Case Report - International Journal of Clinical Rheumatology (2024) Volume 19, Issue 11
Ochronotic arthropathy and its consequences in a middle age man: a case report
Pedro Weingrill1*, Anair Catarina Marconato2†, Vívian Santana Alves2† and André Luiz Gomes3
1Rheumatology Professor, Universidade da Região de Joinville – UNIVILLE. Joinville, Santa Catarina, Brazil
2Universidade da Região de Joinville - UNIVILLE. Joinville, Santa Catarina, Brazil
3Medicine Department - Universidade da Região de Joinville - UNIVILLE. Joinville, Santa Catarina, Brazil
†These authors contributed equally to this work and share senior authorship
- *Corresponding Author:
- Pedro Weingrill
Rheumatology Professor, Universidade da Região de Joinville – UNIVILLE. Joinville, Santa Catarina, Brazil
E-mail: weingrill@terra.com.br
Received: 01-Nov-2024, Manuscript No. fmijcr-24-152735; Editor assigned: 04- Nov-2024, Pre-QC No. fmijcr-24-152735 (PQ); Reviewed: 18-Nov-2024, QC No. fmijcr-24-152735; Revised: 22-Nov- 2024, Manuscript No. fmijcr-24-152735 (R); Published: 29-Nov-2024, DOI: 10.37532/1758-4272.2024.19(11).204-208
Abstract
Alkaptonuria is a rare autosomal recessive disorder characterized by a deficiency of the enzyme homogentisate oxidase, leading to the accumulation of homogentisic acid (HGA) in the body. This accumulation results in symptoms such as darkening of the urine and deposition of pigments in various tissues, including joints, ears, and sclerae, a condition known as ochronosis. In this case report, we present a 47-year-old man who sought care at a Family Health Unit with complaints of arthralgia and dark spots on various parts of his body. The patient was diagnosed with alkaptonuria after a lengthy history of symptoms and medical investigations, culminating in complications such as Achilles tendon rupture and diagnosis of Diffuse Large B-Cell Lymphoma. Despite successful chemotherapy treatment for the lymphoma, the patient continues to face significant challenges related to alkaptonuria, including joint pain and physical limitations.
Keywords
Alkaptonuria • Ochronosis • Arthropathy • Inborn error of metabolism • Non- hodgkin
lymphoma • Case report
Introduction
Alkaptonuria and Ochronosis are manifestations that composes an infrequent clinical scenario caused by the deficiency of the enzyme homogentisic oxidase (1,2-homogentisate dioxygenase), which is essential for the oxidation of homogentisic acid (HGA), a byproduct of the reactions during the catabolism of the amino acids Tyrosine and Phenylalanine. Therefore, it is described as an inborn error of metabolism (IEM), which occurs due to a rare genetic alteration of autosomal recessive inheritance. The absence of this enzyme leads to the serum accumulation of HGA and subsequent renal excretion (homogentisic aciduria). When exposed to air or alkaline substances, the urine undergoes a reaction that darkens it or even turns it black, characterizing Alkaptonuria [1], which is the earliest manifestation of the disease.
Besides the urinary alterations, the HGA present in the blood is polymerized into a darkned/ochre pigment, which is deposited in various tissues of the body, including sclera, skin and cartilage, causing changes in color and biomechanical properties. Furthermore, HGA oxidation reactions and its byproducts in the blood affect collagen bonds, making them more rigid and brittle, causing early degenerative changes and a range of clinical manifestations and joint complications. This phenomenon gives the disease the alternative name of Ochronosis [2].
Case Description
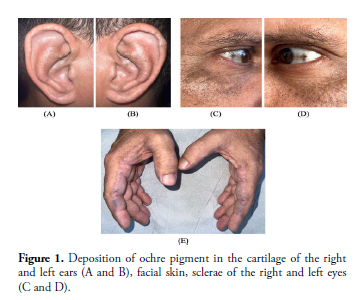
A 47-year-old male patient from Joinville, Santa Catarina, began follow-up at a Primary Health Care Unit in November 2021, complaining of arthralgia in both small and large joints associated with morning stiffness, with progression in intensity over the past year. During the consultation, he reports the presence of bluish/darkened spots on both ears and the lateral aspect of the index fingers and the medial side of the thumbs, hyperchromic spots on the sclera, as well as darkening of the urine about 5 minutes after urinating (Figure 1). He reports that symptoms began early in his life, with urine darkening in cloth diapers sometime after urination; his parents sought medical help but never found answers. The patient states that he noticed the onset of pigment deposits on his hands and ears during adolescence and, and this was followed by joint pain. He underwent previous investigations in adulthood, including urine tests and other laboratory exams, but no significant findings were found that would lead to suspect the disease. The patient is the father of three children and two grandchildren and denied any manifestations in his family members. Suspicion of Alkaptonuria was then raised and further investigation was initiated.
