News and Views - Imaging in Medicine (2010) Volume 2, Issue 2
News & Views in ... Imaging in Medicine 2:2
Abstract
Breast cancer screening study EVA: results published
Results from the EVA trial demonstrate that MRI screening with mammography or ultrasound do not find breast cancer any earlier than MRI alone. In the prospective, multicenter, observational, cohort study, four methods for breast cancer screening were studied. The four methods investigated were clinical breast examination, mammography, ultrasound and qualityassured breast MRI; the techniques were studied alone and in various combinations.
The study, carried out between 2002 and 2007, found that ultrasound and mammography have similar cancer-detection rates: 6.0 out of 1000 for ultrasound and 5.4 out of 1000 for mammography. Although combining these two methods increased detection to 7.7 out of 1000, this was not significant. However, the cancer-detection rate for MRI alone was 14.9 out of 1000, significantly higher than the rates for the other screening methods. Crucially, neither the addition of mammography nor ultrasound to MRI significantly improved the number of cancers detected. MRI plus mammography yielded 16.0 cancers out of 1000, while MRI plus ultrasound yielded the same number of cancers as MRI alone. The authors discuss the positive predictive value for mammography, ultrasound and MRI and found it to be 39, 36 and 48%, respectively. From these results, the authors concluded “in women at elevated familial risk, quality-assured MRI screening shifts the distribution of screen-detected breast cancers toward the preinvasive stage. In women undergoing quality-assured MRI annually, neither mammography, nor annual or half-yearly ultrasound or clinical breast examination will add to the cancer yield achieved by MRI alone.”
Of the 27 breast cancers diagnosed during the study, all were detected during annual screening rather than at biannual ultrasound checks. Only asymptomatic women at high risk of developing breast cancer were included in the study; women were determined to be at high risk if their familial lifetime risk was 20% or greater. A total of 687 such women participated in the study, and 1679 screening rounds took place. Additionally, 371 women also had a biannual ultrasound and clinical breast examination.
Current guidelines support mammography as the main method for breast cancer screening, with MRI as a supplementary screening modality. However, results from this EVA trial suggest that where MRI is available, there is little need for mammography screening as well. Lead author C Kuhl, from the University of Bonn (Bonn, Germany) calls for a revision of current breast cancer screening guidelines and emphasizes “the radiation dose associated with regular mammographic screening is clearly acceptable and safe. However, regular mammographic screening usually starts at age 40–50.” Kuhl explains that guidelines to start regular mammographic screening from age 25–30 years alters the situation, “not only because these women will undergo more mammograms and therefore will experience a cumulative lifetime radiation dose that will be substantially higher, but also because the breast tissue of young women is more vulnerable to the mutagenic effects of radiation. Accordingly, we impose more radiation on less radiation-tolerant breast tissue for a very limited, if any, diagnostic benefit.”
Source: Kuhl C, Weigel S, Schrading S et al.: Prospective multicenter cohort study to refine management recommendations for women at elevated familial risk of breast cancer: the EVA trial. J. Clin. Oncol. (2010) (Epub ahead of print).
Ultrasound for the treatment of brain hemorrhage
Details of the study were presented at the American Heart Association’s International Stroke Conference in San Antonio (TX, USA , 23–26 February 2010). A total of 33 patients took part in the study, conducted by researchers from the Swedish Neuroscience Institute (Seattle, WA, USA) and the Johns Hopkins University Medical School (Baltimore, MD, USA). All the patients taking part in the Safety of Lysis with Ultrasound in the Treatment of Intracerebral and Intraventricular Hemorrhage (SLEUTH) study had spontaneous intracerebral hemorrhage.
“...the more quickly a clot can be removed the better, and hours count ... the most surprising thing we discovered was how rapidly the hemorrhage disappeared with ultrasound.”
The treatment required placement of a burr hole, once this was in place, a GPS- like system (STEALTH) was used to direct the ultrasound and drainage catheter into the hemorrhage. Thrombolytic drug tissue plasminogen activator was given for 24 h, administered as the ultrasound was delivered to the hemorrhage.
David Newell, co-executive director of the Swedish Neuroscience Institute comments “the more quickly a clot can be removed the better, and hours count. A minimally invasive treatment approach that combines catheter-delivered ultrasound in conjunction with a clot-busting drug was used.” Newell continues “the most surprising thing we discovered was how rapidly the hemorrhage disappeared with ultrasound. There were virtually no side effects, such as site infections or bleeding, during or after treatment.”
Those involved in the study call for a multicenter trial for safety with a redesigned catheter.
Newell said the results are encouraging “this has great potential to address the problem without cranial surgery.”
Source: International Stroke Conference. TX, USA, 23–26 February 2010: http://stroke conference.americanheart.org
Contrast-enhanced MRI to assist arthritis diagnosis
A study investigating the potential for contrast-enhanced MRI to differentiate between psoriatic and rheumatoid arthritis has been published in the March issue of the American Journal of Roentgenology. The use of contrast agents with MRI can improve the visualization of tissues. Scientists from the University Hospital of Tübingen (Tübingen, Germany) have examined 31 patients with rheumatoid arthritis and 14 patients with psoriatic arthritis in a 3 T whole-body MR unit. All participants were injected with a contrast medium, and the uptake time in the synovial tissue was measured. From this data, gained uptake curves were drawn, and from these the relative enhancement rate was calculated after 35 s, 52 s, 3 min and 15 min. Any enhancements at 35 and 52 s were deemed early, and any enhancement at 15 min was considered late. These dynamic contrast-enhanced MRI rates were compared with laboratory and clinical data. The relative enhancement rate between the two groups after 15 min was found to be statistically significant (p < 0.01). However, no difference in relative enhancement rate was found between the two groups at 35 s, 52 s or 3 min following contrast agent injection, (p = 0.695, p = 0.573 and p = 0.278, respectively). The authors therefore conclude “15 minutes after contrast injection, a statistically significant difference between rheumatoid arthritis and psoriatic arthritis was found in synovial enhancement that might play an important role in differentiating the two diseases.”
