Research Article - Interventional Cardiology (2022)
Optimal procedure for high-quality chest compression during cardiac arrest resuscitation of a patient in Japanese bathtub: Manikin-based randomized trial
- Corresponding Author:
- Koji Fujita
Department of Neurological Surgery,
Naga Municipal Hospital,
Kinokawa City,
Wakayama,
Japan,
E-mail: priuskf@gmail.com
Received date: 28-Mar-2022, Manuscript No. FMIC-22-61120; Editor assigned: 30-Mar-2022, PreQC No. FMIC-22-61120 (PQ); Reviewed date: 15-Apr-2022, QC No. FMIC-22-61120; Revised date: 22-Apr-2022, Manuscript No. FMIC-22-61120 (R); Published date: 29-Apr-2022, DOI: 10.37532/1755- 5310.2022.14(S9).214
Abstract
Background: In Japan, the outcome from treatment of bath-related cardiac arrest patients has been poor, because of difficulties with performing Cardiopulmonary Resuscitation (CPR) of sitting patients in small bathtubs. To clarify the most appropriate CPR in bathtubs, our study was conducted in order to compare the differences in chest compression quality when CPR is performed on sitting and supine patients in a bathtub.Methods: A total of 52 fire academy students were randomly assigned as ‘rescuers’ to perform chest compression on either a sitting manikin (“Sitting Group”) or a supine manikin (“Supine Group”) in a bathtub. The quality of chest compression performed for 2 minutes by the two different groups was investigated.
Results: The rate of chest compressions with the correct hand position was better in the Supine Group (96.1%) than in the Sitting Group (94.6%; p<0.01). The rate of total chest compressions with correct recoil was greater in the Sitting Group than in the Supine Group (60.5% versus 13.5%, p<0.001). In the Supine Group, the average depth of chest compression (48.4 mm) was better than in the Sitting Group (40.8 mm; p<0.001). Although in both groups, the depth of chest compressions gradually attenuated significantly with time, the optimal compression depth for survival was nearly maintained. In the Supine Group, the number of participants with appropriate chest compression depth was kept during 2-minute CPR.
Conclusion: The rescuer’s chest compression quality during CPR in the bathtub was better with supine patients than with sitting patients due to the difference in accumulated fatigue of the rescuer.
Keywords
Chest compression • Bath-related cardiac arrest • Cardiopulmonary resuscitation • Manikin-based randomized trial
Abbreviations
CPR: Cardiopulmonary Resuscitation; BLS: Basic Life Support; AHA: American Heart Association; i-EMG: Integrated Electromyography
Background
Taking a long bath by soaking in a bathtub filled with hot water has been a traditional custom for the Japanese, unlike their European and American counterparts [1]. Its purposes are not only to warm the bather’s body, but also to aid relaxation. However, sudden death in bathtubs has been receiving increasing attention in Japan [2,3]. According to the recent nationwide survey in Japan, bath-related deaths have been reported as accounting for more than 10% of all sudden deaths [2]. The annual number of sudden deaths during bathing was estimated to be approximately 19,000, with most victims aged 65 or older [3]. The outcome of bath-related cardiac arrest patients was extremely poor, as shown by a report that the rates of prehospital return of spontaneous circulation and of one-month survival were 3.6% and 1.6%, respectively [4].
Another feature of Japanese bathing customs is that the typical Japanese bathtub is deep and small, typically 500 to 600 mm in depth and 800 to 1100 mm in width. Bathers sit hugging their knees during bathing, with hot water immersion up to the shoulders. For this reason, a bystander often has to perform chest compression of a cardiac arrest patient stranded in a small tub, owing to the difficulty of rescuing the patient outside it. However, the optimal setting and procedure for Cardiopulmonary Resuscitation (CPR) using chest compression only, performed on patients with bath-related cardiac arrest in the tub, has not been sufficiently investigated.
The present study was conducted to clarify differences in the quality of chest compression in the bathtub, by comparing the relative performance with sitting and supine positioning of adult patients using simulation manikins.
