Case Report - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 3
Occurrence of cervical spine arthritis with prominent bone edema highly responsive to adalimumab in a patient with psoriatic peripheral arthritis and long-standing remission
- Corresponding Author:
- Maria Concetta Miceli
Rheumatology Unit
Villa Sofia-Cervello United Hospital, Palermo, Italy
E-mail: maricmiceli@gmail.com
Abstract
Cervical spine involvement frequently occurs in patients with psoriatic arthritis (PsA) even in absence of sacroiliitis. Long disease duration, high disease activity in the first five years and presence of peripheral involvement are all predictors of this peculiar articular involvement. We describe the case of a PsA patient, with an initial oligoarthritis pattern of disease highly responsive to etanercept monotherapy and long-standing clinical remission, who developed cervical spine involvement with bone marrow edema of odontoid process and early atlo-axial instability. Notably, he did not exhibit any other clinical symptom or sign of disease activity and was highly responsive to switching to a second anti-TNF drug (adalimumab). The case stresses the importance of strict monitoring PsA patients and considering the possible changing pattern of disease. Early identification of cervical spine involvement requires proper use and interpretation of imaging techniques. Interestingly different articular manifestations of PsA may show different response to therapy even in the same patient.
Keywords
psoriatis arthritis • magnetic resonance imaging • tumor necrosis factor inhibitors
Introduction
Psoriatic arthritis (PsA) is a heterogeneous disease with different patterns of joint involvement that can also change over time [1,2]. Cervical spine involvement is rather common and has been reported in 35-75% of patients [3]. Typical cervical spine lesions are apophyseal joint erosions, vertebral plate erosions and atlantoaxial subluxation using conventional radiography and some studies have shown a very similar pattern to that observed in patients with rheumatoid arthritis [4]. According to Blau and Kaufman classification [5], PsA patients can be divided in patients with inflammatory involvement (erosions and/or subluxations evidence), patients with cervical ankylosing disease (apophyseal joint sclerosis or fusion, anterior or posterior calcification, and/or syndesmophyte formation), and patients with normal cervical spine radiograph. Long disease duration, active disease and the presence of peripheral involvement have all been reported as predictors of cervical spine involvement [3], which does not seem related to severity of skin or nail disease [6] and can often occur in patients with normal sacroiliac joints [3].
Therapeutic management of PsA is challenging due to its clinical heterogeneity and treatment recommendations are focused on preliminary identification of the prevalent pattern of disease [7]. The ultimate goal of therapy should be to achieve remission or low disease activity in all domains in order to improve quality of life and prevent structural damage. Patient assessment should be multidisciplinary and treatment individualized, taking into account disease activity as well comorbidity and previous therapy. A key-point is that optimal care in an iterative process.
Anti-TNF therapy should be used in PsA patients with peripheral arthritis not responsive to first-line therapy with synthetic disease-modifying anti-rheumatic drug (DMARDs) as well as in those with axial disease not responsive to Non-Steroidal Anti- Inflammatory Drugs (NSAIDs) [7]. Observational and real life data support switching to a second anti-TNF as a therapeutic option in patients non responsive to a first anti-TNF drug [8-12]. We describe a woman with PsA and peripheral oligoarthritis at presentation, with long-standing remission while on etanercept therapy, who developed cervical spine disease and was highly responsive to switching to adalimumab.
Case report
A 67-year old woman presented at her scheduled outpatient control on February 2019 complaining of progressive inflammatory cervical pain with morning stiffness and limited rotation in all planes. She had been diagnosed of palmo-plantar psoriasis about 20 years earlier and of peripheral arthritis involving knees and wrists about 10 years after. Her siblings had skin psoriasis and her medical history was remarkable for hypertension and chronic obstructive pulmonary disease. Rheumatoid factor and anti-citrullinated peptide antibody were negative.
