Research Article - Clinical Practice (2017) Volume 14, Issue 2
Outpatient surgery of skin and soft tissue lesions: case summary and perspectives on training
- Corresponding Author:
- Qi Bao
Department of Plastic and Reconstructive Surgery
2nd Affiliated Hospital, Zhejiang University School of Medicine
Hangzhou, China
E-mail: baoqi@zju.edu.cn
Abstract
Background & Objectives: Summarize experience in skin and soft tissue lesion surgery in an outpatient operation room (OR) of a large University department, as a means to demonstrate the surgeries in the training of plastic surgeons. Methods: 242 skin and soft tissue lesions were retrospectively analyzed according to pathological classifications and treatments. Results: From Oct. 2014 to Aug. 2015, 212 patients with 242 lesions were operated on in our outpatient OR. 76 cases were male and 136 female, with a mean age of 33.5. The youngest patient was 7-years old, while the oldest was 74. The most frequent pathological types were intradermal nevus (33.5%), compound nevus (15.3%), epidermoid cyst (11.2%), seborrheic keratosis (8.3%), and hemangioma (4.5%). The top five operation sites were at face (42.1%), trunk (11.6%), neck (8.7%), scalp (8.3%) and nose (6.6%). The coincidence rate of pre-operation diagnosis and post-operation pathological diagnosis was 93.0%. The complication rate was 1.2%. Conclusions: The plastic surgery department of public general hospital has a large number of patients with skin and soft tissue lesions that belong to a variety of pathological types. This provides a good platform to train plastic surgeons.
Keywords
outpatient surgery, skin and soft tissue lesions, plastic surgery training
Introduction
Patients come to the Plastic Surgery Departments of public hospitals in China for treatment of skin or soft tissue lesions. In addition to wards and operation-room surgeries, the outpatient clinic for minor surgery represents an important resource for the training of plastic surgeons (first 2-3 years in fellowship). In the present study, we summarize the cases of skin and soft tissue lesion surgeries in the outpatient operation room (OR) of our department and outline the significance of these minor surgeries in the training of plastic surgeons.
Clinical Methods
Common data
212 patients with skin or soft tissue lesions were admitted to our clinic from Oct. 2014 to Aug. 2015. Totally, 242 masses were resected. Among the recruited patients, 76 cases were male (35.9%), and 136 cases were female (64.1%). 21 patients had 2 masses resected at once, and 4 patients had 3 masses resected at once. The mean age of all the patients was 33.5, with an age ranging from 7 to 74. The mean ages for male and female patients were 35.2 and 32.8 respectively.
Pre-operation preparation
Blood samples were drawn from all patients before operation for analysis of complete blood cell count (CBC), coagulation function (PT, INR, PTT), HIV, HBV, HCV and Syphilis antigen test. Operations were scheduled for the patients whose tests were in normal range. In order to prevent hypoglycemia syncope, we advised patients to take meals as usual before surgery. For hypertensive (HTN) patients, the schedule for taking anti-hypertensive medicine was not changed. Vital signs including temperature, blood pressure, heart rate and breath rate were checked right before the surgery. The operation was performed only when vital signs were in a normal range. All patients were informed with surgery risks and complications.
Pathological diagnosis
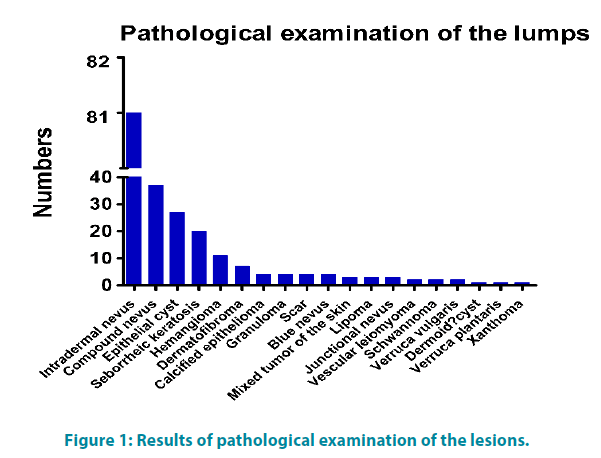
All resected masses were sent for pathological analysis. The most frequent pathological types were intradermal nevus (81 cases), compound nevus (37 cases), epidermoid cyst (27 cases), seborrheic keratosis (20 cases), and hemangioma (11 cases). Other pathological types included 7 cases of dermatofibroma, 4 cases of calcified epithelioma, granuloma, scar and blue nevus, mixed tumor of the skin, lipoma and junctional nevus each with 3 cases, vascular leiomyoma, schwannoma and verruca vulgaris each for 2 cases, dermoid cyst, verruca plantaris, basal cell carcinoma, pilar cyst, amyloidosis, neurofibroma and xanthoma 1 case each (FIGURE 1). Immunohistochemical staining for markers for neurofibroma, amyloidosis and schwannoma were applied to these 3 cases for precise diagnosis.