Materials and Methods
Study design
The 52 volunteer participants (mean age 20.7 years, average height 172.4 cm, and predominantly male (49)) were recruited from the students of the Fire Fighter Academy in Wakayama Prefecture. They underwent a Basic Life Support (BLS) training program. The participants were randomly assigned (based on a 1:1 ratio) to one of two CPR groups, the first using a human-like, mechanical manikin in a sitting position (“Sitting Group”) and the second using a similar manikin in a supine position (“Supine Group”) and applying the envelope method. The flow chart is shown in Figure 1.
Study settings
We prepared two bathtubs of an approximate standard size (measuring 1200 mm by 720 mm with 500 mm in depth) for Japanese-style bathing and two Resusci Anne Simulator PLUS manikins (length of 1600 mm and weight of 21 kg) (Laerdal Medical, Norway). Then we placed two manikins in either a sitting or a supine position into each tub.
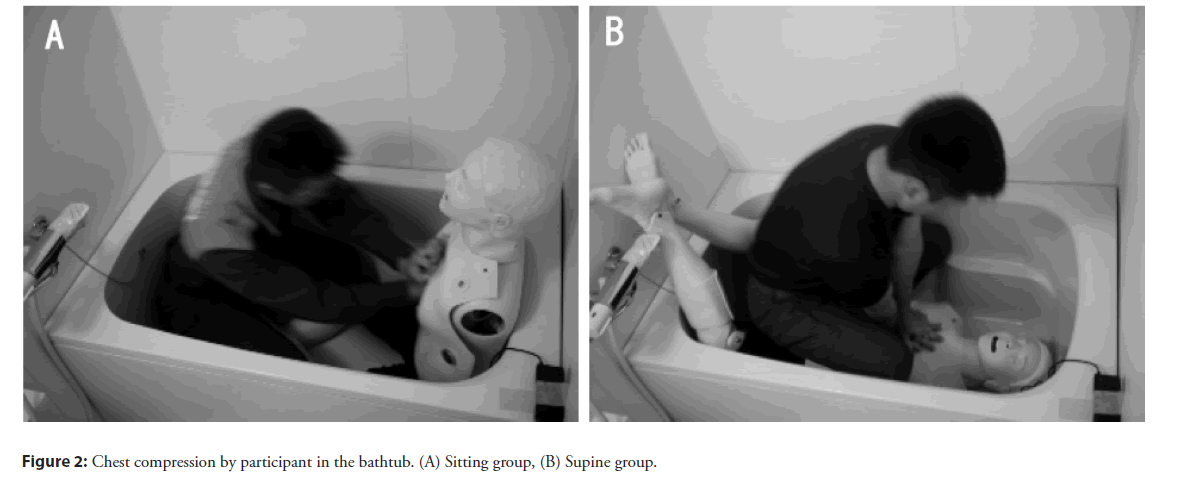
Each participant entered our laboratory alone. On site, they were allocated randomly into either the Sitting or the Supine Group. Then the participant got into the bathtub and performed 2-minute chest compression-only CPR of the manikin with the designated posture in the tub (Figure 2). While chest compressions were being performed, the total number of chest compressions, the tempo of chest compressions, the number of correct hand positions during chest compressions, the depth at recoil during chest compressions and the depth of chest compressions were continuously recorded using a SimPad PLUS System (Laerdal Medical, Norway). On the assumption that the rescuer would receive verbal guidance from a dispatcher, a metronome was used as a pace-making device during chest compression, providing tones of 110 compressions per minute.
According to the American Heart Association (AHA) 2015 guideline, chest compression-only CPR without rescue breath is recommended as the preferred CPR technique performed by an untrained bystander [5]. Consequently, we adopted chest compression-only CPR in this trial. In addition, based on previous reports of a decrease in quality of chest compression by a single rescuer over 120 seconds after starting CPR [6,7], we set the duration of chest compression at 2 minutes. The appropriate tempo of chest compressions per minute was established between 100 and 120 per minute, as recommended by the AHA 2015 guideline [5]. The adequate compression depth was defined in the 2015 AHA recommendation as 50 mm or more but less than 60 mm [5]. The sufficient recoil was defined as full lift up from the chest.