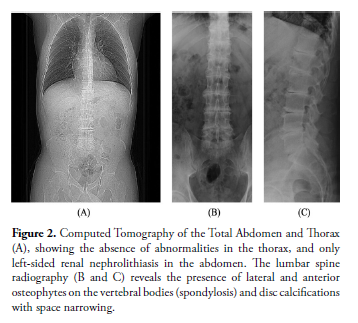
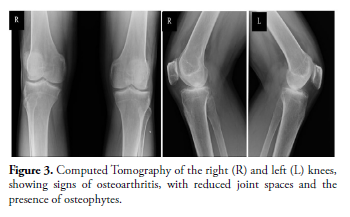
Initially, the patient was referred for follow-up with a nutritionist, who recommended a diet avoiding foods high in potassium and sodium, as well as dark green foods at three-day intervals. Following the cardiologist's advice, an echocardiogram was performed, showing no abnormalities, and an electrocardiogram revealed only a slight delay in conduction through the right bundle. Laboratory tests, including a complete blood count, liver enzymes, lipid profile, and glucose levels, did not show significant changes, although calcium oxalate crystals were observed in the urinalysis. For a comprehensive assessment of the osteoarticular condition, various imaging studies were conducted. The lumbar spine X-ray revealed the presence of lateral and anterior osteophytes on the vertebral bodies (spondylosis) and disc calcifications and space narrowing (Figure 2). The knee X-rays showed signs of osteoarthritis, with reduced joint spaces and the presence of osteophytes (Figure 3). An abdominal ultrasound was also performed, but no abnormalities were found in the exam.
Figure 2: Computed Tomography of the Total Abdomen and Thorax (A), showing the absence of abnormalities in the thorax, and only left-sided renal nephrolithiasis in the abdomen. The lumbar spine radiography (B and C) reveals the presence of lateral and anterior osteophytes on the vertebral bodies (spondylosis) and disc calcifications with space narrowing.
Figure 3: Computed Tomography of the right (R) and left (L) knees, showing signs of osteoarthritis, with reduced joint spaces and the presence of osteophytes.
During the investigation process, the patient suffered a left Achilles tendon rupture while walking after playing soccer. Surgical intervention was performed, and during the procedure, an avulsion of the tendon with significant changes in consistency and appearance, including the presence of dark spots, was identified. Consequently, the decision was made to resect the tendon and transfer the Flexor Hallucis Longus, which had a similar appearance but with fewer lesions. The resected material was sent for histopathological analysis and confirmed the presence of ochronotic pigmentation, corroborating the suspicion of alkaptonuria. After this episode, DNA extracted from a buccal swab was analyzed, with molecular analysis performed using next-generation sequencing to investigate potential pathogenic variants in the HGD gene (homogentisate 1,2-dioxygenase, OMIM* 607474). A pathological heterozygous variant was identified: "chr3:120,641,660 C>T (or alternatively c.808G>A - ENST00000283871), causing the substitution of glycine at codon 270 with arginine (p.Gly270Arg)" and "chr3:120,638,553 G>T (or alternatively c.908C>A - ENST00000283871), causing the substitution of alanine at codon 303 with aspartate (p.Ala303Asp)." Pathogenic variants in homozygous or compound heterozygous states in the HGD gene are responsible for alkaptonuria, a genetically determined condition inherited in an autosomal recessive manner.
Additionally, in April 2023, the patient developed lymphadenopathy in the right cervical chain, which was mobile, painless, and not adhered to deeper structures. Initially, an ultrasound of the area showed the presence of atypical or highly inflammatory adenopathy on the right, measuring 2.3 x 1.4 x 2.1 cm. Subsequently, the patient underwent a biopsy of the lymph node in question and was diagnosed with Diffuse Large B-Cell Lymphoma (Non- Hodgkin Lymphoma). The patient was referred to a hematologist and underwent three sessions of chemotherapy with Doxorubicin 90 mg + Cyclophosphamide 1,300 mg + Vincristine 2 mg and one session of Doxorubicin 90 mg + Cyclophosphamide 1,300 mg + Vincristine 2 mg + Rituximab 700 mg. After completing the treatment, a complete metabolic response was observed, and a watchful waiting approach was chosen. However, recently, new lymphadenopathies emerged. A PET/CT scan for restaging highlighted increased FDG (fluorodeoxyglucose) uptake by the left palatine tonsil and bilateral cervical lymph nodes (larger on the right) and right paratracheal lymph nodes, all newly detected, necessitating a return to chemotherapy.