The coincidence rate of pre-operation diagnosis and post-operation pathological diagnosis was 93.0%. The final diagnosis was changed in only 17 cases. Among these 17 inconsistent cases, 12 cases of seborrheic keratosis and 1 case of basal cell carcinoma were misdiagnosed as pigmented nevus. 1 case of mixed tumor of the skin was misdiagnosed as sebaceous cyst, 1 case of pilar cyst was misdiagnosed as lipoma, 1 case of hemangioma was misdiagnosed as granuloma and 1 case of seborrheic keratosis was misdiagnosed as sebaceous nevus (TABLE 1). 11 out of 14 cases tested with ultrasound examination were confirmed in the final diagonosis (78.6%). The 3 cases that were misdiagnosed by ultrasound were the same -- dermatofibroma. The pre-operation ultrasound suggested they were sebaceous cyst, folliculitis and lipoma respectively.
| Case No. | post-operation pathologic diagnosis | pre-operation diagnosis |
|---|---|---|
| 12 | seborrheic keratosis | pigmented nevus |
| 1 | basal cell carcinoma | |
| 1 | seborrheic keratosis | sebaceous nevus |
| 1 | mixed tumor of the skin | sebaceous cyst |
| 1 | pilar cyst | lipoma |
| 1 | hemangioma | granuloma |
Table 1: Pre-operation diagnosis and post-operation pathologic diagnosis
Locations of the lesions
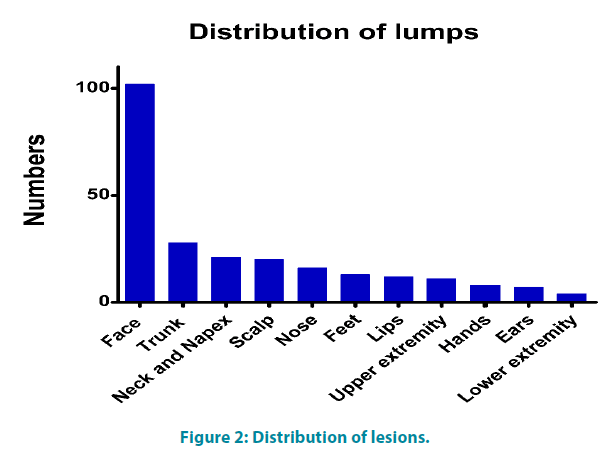
The most frequent operation site was the face (including forehead, brow, periocular, cheek and mandible), accounting for 42.1% (102 cases). 28 cases were on the trunk (11.6%, including chest, abdomen, waist, back, buttock, axillary, shoulders, nipple and areola), 21 cases on neck and napex (8.7%), 20 cases on scalp (8.3%), 16 cases on nose (6.6%), 13 cases on feet (5.4%), 12 cases on lips (5.0%), 11 cases on upper extremities (4.5%), 8 cases on hands (3.3%), 7 cases on ear (2.9%) and 4 cases on lower extremities (1.7%) (FIGURE 2).
Operation procedure
Lidocaine (1%) and epinephrine (1:200 000) were applied as anesthesia. If the patient had hypertension history, we choose 1% of lidocaine without epinephrine to avoid hemorrhage. All incisions were closed as primary closure. The incisions on nose, lips, ears, other facial places and neck were closed by 5-O Prolene®, while the periocular place can choose 7-O Prolene® for cosmetic purposes. For the extremities, scalp and trunks incision, 2-O or 4-O thread was choosen to suture for tension purposes. No antibiotics were applied for sterile incision, and local wound care was done once a day. If the postlesion- resection wound was deep, normally 1-2 latex flaps were left for drainage. This flap was removed on post-operation day 1. If the wound recovered well, and there was no erythema or edema, the suture was removed after 7 days on lip, face and neck surgeries. After 10 days, the suture on nose, trunk, napex and ears was removed. For scalp and extremities’ incisions, were removed after 14 days.