We evaluated the total input data for 2-minute chest compression performed by each participant, and the data was divided into quarters, i.e. the first period (time from the beginning of chest compression to 30 seconds), the second period (from 31 to 60 seconds), the third period (from 61 to 90 seconds), and the fourth period (from 91 to 120 seconds).
Statistical analysis
The JMP pro version 14 (SAS Institute Inc., Cary, NC, USA) was employed for all the statistical analyses. The data were compared across groups using the chi-squared test for categorical variables and the student’s t-test for continuous variables. Analysis Of Variance (ANOVA) was applied to compare mean compression depths for each group during the four periods, thus checking any time-dependent changes. The difference in the sufficient chest compression depth (50 mm or more but less than 60 mm) ratio between the first and fourth periods in each group was analyzed with a chi-squared test. All of the tests were two-tailed and a p-value of <0.05 was considered statistically significant.
Results
Participants demographics
Fifty-two participants were enrolled in this study and divided into two groups of 26 members of a “Sitting Group” and a “Supine Group”, respectively. The baseline characteristics of the participants are shown in Table 1. There were no significant differences between the two groups in terms of age, sex ratio, height or previous CPR training.
Performance of chest compressions during two-minute test period
Table 1 shows the participants’ performance of chest compressions in 2-minute CPR for each group. There was no significant difference in the number of chest compressions performed by the two groups (211.9 ± 35.4 for the Sitting Group compared to 218.3 ± 4.2 for the Supine Group, p=0.183). With regard to the tempo of chest compressions per minute, the difference was not significant between the groups (109.25 ± 2.90 for the Sitting Group compared to 109.18 ± 2.89 for the Supine Group, p=0.233). As regards the appropriate tempo rate for chest compressions, from 100 to 120 per minute, there was also no significant difference between the Sitting Group (99.3%) compared to the Supine Group (99.4%, p=0.405). The proportion of chest compressions performed with the correct hand position was significantly better in the Supine Group (96.1%) than in the Sitting Group (94.6%; p<0.01). The average depth at recoil during chest compressions was significantly deeper in the Supine Group than in the Sitting Group (4.85 ± 3.77 mm versus 1.65 ± 2.89 mm, p<0.001). The rate of total chest compressions with correct recoil during the 2-minute CPR in the Sitting Group was 60.5%, which was significantly higher (p<0.001) than that in the Supine Group (13.5%).
| Sitting group (n=26) | Supine group (n=26) | p-value (chi-squared or t-test) | |
|---|---|---|---|
| Age, year, mean ± SD | 20.50 ±2 .06 | 20.96 ± 1.93 | 0.409 |
| Male, n (%) | 24 (92.3) | 25 (96.2) | 1 |
| Height, cm, mean ± SD | 171.3 ± 6.2 | 173.0 ± 7.7 | 0.398 |
| Prior CPR training, n (%) | 26 (100) | 26 (100) | - |
| Total number of CCs, n | 5510 | 5676 | - |
| Number of CCs , n, mean ± SD | 211.9 ± 35.4 | 218.3 ± 4.2 | 0.183 |
| Tempo of CCs per minute, n, mean ± SD | 109.25 ± 2.90 | 109.18 ± 2.89 | 0.233 |
| Proportion of CCs with appropriate tempo from 100 to 120 per minute, n/total (%) | 5470/5510 (99.3) | 5642/5676 (99.4) | 0.405 |
| Proportion of CCs with correct hand position, n/total (%) | 5212/5510 (94.6) | 5453/5676 (96.1) | <0.01 |
| Mean depth of release of CCs, mm, mean ± SD | 1.65 ± 2.89 | 4.85 ± 3.77 | <0.001 |
| Proportion of CCs with correct recoil, n/total (%) | 3331/5510 (60.5) | 766/5676 (13.5) | <0.001 |
| Mean depth of CCs, mm, mean ± SD | 40.8 ± 8.9 | 48.4 ± 10.2 | <0.001 |
| Proportion of appropriate depth of CCs from 50 to 59mm, n/total (%) | 860/5510 (15.6) | 1689/5676 (29.8) | <0.001 |
Abbreviations: CPR: Cardiopulmonary Resuscitation; CCs: Chest Compressions
Table 1: Baseline and clinical characteristics of participants.