According to CASPAR criteria [1] she had been classified as peripheral psoriatic arthritis. At the beginning she was successfully treated with Methotrexate (MTX) 15 mg weekly. In 2013 MTX was stopped due to gastrointestinal intolerance and partial loss of efficacy. We started monotherapy with etanercept 50 mg weekly which achieved rapid and sustained articular and cutaneous remission. Notably our patient had never complained of spine pain nor showed radiographic sacroiliitis.
On February 2019, she unexpectedly developed severe cervical pain with frequent awakenings in the night and prolonged morning stiffness. These symptoms had started suddenly, in the absence of any precipitating factors and without fever or decline in general condition. On clinical examination, neck mobility was severely impaired with limited rotation (~40°) on both sides. There were no symptoms or signs of peripheral arthritis or enthesitis, neither low back pain. Neurological examination was normal. Laboratory examination showed elevated signs of inflammation: Erythrocyte Sedimentation Rate (ESR) was 77 mm/h and C-Reactive Protein (CRP) was 12 mg/l, with normal blood count.
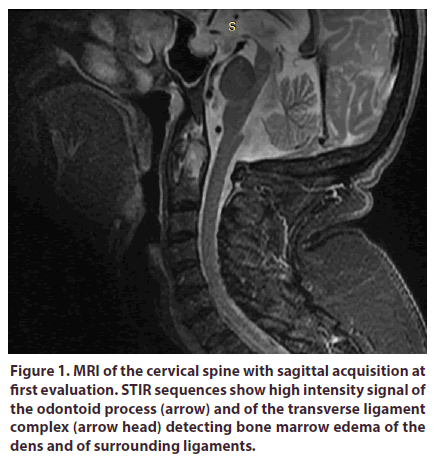
NSAIDs treatment was started with diclofenac 150 mg daily with no clinical response and then with meloxicam 15 mg daily with marginal pain relief. A Magnetic Resonance Imaging (MRI) with T2-STIR sequence of the cervical tract was performed, which showed high hyperintensity signal of the odontoid process and thickening of soft tissue around the atlanto-epistrophic joint, indicating bone edema of the dens and associated synovitis (Figure 1).
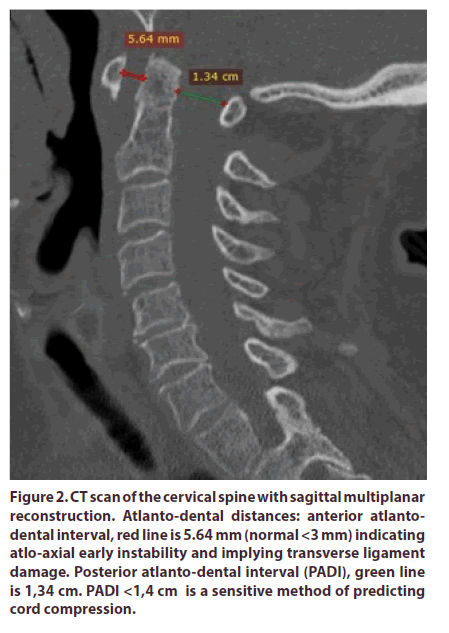
Computed Tomography (CT) with sagittal reconstruction of the atlantoaxial joint was also performed showing no erosions nor destructive lesions of the odontoid cortical bone. There were an anterior atlanto-dental interval of 5.6 mm (indicating early instability) and a Posterior Atlanto-Dental Interval (PADI) of 13,4 mm; notably a PADI < 14 mm is a sensitive method of predicting cord compression and a reliable method to identifying high risk patients who should be further assessed with MRI [13,14]. Degenerative disk disease from C5 to C7 was also visualized (Figure 2).
Figure 2: CT scan of the cervical spine with sagittal multiplanar reconstruction. Atlanto-dental distances: anterior atlantodental interval, red line is 5.64 mm (normal <3 mm) indicating atlo-axial early instability and implying transverse ligament damage. Posterior atlanto-dental interval (PADI), green line is 1,34 cm. PADI <1,4 cm is a sensitive method of predicting cord compression.