Results
In these 242 cases of lesion resection, 239 cases which accounted for 98.8% were primary wound healing, while 3 cases developed as complications. These 3 complications were all incision dehiscence. One of them was pathologically diagnosed as basal cell carcinoma, and the basal cutting edge was positive. This patient was then hospitalized and received extended resection of the lesion and nasolabial fold island flap reconstruction. The other 2 cases were cured by long-time wound care with secondary intention.
Discussion
Pathological diagnoses
Based on pathological analysis, the most common pathological type treated was intradermal nevus, which accounted for 81 cases. And the 2nd to 5th top pathological types were compound nevus, epithelial cyst, seborrheic keratosis and hemangioma respectively. The common types of skin and soft tissue lesions can be treated by plastic surgeons in training. Almost all pathological types of skin and soft tissue lesions were observed in this process. Pursuing the pathological result represents good training for surgeons, as provides experience to differentiate benign and malignant lesions. Cutaneous or subcutaneous masses that are firm, fixed, painful, or adherent to adjacent structures are more concerning for malignancy [1].
If we summarized all the nevi, including intradermal nevi, compound nevi, junctional nevi and blue nevi, they accounted for more than half of cases. So nevi are the most common lesions in our outpatient plastic surgery clinic. The number of female patients was twice that seen as male (136 vs. 76).
Incision lines
The Langer’s line was normally followed during incision design. The Langer’s line is the natural direction/alignment of connective tissue in the dermis (e.g. transverse lines across the abdomen). Incisions perpendicular to Langer’s lines result in larger scars than incisions parallel to the lines. So the incision lines were made parallel to the Langer’s line, as well as the wrinkle line and the counter line to minimize scars. The lesions treated were distributed over all of parts of the body providing a good opportunity for young plastic surgeons to become familiar with the anatomy of the skin and soft tissues.
Complications
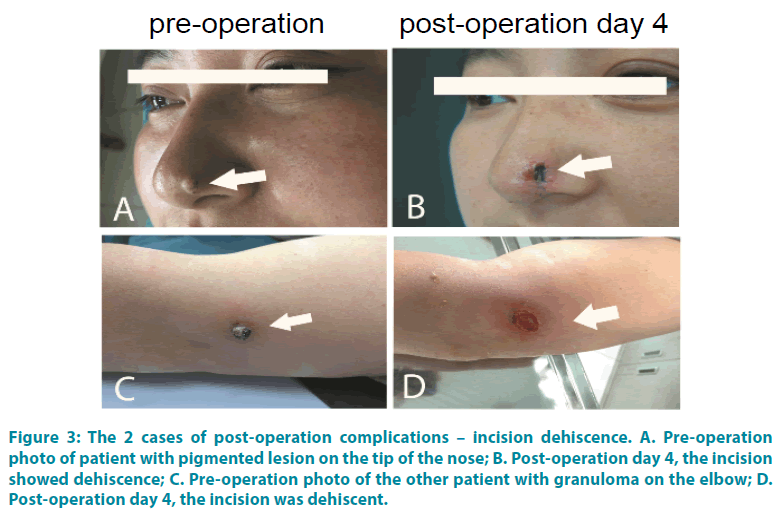
The cosmetic considerations should follow the rules of entire resection of the lesion. Out of 242 cases, only 1 case had a positive cutting edge, the rest all had negative cutting edges. The preoperation diagnosis of this exceptional case was nevus on the tip of the nose, so we did the nevus resection and closed the incision primarily. On post-operation day 4, the patient complained about the incision dehiscence. According to the pathological results, it was basal cell carcinoma with basal cutting edge positive, which was the reason why the incision was not healing. Finally, the patient had re-surgery as mentioned above. And the final pathological result confirmed the cutting edge negative. This experience suggests that differential diagnosis of benign and malignant skin tumor before surgery is important, and the frozen section pathological examination should be taken if necessary. However, the other 2 cases were cured by longtime wound care, and finally received secondary intention. Both cases were on high-tension areas of the body, one was on the tip of the nose, and the other was on the elbow (FIGURE 3). So the sub-dermal sutures should be reliable, and skin flap was applied when the tension of primary closure is too big. In addition, as the peri-nasal area has excessive sebum and sweat, post-operation incision care and wound dressing change was necessary. The prime aim of this complication series was to insure that knowledge of the existence of complications increases, that prevention can become more widely accepted and that the recognition and management of established complications can be undertaken with skill and competence [2].