Lead author of the study, N Schwenzer, from the University Hospital of Tübingen, explains the need for a technique that differentially diagnoses between the two types of arthritis “clinically, it may be difficult to distinguish psoriatic arthritis from rheumatoid arthritis because the symptoms of both diseases are similar and the diagnostic tests currently available to aid in the differentiation of psoriatic and rheumatoid arthritis are not always sufficient.” She continues “our study revealed a significant difference in perfusion between those patients with rheumatoid arthritis and psoriatic arthritis after 15 minutes. However, since it was a small group of patients and there was an overlap in perfusion values between both types of arthritis, a diagnosis could not be led by contrastenhanced MRI alone. Our results are nonetheless promising though.”
Source: Schwenzer NF, Kötter I, Henes JC et al.: The role of dynamic contrast-enhanced MRI in the differential diagnosis of psoriatic and rheumatoid arthritis. AJR Am. J. Roentgenol. 194(3), 715–720 (2010).
Nanosized imaging of cardiomyocytes
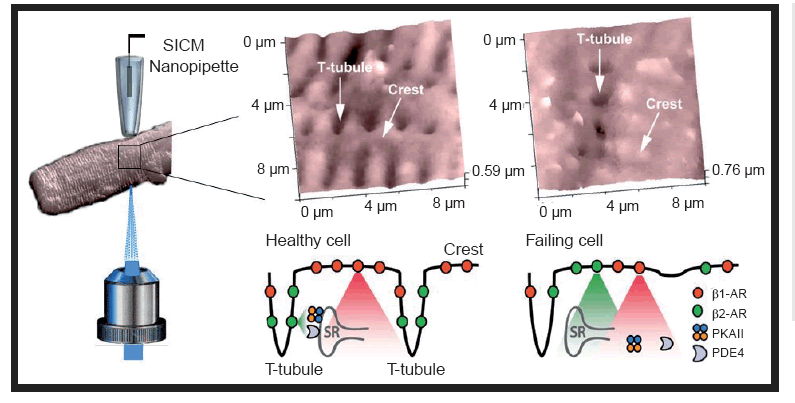
Scientists have reported signaling differences between the cardiac cells of a rat model of chronic heart failure and the cardiac cells of healthy rats. The differences lie in the spatial distribution of the β2-adrenergic receptors (β2-ARs). The researchers, from Imperial College London (London, UK), found that in the cardiomyocytes of healthy adult rats, the β2-ARs are localized exclusively to the deep transverse tubules. However, in the rat model of chronic heart failure, the β2-ARs are situated on the cell crest. This difference in location of the β2-ARs has large implications for the cellular signaling pathways of the cardiomyocyte. In the chronic heart disease model, this redistribution led to diffuse receptor-mediated cAMP signaling. The authors hypothesize that this contributes to the failing myocardial phenotype.
Although β1-ARs and β2-ARs are known to mediate distinct effects on cardiac function, the effect of the spatial localization of b-ARs is less documented. The b-ARs regulate the production of the cAMP and are coupled to the G protein.
Using state-of-the-art technology developed at Imperial College London, the researchers combined nanoscale live-cell scanning ion conductance and fluorescence resonance energy transfer microscopy techniques to carry out the study protocol. The technique enables the surface of individual cardiomyocytes to be imaged in unprecedented detail, providing the researchers with a unique insight into the components of the cell.
Corresponding author Julia Gorelik comments “our new technique means we can get a real insight into how individual cells are disrupted by heart failure. Using our new nanoscale live-cell microscopy we can scan the surface of heart muscle cells to much greater accuracy than has been possible before and to see tiny structures that affect how the cells function.”
It is hoped that the findings will lead to improvements in therapeutics for heart failure and abnormal heart rhythms. In particular, the research may have implications for the design of b-blockers. Gorelik explains “through understanding what’s happening on this tiny scale, we can ultimately build up a really detailed picture of what’s happening to the heart during heart failure and long term, this should help us to tackle the disease. The main question for our future research will be to understand whether drugs can prevent the β2-AR from moving in the cell and how this might help us to fight heart failure.”
Source: Nikolaev VO, Moshkov A, Lyon AR et al.: b2-adrenergic receptor redistribution in heart failure changes CAMP compartmentation. Science (2010) (Epub ahead of print).
SICM images of cardiomyocytes. A healthy heart muscle cell, shown on the left, has specialized structures, t-tubules, that allow b2AR to localize properly and signal through SR, PAKII and PDE4 permitting correct regulation of heart contraction. On the right, the damaged cell has lost most of its t-tubules and b2AR appear on the entire cell surface, which prevents adequate signaling and leads to disregulated heart beating.