Depth of chest compression related to the time course
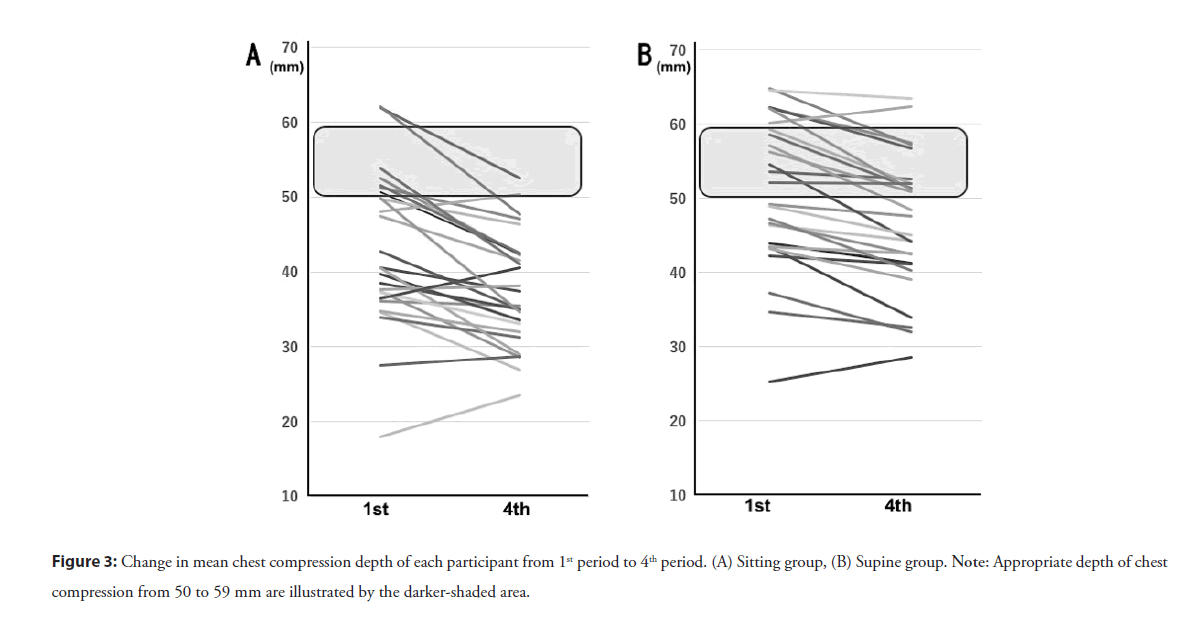
The mean depth of chest compressions over the whole 2 minutes was significantly deeper in the Supine Group than in the Sitting Group (48.4 ± 10.2 mm versus 40.8 ± 8.9 mm, p<0.001) (Table 1). The mean chest compression depth was calculated for each 30-second period during the 2 minutes of uninterrupted chest compressions. Table 2 shows the average depth and the rate of sufficient depth of chest compressions during each of those periods of that 2-minute CPR. In the Sitting Group, the mean depth of chest compressions reported in the four periods decreased steadily and significantly (the readings for the first, second, third and fourth periods are 43.7 ± 9.5 mm, 42.2 ± 9.0 mm, 39.6 ± 8.0 mm, 37.8 ± 8.0 mm, respectively, p<0.001). When the compression depths of each period in any given resuscitation were analyzed, the sufficient chest compression depth ratio (50 mm or more and less than 60 mm) in the fourth period (9.0%) had significantly declined compared with the first period (21.3%, p<0.001). In the Supine Group, the average depth of chest compressions in all four periods, also attenuated significantly (the first, second, third and fourth periods had readings of 50.7 ± 10.5 mm, 49.3 ± 10.5 mm, 47.1 ± 10.1 mm, 46.6 ± 9.3 mm, respectively, p<0.001 ). In contrast, a significant increase in the sufficient chest compression depth ratio was observed in the fourth period (30.5%) as compared to the first period (26.1%, p<0.001). The changes of the mean chest compression depth of each participant from the first to the fourth periods are demonstrated in Figure 3. The number of participants who carried out chest compression with appropriate depth between 50 and 59 mm decreased from five in the first period to two in the fourth period in the Sitting Group. In contrast, in the Supine Group the number increased from seven to nine.