A comprehensive clinical and serological evaluation ruled out infections or neoplastic disease. On May 2019 our patient was still complaining of severe cervical pain. Etanercept was stopped and adalimumab 40 mg every two weeks was started. After one month, cervical pain had significantly decreased and one month later it had completely remitted, with gain in bilateral cervical rotation (80°) and normalization of ESR and PCR.
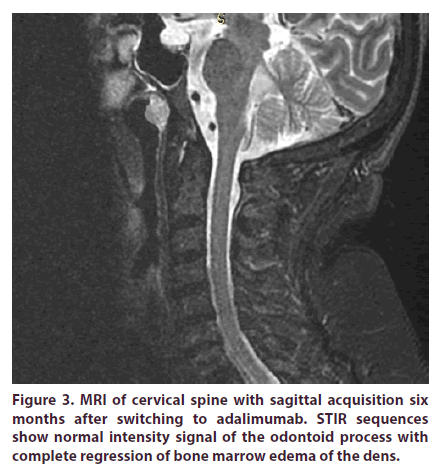
A follow up MRI was performed six months after starting adalimumab therapy and showed bone marrow edema disappearance from the odontoid process with normal signal intensity in STIR weighted sequence (Figure 3). After nine months our patient is still on Adalimumab therapy and persistent clinical remission.
Discussion
PsA is a heterogeneous disease and in its natural history pattern of joint involvement may change [1,2,7]. Cervical spine arthritis is not uncommon, may occur without other signs of spondylitis and may be clinically relevant with 7-21% of patients developing anterior atlantoaxial subluxation [3,15]. Conventional radiography discloses different lesions that are sometimes similar to that observed in rheumatoid arthritis with periodontoid synovial pannus mass, few cases of atlantoaxial subluxation and erosions of odontoid process [3,15-18].
In our patient we observed the acute onset of cervical pain occurring many years after diagnosis. She was on etanercept monotherapy and long-standing remission, without any sign of peripheral arthritis or psoriatic skin lesions. Notably, cervical pain was associated with marked elevation of ESR and CRP, as reported in other studies with cervical spine spondylitis due to PsA [5,18]. We performed an exhaustive imaging evaluation which disclosed inflammatory lesions and early atlantoaxial instability, implying transverse ligament damage.
Moreover, MRI showed intense bone edema of the odontoid process and of the transverse ligament complex with surrounding synovitis. Our findings support the hypothesis that in PsA different pathogenic mechanisms may play a role in cervical involvement and the primum movens could be bone edema of the odontoid process (rather than synovial pannus as observed in rheumatoid arthirtis) or entheseal involvement of the transverse or alar ligaments (as generally occur in spondyloarthropaties).
Conclusion
Early occurrence of atlo-axial instability in a patient on apparent disease remission highlights the importance of prompt assessment of cervical pain in PsA using adequate imaging techniques. In our patient there was no response to adding NSAIDs to etanercept therapy and we decided to switch to adalimumab with rapid clinical response of cervical symptoms and persistent remission of peripheral arthritis. Moreover, MRI confirmed the complete regression of bone edema of the cervical joint. The unusual course of symptoms and response to treatment of this case confirm that PsA is a protean disease and any patient may need an individualized diagnostic and therapeutic approach.
Contributorship
Maria Concetta Miceli made substantial contributions to the analysis and interpretation of data and drafted the manuscript. Livia Bruno collected, edited and analyzed the images. Chiara Arcuri participated in the collection and analysis of data. Giuseppe Provenzano participated in the collection, analysis and interpretation of data and contributed to draft the manuscript.
Competing interest
Maria Concetta Miceli served as advisory board member and/or received lecture grants from Sanofi, Novartis,UCB, Roche, BMS, Lilly. Chiara Arcuri served as advisory board member and/or received lecture grants from Celgene, Roche, UCB, Novartis, MSD, BMS. Giuseppe Provenzano served as advisory board member and/or received lecture grants from AbbVie, Biogen, BMS, Grunenthal, Lilly, MSD, Roche, Sandoz, Sanofi, UCB.