At present, the patient exhibits black-blue discoloration on the hands, face, sclerae, and auricles (link to images of the patient). In addition to the visible manifestations, the patient experiences pain related to limb movements due to global joint involvement. A recent ultrasound of the right ankle shows involvement of the limb by the disease, evidencing early signs of osteoarthritis in the foot, signs of tendinopathy of the anterior and posterior tibial tendons, enthesopathy of the calcaneus, fibrous scar changes in the anterior talofibular and calcaneofibular ligaments, a small joint effusion, signs of chronic plantar fasciitis, and increased thickness of the skin and subcutaneous tissue in the lateral region of the hindfoot.
Discussion
This case highlights a rare genetic condition with autosomal recessive inheritance, with an estimated prevalence in the population ranging from 1 in 250,000 to 1 million people [1], affecting males more frequently [3]. As experienced by the patient, ochronosis is often diagnosed late, with an average age of 56, since the deposit of HGA in the tissues takes decades up to clinical manifestations [1]. Even more, as it is still a little-known disease, many patients had their diagnosis compromised in the past. Fortunately, no family members of the patient have been affected by the genetic disorder.
Nowadays, there is no specific treatment for enzymatic deficiency, as there are reports of potentially fatal complications associated with the replacement of 1,2-homogentisate dioxygenase. Symptom control is the main focus in managing these patients, through pain management and therapies for mobility and osteoarticular strengthening. Delaying disease progression can be managed through a low-protein diet, reducing serum levels of tyrosine and phenylalanine, and supplementation with ascorbic acid (vitamin C) and glutathione, in an attempt to reduce the oxidative processes generated by the disease [4]. Studies show the promising use of Nitisinone [5], an inhibitor of 4-OH-phenylpyruvate dioxygenase in the tyrosine metabolic pathway, to reduce serum and urinary levels of homogentisic acid (HGA) as an attempt to slow the clinical progression of the disease.
Regarding the Non-Hodgkin Lymphoma (NHL) presented by the patient, there is no well-established relationship between alkaptonuria and NHL in the medical literature [6]. Alkaptonuria results from an inherited metabolic error, whereas NHL is generally associated with various immunological, infectious, and genetic factors. To date, there are no studies or sufficient evidence demonstrating a direct link between these two conditions. The occurrence in the described patient may be coincidental, as both diseases have distinct risk factors and etiologies. However, due to the rarity of alkaptonuria, it may be valuable for the medical community to monitor and document any similar cases to identify if there is any pattern or possible association that has not yet been recognized.
This report highlights the importance of considering rare diagnoses such as Alkaptonuria in patients with atypical clinical manifestations, including darkened urine and skin spots, especially when accompanied by chronic joint symptoms. Early diagnosis is essential for appropriate disease management and minimizing complications. Additionally, the case underscores the need for ongoing monitoring of patients with rare genetic disorders, as additional complications, such as the development of neoplasms, may arise over time. Alkaptonuria continues to present a clinical challenge due to the lack of specific treatments, and the current therapeutic approach focuses on symptom management and attempting to slow disease progression. Documenting cases like this is crucial for expanding knowledge about Alkaptonuria and its possible associations with other health conditions.
Patient perspective
The reported patient unfortunately had a very late diagnosis of Alkaptonuria and did not have the opportunity to receive adequate supportive treatment, resulting in significant disease sequelae. Despite the possibility of general involvement of organs, such as the cardiovascular and gastrointestinal systems, due to pigment deposition and oxidation, these have not yet had a significant impact on the patient’s current clinical condition. The osteoarticular system has suffered the most significant alterations, with extensive involvement of tendons and ligaments, leading to drastic consequences in his life. At present, the patient has severe limitations caused by constant pain and is unable to engage in activities due to the high risk of new tendon ruptures.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Moreira C, Shinjo SK, Pereira IA et al. Livro da Sociedade Brasileira de Reumatologia - 3. ed. Santana de Parnaíba [SP]: Manole (2023).
- Brandão LR, Borjaille BP, Hasegawa TM et al. Alcaptonúria (ocronose): relato de dois casos. Revista Brasileira de Reumatologia, 46(5), 369–372 (2006).
- Lima DA, Bastos RC, Filho JA et al. Artropatia ocronótica e alcaptonúria (ocronose): Relato de caso. Revista Brasileira de Ortopedia (2024).
- Mullan A, Cocker D, Taylor G et al. Fatal oxidative haemolysis and methaemoglobinaemia in a patient with alkaptonuria and acute kidney injury. Clin Kidney J (2015).
- Kisa PT, Eroglu ES, Bahceci H et al. Efficacy of Phenylalanine- and Tyrosine-Restricted Diet in Alkaptonuria Patients on Nitisinone Treatment: Case Series and Review of Literature. Ann Nutr Metab 78, 48–60 (2022).
- Cerhan JR, Slager SL Familial predisposition and genetic risk factors for lymphoma. The American Society of Hematology. 20, 2265-2273 (2015).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref