Case Report - Interventional Cardiology (2020) Volume 12, Issue 6
OCT-guided complication management during sirolimus-eluting bioresorbable magnesium stent implantation with nine months OCT follow-up
Gianluca Caiazzo*, Mario De Michele, Luca Golino, Vincenzo Manganiello, Luciano FattoreICCU, Presidio Ospedaliero San Giuseppe Moscati, Aversa, Italy
- Corresponding Author:
- Dr. Gianluca Caiazzo ICCU, Presidio Ospedaliero San Giuseppe Moscati, Aversa, Italy. E-mail: gianluca.caiazzo@gmail.com
Received date: August 17, 2020 Accepted date: September 09, 2020 Published date: September 16, 2020
Abstract
A 54 years-old lady with NSTEMI underwent OCT-guided PCI. After a sirolimus-eluting bioresorbale magnesium stent (BRS) implantation, a second BRS was lost in the coronary artery. OCT guidance allowed the successful management of such complication and showed a good result with almost complete reabsorption of the implanted BRSs at 9 months follow-up.
Keywords
Optical Coherence Tomography (OCT); Bioresorbable Scaffolds (BRS); Percutaneous Coronary Interventions (PCI)
Case Presentation
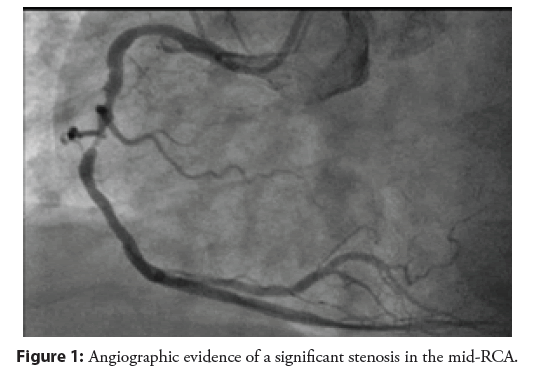
A 54 year-old lady, active smoker with hypertension and hyperlipidemia, presented at our ED with atypical chest pain. EKG was unremarkable while echocardiogram showed mild inferior hypokinesia with normal LVEF (55%). Positive biomarkers for myocardial damage were found. The patient underwent coronary angiography the same day of admission. A significant stenosis of the mid-right coronary artery (RCA) was found (Figure 1).
Figure 1: Angiographic evidence of a significant stenosis in the mid-RCA.
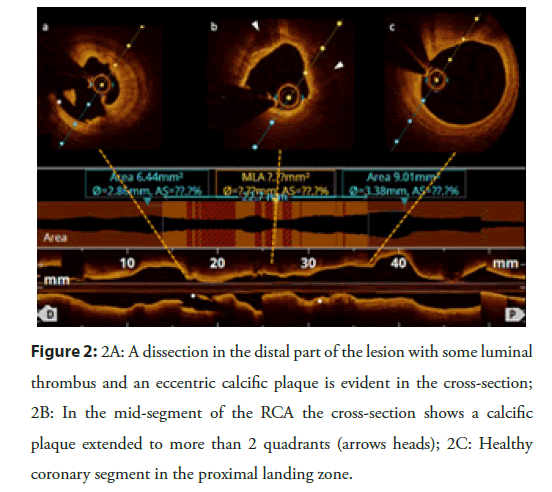
The interventional plan was to implant a sirolimus-eluting bioresorbale magnesium scaffold on the mid-RCA via right radial artery access with OCT guidance. A 6 French Amplatz Left 1 guiding catheter was positioned at the RCA ostium and two workhorse coronary wires were passed through the lesion for higher support. Predilation with a 2.5 × 15 mm semi-compliant balloon at 12 atm was performed. OCT pullback showed a long significant stenosis with a dissection in the distal part of the lesion (mean vessel diameter 2.86 mm), an eccentric calcific plaque in the mid-segment and a normal vessel in the proximal landing zone (mean vessel diameter 3.38 mm) (Figure 2).
Figure 2: 2A: A dissection in the distal part of the lesion with some luminal thrombus and an eccentric calcific plaque is evident in the cross-section; 2B: In the mid-segment of the RCA the cross-section shows a calcific plaque extended to more than 2 quadrants (arrows heads); 2C: Healthy coronary segment in the proximal landing zone.
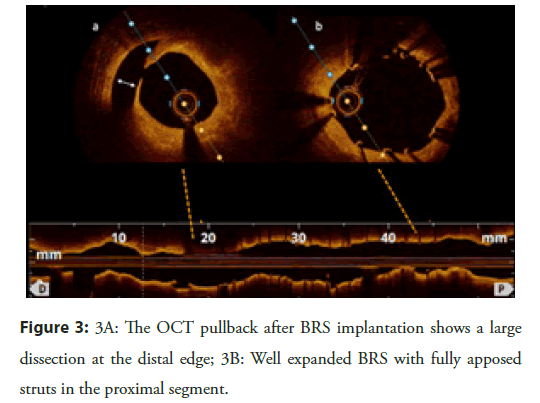
Further 1:1 balloon/artery ratio pre-dilation was performed with a 3.0 × 15 mm non-compliant balloon at 12 atm. After checking for good expansion of the 3.0 mm balloon in two orthogonal views, a 3.0 × 25 mm sirolimus-eluting bioresorbable magnesium scaffold was implanted at 12 atm (stent sizing on the basis of the OCT measures). Post-dilation with a 3.5 × 12 mm non-compliant balloon was performed at 18 atm. At OCT evaluation a significant distal edge dissection was found (Figure 3).
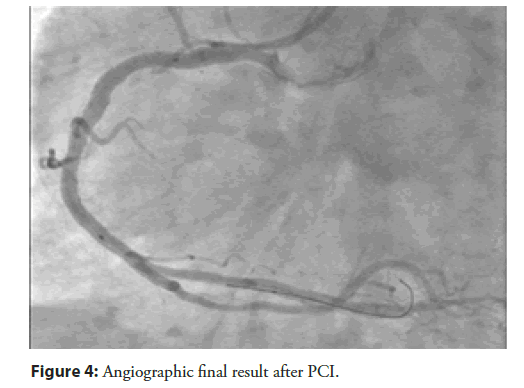
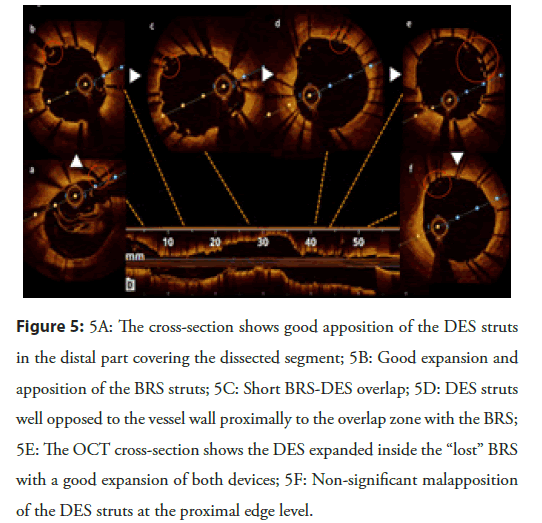
For this reason, the advancement of a second BRS was attempted, in order to cover the distal edge dissection. After two attempts, dislocation of the BRS from its delivery system occurred, with the BRS lying into the proximal segment of the coronary artery, proximally to the previously implanted scaffold. At this point, thin-struts 3.5 × 26 mm drug-eluting stent (DES) was passed through the lost BRS in the proximal RCA and, after checking for sufficient overlapping with the first BRS implanted, the DES was deployed at 14 atm. The distal edge dissection was then covered with a second 3.0 × 18 mm DES deployed at 14 atm. An OCT pullback was performed confirming good stents and scaffold apposition, short overlap between the BRS and the two DES, and presence of the lost BRS fully expanded and embedded into the vessel wall completely covered by the proximal DES struts (Figure 4). A final good result was obtained with a TIMI 3 flow (Figure 5). The patient was discharged after uneventful hospital stay two days later.
Figure 5: 5A: The cross-section shows good apposition of the DES struts in the distal part covering the dissected segment; 5B: Good expansion and apposition of the BRS struts; 5C: Short BRS-DES overlap; 5D: DES struts well opposed to the vessel wall proximally to the overlap zone with the BRS; 5E: The OCT cross-section shows the DES expanded inside the “lost” BRS with a good expansion of both devices; 5F: Non-significant malapposition of the DES struts at the proximal edge level.
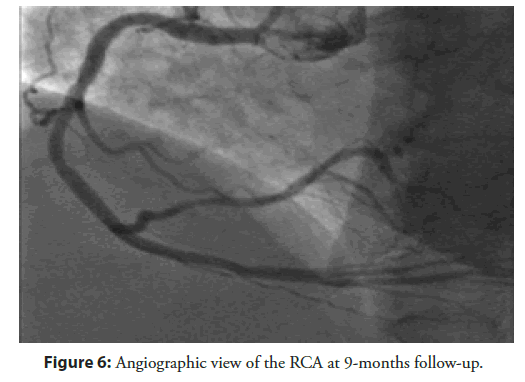
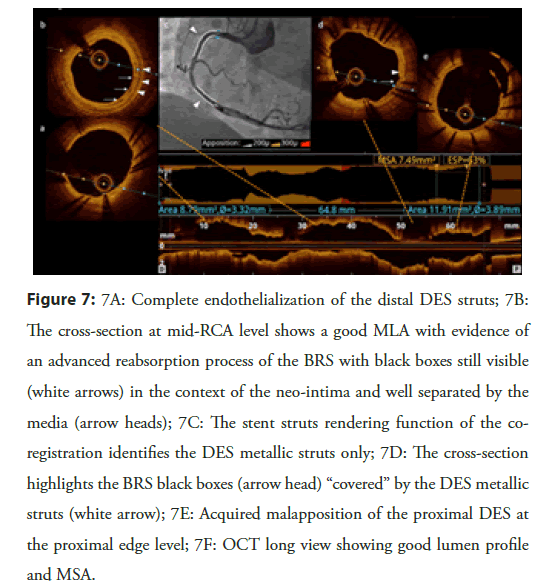
Follow-up
At 9-months angiographic follow-up the artery looked good with TIMI 3 flow and absence of stent/scaffold restenosis. OCT analysis showed: optimal stent apposition in the distal segment with no neo-intimal hyperplasia; advanced reabsorption process of the BRS in the mid-segment with black boxes still visible; good stent apposition in the proximal part with some non-significant acquired malapposition probably due to the dislocated BRS reabsorption between the vessel wall and the DES metallic struts (Figures 6 and 7).
Figure 7: 7A: Complete endothelialization of the distal DES struts; 7B: The cross-section at mid-RCA level shows a good MLA with evidence of an advanced reabsorption process of the BRS with black boxes still visible (white arrows) in the context of the neo-intima and well separated by the media (arrow heads); 7C: The stent struts rendering function of the coregistration identifies the DES metallic struts only; 7D: The cross-section highlights the BRS black boxes (arrow head) “covered” by the DES metallic struts (white arrow); 7E: Acquired malapposition of the proximal DES at the proximal edge level; 7F: OCT long view showing good lumen profile and MSA.
Discussion
The rationale for the use of BRS during PCI are numerous since they provide temporary structural support to a vessel while eluting an anti-proliferative drug, and can be reabsorbed in a timepredictable fashion [1]. The first BRS introduced in the market, the Absorb BVS, have shown, after initial positive results [2], higher scaffold thrombosis rates when compared to last-generation drugeluting stents [3,4]. Notwithstanding limited clinical evidence available to date, magnesium-based BRS represent an interesting novelty in this field, promising higher radial force than PLLAbased BRS [5-7].
Conclusion
Our case shows a very good angiographic and OCT mid-term result after magnesium BRS implantation although a procedural complication occurred. OCT provided precious information for complication management and interpretation.
Acknowledgements
Funding
No financial support has been received for this article.
Disclosures
Authors have no competing interests and no relationships with industry to declare.
References
- Capodanno D. Bioresorbable scaffolds: clinical outcomes and considerations. Interv Cardiol Clin. 5(3): 357-363 (2016).
- Caiazzo G, Kilic ID, Fabris E, et al. Absorb bioresorbable vascular scaffold: What have we learned after 5 years of clinical experience? Int J Cardiol. 15: 129-36 (2015).
- Lipinski MJ, Escarcega RO, Baker NC, et al. Scaffold thrombosis after percutaneous coronary intervention with ABSORB bioresorbable vascular scaffold: a systematic review and meta-analysis. JACC Cardiovasc Interv. 9(1): 12-24 (2016).
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. ESC scientific document group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 40(2): 87-165 (2019).
- Ielasi A, Cerrato E, Geraci S, et al. Sirolimus-eluting magnesium resorbable scaffold implantation in patients with acute myocardial infarction. Cardiology. 142(2): 93-96 (2019).
- Rapetto C, Leoncini M. Magmaris: a new generation metallic sirolimus-eluting fully bioresorbable scaffold: present status and future perspectives. J Thorac Dis. 9(S9): S903-S913 (2017).
- Cerrato E, Barbero U, Gil Romero JA, et al. Magmaris™ resorbable magnesium scaffold: State-of-art review. Future Cardiol. 15(4): 267-279 (2019).