| Sitting group (n=26) | Supine group (n=26) | |||
|---|---|---|---|---|
| p-value | p-value | |||
| Total number of CCs, n | 5510 | 5676 | ||
| Mean depth of CCs, mm, mean ± SD | <0.001* | <0.001* | ||
| 1st period | 43.7 ± 9.5 | 50.7 ± 10.5 | ||
| 2nd period | 42.2 ± 9.0 | 49.3 ± 10.5 | ||
| 3rd period | 39.6 ± 8.0 | 47.1 ± 10.1 | ||
| 4th period | 37.8 ± 8.0 | 46.6 ± 9.3 | ||
| Proportion of appropriate depth of CCs from 50 to 59mm, n/total (%) | <0.001**  | <0.001**  | ||
| 1st period | 292/1372 (21.3) | 365/1398 (26.1) | ||
| 2nd period | 261/1374 (19.0) | 436/1426 (30.6) | ||
| 3rd period | 181/1369 (13.2) | 453/1426 (31.8) | ||
| 4th period | 126/1395 (9.03) | 435/1426 (30.5) | ||
Note: CCs: Chest Compressions; *Analysis Of Variance (ANOVA); **Analysis was performed based on the 4th period compared to 1st period by chi-squared test.
Table 2: Differences of depth of CCs over consecutive 30-second segments.
Discussion
To our knowledge, this manikin-based randomized trial is the first to evaluate the quality of chest compression during CPR of the patients with cardiac arrest in the bathtub. Japanese people typically sit hugging their knees in a small tub filled with hot water as part of their daily customs. Owing to this, it is very possible that patients with cardiac arrests during bathing are found in a sitting posture in the tub. According to a report by Kiyohara, et al. in a sample of 512 bath-related cardiac arrests in Japanese homes, the place of arrest was inside a bathtub in 86.9% of the cases, in a wash place in 12.1% of the cases and in a dressing room in 1% of the cases [4]. As it is difficult for a bystander to rescue a patient from outside a small bathtub, we arranged for participants in this trial to perform chest compression inside the actual tub. High quality chest compression during CPR is characterized and impacted by optimal tempo, location, recoil and depth. This study was able to investigate all of these factors under unstable situations, such as patients sitting or in a supine posture in a bathtub.
The appropriate tempo of chest compression was nearly maintained without degradation by both of the two groups. Using a pace-making device such as a metronome is reported to help sustain the ideal tempo of chest compression [8,9]. In our study, it was considered that employing a metronome might contribute to maintaining an adequate tempo of chest compression during CPR.
High quality chest compression must apply vertical pressure to the patient’s sternum from directly above it. The heel of one hand of the rescuer should be placed on the patient’s sternum, while the heel of the other hand is placed on top of the first hand. To shift the weight of the rescuer’s upper body onto the hands, the shoulders should be positioned directly above the hands with the elbows kept straight. As regards the hand position for chest compression, participants in the Supine Group were able to exert more effective pressure on the sternum, and from the right position, than the Sitting Group. In contrast, the state of recoil with chest compression was worse in the Supine Group than in the Sitting Group. As reasons for this, we surmise that in the Supine Group, despite pushing on the sternum using the optimal hand position, due to the participant’s head being in a forward posture in a narrow tub during the chest compressions, the weight of the participant’s upper body applied sustained loading to the location of compression.
We found the average depth of chest compression in the Sitting Group was far from sufficient. In the Sitting Group, as the participant was directly facing the manikin, the participant was forced to perform an insufficient chest compression with flexion and extension of the elbow joints, making it difficult to transfer the weight of the upper body to the hands. However, in both groups, the average depth of chest compressions corresponded to the optimal compression depth in the range of 40.3-55.3 mm, which is strongly associated with maximum survival in a large study of out-of-hospital cardiac arrest resuscitation for adults [10]. In even the Sitting Group, the average depths of chest compression in the first and second periods was over 40 mm. Based on these results, the chest compression under these conditions was predictably effective.