Figure 3: The 2 cases of post-operation complications – incision dehiscence. A. Pre-operation photo of patient with pigmented lesion on the tip of the nose; B. Post-operation day 4, the incision showed dehiscence; C. Pre-operation photo of the other patient with granuloma on the elbow; D. Post-operation day 4, the incision was dehiscent.
Special studies for accurate diagnosis
There were 15 cases that underwent ultrasonography examination in which 3 results were differed from pathological diagnosis. The coincidence rate of diagnoses was 80%. However, the final diagnoses of these 3 cases were all dermatofibroma, while the impressions of the ultrasonography were sebaceous cyst, lipoma and folliculitis. A canonical dermatofibroma ultrasound result should be intra-dermal ovalshaped well-defined homogeneous low-echo mass, with or without enhanced shadowing [3]. The information of description and pictures on the report is as important for the diagnostic impression of ultrasound for surgeon. Clearly diagnosis should be concluded with multiple parameters rather than a single test. Likewise, the visual and palpation examination is the pre-request for clinician’s diagnosis. The dermatofibromas appear as firm, flesh-colored nodules typically.
Pre-operation diagnosis versus pathological diagnosis
136 cases had pre-operation diagnosis as nevus in which only 1 case had a final diagnosis as basal cell carcinoma (0.7%). Reeck reported 1946 cases of nevi, 30 of which were basal cell carcinoma (0.15%) in the final diagnosis [4]. For 13 other cases of seborrheic keratosis, their pre-operation diagnoses were nevi, sebaceous nevi or pigment spots. As seborrheic keratosis is very common lesion of older adults, it is easy to be confused with nevus. Usually they distribute over the skin of the face, neck, and upper trunk, normally show rough-surfaced, coin-like plaques, and vary from a few millimeters in size to several centimeters. They enlarge slowly over time and pigmented brown to black gradually. Other misdiagnosis were: 1 case of mixed tumor of the skin, pre-operation diagnosis was sebaceous cyst; 1 case of Pilar cyst, pre-operation diagnosis was lipoma; 1 case of hemangioma, pre-operation diagnosis was granuloma. Since young plastic surgeons are at the lower part of the learning curve, the experience should be accumulated by long-term [5]. So there is no shortcut in clinic, but only hard working.
Conclusion
Plastic surgeons in training should follow the rules of standard surgery. The process of the preoperation assessment, preparation and procedure also has the reference significance for in-patient surgery [6]. Skin and soft tissue lesion surgery is the best chance for basic training: including pre-op assessment, incision design, suture skill, dealing with complications, special study and pathology result consultation. Familiar with the anatomy of the skin and sub-dermal tissues all over the body is a part of the fundamental training for reconstructive and cosmetic surgery.
In our opinion, skin and soft tissue minor surgery is the basic training method for young plastic surgeons. The plastic surgery department of public general hospital has a large number of outpatients of skin and soft tissue lesions, with a variety of pathological types. This provides a good platform for the training of young plastic surgeons.
Conflict of Conflict of Interest
There is no conflict of interest to disclose.
Applicable Funding Source
The authors have financial support from Zhejiang province key science and technology innovation team (Grant No. 2013TD13), Zhejiang provincial natural science foundation of China (Grant No. LQ16H160006 & LQ16H160007), National Science Foundation for Distinguished Young Scholars of China (Grant No. 81602047, 81601710).
Acknowledgement
We would like to acknowledge the help provided by Dr. Hangfei Qi in revising this article.
References
- Henderson MM, Neumeister MW, Bueno RA Jr. Hand tumors: I. skin and soft-tissue tumors of the hand. Plast Reconstr Surg. 133(2):154-164 (2014).
- Stoddard CJ, Smith JAR. Complications of Minor Surgery. W.B. Saunders Company, Philadelphia, Pennsylvania, (1985).
- Huang ZP, Chen J, Ren J, et al. Ultrasound findings of dermatofibroma. Chin J Med Ultrasound 17(3): 484-487 (2010).
- Reeck MC, Chuang TY, Eads TJ, et al. The diagnostic yield in submitting nevi for histologic examination. J Am Acad Dermatol40(4):567-571 (1999).
- William F. Walker. A Colour Atlas of Minor Surgery. Edited by Wolfe Medical Publishers, Ltd., London(1986).
- Evans GR, Scholz T, Brandt K. Outpatient Surgery. Plast Reconstr Surg136(1):89-95 (2015).