable; and the commonly employed ‘discriminatory levels’ of pregnancy blood tests are not reliable for determining nonviable pregnancies. Furthermore, the panel cautioned physicians not to take any action that may damage an intrauterine pregnancy based on the results of only a single blood test and an inconclusive ultrasound on women in a stable condition.
“These are critical guidelines and will help all physicians involved in the care of the emergency patient. They represent an up-to-date and accurate scientific compass for navigating the pathway between opposing forces felt by the emergency physician and his/her consultants who are concerned about the potential morbidity and mortality of an untreated ectopic pregnancy in a patient who may be lost to follow-up, but yet must ensure the safety of an unrecognized early normal pregnancy,” commented Michael Blaivas of the University of South Carolina (SC, USA), a member of the panel.
Kurt T Barnhart of the Perelman School of Medicine at the University of Pennsylvania (PA, USA), another member of the specialist panel, added, “With improvement in ultrasound technology, we are able to detect and visualize pregnancies at a very early age. These guidelines represent a consensus that will balance the use of ultrasound and the time needed to ensure that an early pregnancy is not falsely diagnosed as nonviable. There should be no rush to diagnose a miscarriage; more time and more information will improve accuracy and hopefully eliminate misdiagnosis.”
Source: Doubilet PM, Carol B. Benson CB, Tom Bourne T, Blaivas M; for the Society of Radiologists in Ultrasound Multispecialty Panel on Early First Trimester Diagnosis of Miscarriage and Exclusion of a Viable Intrauterine Pregnancy. Diagnostic criteria for nonviable pregnancy early in the first trimester. N. Engl. J. Med. 369, 1443–1451 (2013).
PET imaging predicts inoperable lung cancer outcomes
A multisite trial published in the Journal of Clinical Oncology and funded by the NCI has revealed a possible application for PET imaging in predicting the aggressiveness of lung cancer tumors and thus identifying which patients need more radical courses of treatment.
“Lung cancer remains the number one cancer killer in the USA. These findings have the potential to give cancer physicians a new tool to more effectively tailor treatments for patients with locally advanced lung cancer.”
Comprising 250 participants at 60 cancer centers throughout the USA, the study investigated the use of 18F-FDG PET in stage III inoperable lung cancer. Patients were scanned before and after a combined treatment regimen of chemotherapy and radiotherapy. Post-treatment scans were found to be predicitive of prognosis as primary tumors with a higher uptake of FDG were more aggressive, increasing the rate of recurrence and reducing the survival rate of patients.
A strong correlation between radiation dose and local control of the cancer was also identified and reinforces the need for further research into radiotherapy delivery for lung cancer.
“Lung cancer remains the number one cancer killer in the USA. These findings have the potential to give cancer physicians a new tool to more effectively tailor treatments for patients with locally advanced lung cancer,” said study author and principal investigator Mitch Machtay of the Case Medical Center (OH, USA), adding, “This is one of the largest studies of its kind to show that PET scans have great potential in predicting the prognosis for patients with inoperable lung cancer … It supports the theory that PET scans add an important new dimension to a physician’s ability to determine which patients need additional cancer therapies to best manage their disease.”
Source: Machtay M, Duan F, Siegel BA et al. Prediction of survival by [18F]fluorodeoxyglucose positron emission tomography in patients with locally advanced non-small-cell lung cancer undergoing definitive chemoradiation therapy: results of the ACRIN 6668/RTOG 0235 trial. J. Clin. Oncol. doi:10.1200/JCO.2012.47.5947 (2013) (Epub ahead of print).
New MRI technique able to diagnose Fabry disease
A novel MRI technique developed by researchers at the University of Alberta (Canada) has shown high sensitivity for the detection of Fabry disease, a rare genetic disorder. The results of the investigation, published in Circulation: Cardiac Imaging, have already led to a change in clinical guidelines in Canada.
Fabry disease is an X-linked liposomal storage disorder characterized by the dysfunctional metabolism of sphingolipids. Symptoms of the disease can be widespread and involve multiple organs. In this particular instance researchers focused on the cardiac complications that occur as a result of build-up of glycolipids in the cardiac muscle.
The technique, known as T1 mapping, was reported to detect microscopic changes in the heart earlier than regular MRI scans or ultrasound. “This test can uniquely identify Fabry disease by detecting microscopic changes in the heart muscle structure that are not visible on regular images,” said lead author Richard Thompson. “Fabry disease can look like other diseases if you only look at the whole heart structure or function, but this T1 mapping test, that can detect the tiniest changes in the heart, could identify all the patients with Fabry disease.”
Gavin Oudit, senior author, also of the University of Alberta, believes it is very likely that this technique will become a key part of the clinical examination of potential Fabry disease patients, advancing clinical care around the world. The sooner the disease can be diagnosed, the sooner treatment can be started and the less damage will be done to the heart. This is of great importance in a population where heart disease is the leading cause of death.