The average change in compression depth in both groups from the first 30 second period to the later three periods gradually decreased with time. This finding was consistent with the results of previous studies, which suggested that rescuer fatigue plays an important role in a time-dependent deterioration in chest compression quality [6,7,11-13]. In the Sitting Group, the fall in chest compression depth was considered to reflect a more excessive accumulation of participant fatigue than the corresponding accumulation of fatigue in the Supine Group. Yasuda, et al. reported that when chest compression was performed under ambulance transportation conditions and associated muscle activity was investigated using integrated Electromyography (i-EMG), it became clear that the total i-EMG values were significantly higher for the deltoid, pectoralis major, and triceps brachii muscles than when chest compression was performed under static conditions [14]. In the Sitting Group, chest compression might be predominantly dependent on the triceps brachii muscles, in order to keep the elbows straight in a disadvantageous position. We thought this disproportionate muscle activity made the participant’s fatigue negatively affect the quality of chest compression. In contrast, in the Supine Group, the number of participants performing chest compression with appropriate depth was maintained from the first to the fourth periods. We speculated that although the participants in the Supine Group performed low-quality chest compression at the start of chest compression in an unfamiliar situation in a narrow bathtub, some of them were able to gradually adjust to this, due to their relatively stable posture and the lower stress on their muscles compared to the situation facing participants in the Sitting Group.
In Japan, the average time taken from an emergency call to arrival at the emergency scene is 8.7 minutes [15]. The bystander is strongly urged by the dispatcher to perform uninterrupted chest compression until emergency technicians arrive at the site. When the bystander performs the chest compression of cardiac arrest patients in a bathtub, it is preferable to initiate the chest compression immediately in the supine position on a hard floor after rescuing the patient from the bathtub. However, it is a quite challenge to pull the unconscious patient out of the tub in cases where the single rescuer is relatively weak or differs from the patients in physical build. Also, insisting on getting the patient out of the tub may cause injury to the rescuer and delay the start of chest compression. If the rescuer starts water discharge from the bathtub immediately after finding the patient and places the patient supine in the tub as fast as possible, chest compressiononly CPR in the tub has a real chance of being equally effective as when it is performed on the floor. Considering that it generally takes about 6 minutes to drain all the water from a Japanese-style, regular-sized bathtub, the rescuer can start the chest compression of the patient before an ambulance arrives at the scene. It will be an even more effective CPR if the rescuer starts the chest compression of the patient in a sitting position first, during water discharge from the bath, and then, when the drainage is nearly complete, goes on to place the patient supine on the bottom of the bathtub and performs uninterrupted chest compression. To place the patient supine from a sitting posture in the bath is easier than to get the patient out of it. Nevertheless, if it is impossible for the rescuer to change the patient’s body position from sitting to supine, the chest compression of the patient in the sitting position is acceptable. This is because from our study’s findings we can see that the optimal compression depth during CPR was maintained even in sitting patients, especially during the first minute.
There are several limitations in this study. Firstly, our results were obtained from a simulation study using a manikin. When we placed the upper body of the manikin in a supine posture in the small tub, we had to thrust both legs upward, due to its hip and knee joints being immobile. Thus, since the actual human body differs from that of a manikin in the weight and range of joint movements, the situation of CPR of a human body may not be the same as this manikin trial. Moreover, appropriate resuscitation skills on a manikin might not necessarily lead to better clinical outcomes. The differences in the hardness of the chest of the manikin compared to that of a human must be considered, because this could affect rescuer fatigue. Also, we were not able to carry out this trial in a bathtub filled with hot water. In real situations, the bystander may behave differently from in these trial conditions.
Secondly, chest compression was performed by young paramedic students with an average age of around 20. All of them had sufficient training in CPR with official AHA BLS certification. Thus, we should be careful in extrapolating our trial results to ordinary people or any other generation.
Thirdly, the Japanese style bathtub that we used is smaller than the European or American style. As a result, our data might not be applicable in Western countries. However, these results, which demonstrate a significant decline in chest compression quality due to rescuer fatigue in unusual situations, may provide useful hints for performing CPR. Accordingly, our research findings can be applied to chest compression for CPR in various difficult situations, such as where the patient is trapped inside a car or in rubble.