Acknowledgements
None.
Funding
None.
Patient consent
Obtained.
Data sharing statement
No additional data are available.
References
- Taylor W, Gladman D, Helliwell P et al. and the CASPAR Study Group. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis. Rheum 54(8), 2665–2673 (2006).
- Gladman DD. Psoriatic arthritis. Rheum. Dis. Clin. North. Am. 24(4), 829–844 (1998).
- Salvarani C, Macchioni P, Cremonesi T et al. The cervical spine in patients with psoriatic arthritis: a clinical, radiological and immunogenetic study. Ann.Rheum. Dis. 51(1), 73–77 (1992).
- Van Tilt I, Lories R J, Westhovens R et al. Unusual cervical spine involvement in psoriatic arthritis: a case series. Clin. Rheumatol. 28(11), 1343–1346 (2009).
- Blau R H, Kaufman R L. Erosive and subluxing cervical spine disease in patients with psoriatic arthritis. J. Rheumatology. 14, 111–117 (1987).
- Bobek D, Babić-Naglić D, Potocki K et al. The cervical spine involvement in patients with psoriatic arthritis. Reumatizam. 54(1), 12–15 (2007).
- Coates LC, Kavanaugh A, Mease PJ et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 Treatment Recommendations for Psoriatic Arthritis. Arthritis. Rheum. 68, 1060–1107 (2016).
- Glintborg B, Ostergaard M, Krogh NS et al. Clinical Response, Drug Survival, and Predictors thereof in 548 Patients With Psoriatic Arthritis Who Switched Tumor Necrosis Factor α Inhibitor Therapy: Results From the Danish Nationwide DANBIO Registry. Arthritis. Rheum. 65(5), 1213–1223 (2013).
- Saad AA, Ashcroft DM, Watson KD et al. British Society for Rheumatology Biologics Register Persistence with anti-tumour necrosis factor therapies in patients with psoriatic arthritis: observational study from the British Society of Rheumatology Biologics Register. Arthritis. Res. Ther. 11(2), R52 (2009).
- Coates LC, Cawkwell LS, Ng NW et al. Sustained response to long-term biologics and switching in psoriatic arthritis: results from real life experience. Ann. Rheum. Dis. 67(5), 717–719 (2008).
- Jani M, Macphie E, Rao C et al. Effectiveness of switching between biologics in psoriatic arthritis- results of a large regional survey. Clin. Med (Lond). 14(1), 95–96 (2014).
- Kristensen LE, Lie E, Jacobsson LT et al. Effectiveness and feasibility associated with switching to a second or third tnf inhibitor in patients with psoriatic arthritis: a cohort study from Southern Sweden. J. Rheumatol. 43(1), 81–87 (2016).
- Roche CJ, Eyes BE, Withehouse GH. The rheumatoid cervical spine: signs of instability on plain cervical radiographs. Clin. Radiol. 57(4), 241–249 (2002).
- Ramos-Remus C, Gomez-Vargas A, Guzman-Guzman JL et al. Frequency of atlantoaxial subluxation and neurologic involvement in patients with ankylosing spondylitis. J. Rheumatol. 22, 2120–2125 (1995).
- Ouedraogo DD, Palazzo E, Nlome-Nze M et al. Predominant cervical involvement in patients with psoriatic arthritis: report of two cases. Joint. Bone. Spine. 74(2), 175–178 (2007).
- Quarta L, Corrado A, Melillo N et al. Cervical myelopathy caused by periodontoid synovial pannus in a patient with psoriatic arthritis: a case report. Clin. Rheumatol. 26(8), 1380–1382 (2007).
- Lu K, Lee TC. Spontaneous regression of periodontoid pannus mass in psoriatic atlantoaxial subluxation. Case report. Spine. 24(6), 578–581 (1999).
- Laiho K, Kauppi M. The cervical spine in patients with psoriatic arthritis. Ann. Rheum. Dis. 61(7), 650–652 (2002).