Currently patients suspected of having the disease either need a blood test or, in the case of females, a genetic analysis. The new technique should allow for much quicker and easier diagnosis and, although it won’t reduce the annual US$200,000 cost of treatment, will allow treatment to be started sooner.
Importantly the technique may also be co-opted into other disease diagnoses. Thompson and Oudit are continuing their research in collaboration with UK researchers, and Mauro Chies, of Alberta Health Services, hopes “to be able to advance these sequences on our MRIs in the near future, and look for ways to use it to evaluate and detect other disease conditions.”
Source: Thompson RB, Chow K, Khan A et al. T1 mapping with cardiovascular MRI is highly sensitive for Fabry disease independent of hypertrophy and sex. Circ. Cardiovasc. Imag. 6, 637–645 (2013).
New device has potential to reduce false-positives in breast cancer screening
A joint team of researchers from Brigham Young University (UT, USA) and the University of Utah (UT, USA) have published a report in Magnetic Resonance in Medicine demonstrating a new device to increase the resolution of sodium MRI images of the breast.
Currently breast cancer screening is carried out either by way of a mammography or proton MRI. Although commonplace x-ray mammography can be uncomfortable and any abnormalities that are detected are usually investigated further with a biopsy. Proton MRI scans have increased sensitivity over x-ray mammography and are usually reserved to investigating abnormal areas identified with the more common technique. However, these scans can also result in false-positives and needless biopsy.
The new device builds on a growing area of interest – sodium MRI. Sodium concentrations are thought to increase in malignant lesions, but previously the images produced have not been of highenough quality to challenge other imaging techniques. However, regarding this study, senior author Neal Bangerter said “The images we’re obtaining show a substantial improvement over anything that we’ve seen using this particular MRI technique for breast cancer imaging.” Specifically, the new device is producing images up to fivetimes more accurate than previous sodium MRI methods.
“This development by Dr Bangerter and his group represents a major advance in the field of multinuclear MRI of the breast,” commented Bruce Daniel, Professor of Radiology at Stanford University (CA, USA). “He and his group have invented a way to dramatically boost the sodium signal from the breast, enabling much better, higher resolution sodium MR images to be obtained. This should open the door to new avenues of research into breast cancer.”
With the device taking only 20 min to return high-quality images, Bangerter and his colleagues are hopeful that the device could add an important new dimension to breast cancer screening and provide additional crucial information. “This method is giving us new physiological information we can’t see from other types of images,” Bangerter said. “We believe this can aid in early breast cancer detection and characterization while also improving cancer treatment and monitoring.”
Source: Kaggie JD, Hadley JR, Badal J et al. A 3 T sodium and proton composite array breast coil. Magn. Reson. Med. doi: 10.1002/mrm.24860 (2013) (Epub ahead of print).
Experts devise method to reduce radiation exposure to children requiring repeat CT scans
A team of pediatric neuroradiologists and neurosurgeons have reported in a paper published in Journal of Neurosurgery that they are able to reduce the level of radiation a child is exposed to during repeated CT scanning without compromising diagnostic accuracy.
The technique is extremely simple – the authors recommend reducing the number of slices from the usual 32–40 to just seven. This reduces radiation exposure by an average of 92% compared with normal CT, while still rendering diagnostically relevant images. “The traditional thinking has been that fewer slices would, by definition, mean less clarity and less accuracy, rendering a CT scan suboptimal, but our findings show otherwise,” says lead investigator Jonathan Pindrik (Johns Hopkins University, MD, USA).
The research involved the analysis of CT scans taken of patients being treated for hydrocephalus, otherwise known as water on the brain. The investigators compared two normal CT scans with two low-dose limited-slice scans for 50 patients aged 17 years and younger. In all patients the limited CT technique produced clear and accurate images of the brain ventricles and the resultant images had a high sensitivity (100%) and specif icity (91%) for portraying any changes. The radiation-minimizing protocol did lead to a 4% error rate as two of the 50 cases were ambiguous and generated confusion among the three clinicians tasked with analyzing them. However, the study authors conclude that the limited technique is adequate and would not adversely impact treatment outcomes while significantly reducing total radiation dose.
“We have been searching for ways to minimize radiation exposure in kids without sacrificing the diagnostic accuracy of the images – which is no easy feat – but we believe our limited-slice CT scans achieve that balance,” says senior study investigator Edward Ahn (Johns Hopkins University).
Source: Pindrik J, Huisman T, Mahesh M, Tekes A, Ahn ES. Analysis of limited-sequence head computed tomography for children with shunted hydrocephalus: potential to reduce diagnostic radiation exposure. J. Neurosurg. Pediatr. doi:10.3171/2013.8.PEDS1322 (2013) (Epub ahead of print).
– All stories written by Adam Born.
About the News and Views
The News and Views highlights some of the most important events and research in the field of imaging in medicine. If you have newsworthy information, please contact: Jonathan Wilkinson, Commissioning Editor, Imaging in Medicine, j.wilkinson@futuremedicine.com