Conclusion
In this manikin-based randomized trial, we found that the chest compression during CPR for patients with cardiac arrest in a bathtub was of better quality in the supine position than in the sitting position. The low quality of chest compression of sitting patients was attributed to greater accumulated fatigue of the rescuer compared with rescuers of supine patients. However, in both positions, the optimal compression depth for survival was nearly maintained. Based on the results, a feasible CPR will be for the rescuer initially to start the chest compression of the sitting patient while water is discharged from the bath, and then when the drainage is nearly complete for the rescuer to place the patient in a supine position on the bottom of the tub and perform the rest of the chest compression.
Acknowledgments
The authors gratefully acknowledge the contribution of the students of Fire academy in Wakayama Prefecture. We also would like to thank William Spurgeon for the English language editing of the manuscript.
Authors’ Contributions
TI, YW and KF conducted the study design. TI, YW, SK and HN conducted the trainings and simulations. YS and KF performed the statistical analysis. TI, YS, SK and KF contributed to the data analysis and interpretation. TI and KF drafted the manuscript and revised it together with YW and HN. All authors have approved the final version of the manuscript.
Funding
There was no funding source in the design or conduct of the study.
Availability of Data and Materials
The datasets used in the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Wakayama Fire Fighter Academy and Wakayama Fire Fighting Command and Control Center. Participants submitted their written informed consent prior to participation. The authors certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Competing Interests
There are no competing interests to declare in this study.
References
- Traphagan JW. Culture and long-term care: The bath as social service in Japan. Care Manag J. 5(1): 53-60 (2004).
[CrossRef] [Google Scholar] [PubMed]
- Kouno A, Matoba R, Shikata I. A statistical study of sudden cardiac death for past five years in Osaka medical, investigated at the Osaka Medical Examiner’s Office. Acta Med Leg Soc (Liege). 39(1): 205-15 (1989).
[Google Scholar] [PubMed]
- Suzuki M, Shimbo T, Ikaga T, et al. Sudden death phenomenon while bathing in Japan-mortality data. Circ J. 81: 1144-9 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Kiyohara K, Nishiyama C, Hayashida S, et al. Characteristics and outcomes of bath-related out-of-hospital cardiac arrest in Japan. Circ J. 80(7): 1564-70 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 132(18 S2): S414-35 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Sugerman NT, Edelson DP, Leary M, et al. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: A prospective multicenter study. Resuscitation. 80(9): 981-4 (2009).
[CrossRef] [Google Scholar] [PubMed]
- Yamanaka S, Huh JY, Nishiyama K, et al. The optimal number of personnel for good quality of chest compressions: A prospective randomized parallel manikin trial. PLoS ONE. 12(12): e0189412 (2017).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Bae J, Chung TN, Je SM. Effect of the rate of chest compression familiarised in previous training on the depth of chest compression during metronome-guided cardiopulmonary resuscitation: A randomised crossover trial. BMJ Open. 6(2): e010873 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Shimizu Y, Tanigawa K, Ishikawa M, et al. An appropriate compression pace is important for securing the quality of hands-only CPR. A manikin study. Hiroshima J Med Sci. 63(1-3): 7-11 (2014).
[Google Scholar] [PubMed]
- Stiell IG, Brown SP, Nichol G, et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 130(22): 1962-70 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Ochoa FJ, Ramalle-Gomara E, Lisa V, et al. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 37(3): 149-52 (1998).
[CrossRef] [Google Scholar] [PubMed]
- Ashton A, McCluskey A, Gwinnutt CL, et al. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation. 55(2): 151-5 (2002).
[CrossRef] [Google Scholar] [PubMed]
- McDonald CH, Heggie J, Jones CM, et al. Rescuer fatigue under the 2010 ERC guidelines, and its effect on Cardiopulmonary Resuscitation (CPR) performance. Emerg Med J. 30(8): 623-7 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Yasuda Y, Kato Y, Sugimoto K, et al. Muscles used for chest compression under static and transportation conditions. Prehosp Emerg Care. 17(2): 162-9 (2013).
[CrossRef] [Google Scholar] [PubMed]
- 2019 report on the current state of emergency services by National Fire and Disaster Management Agency of Japan. (2021).