Research Article - Interventional Cardiology (2022) Volume 14, Issue 4
Percutaneous retrieval of foreign bodies in the heart and major vessels
- Corresponding Author:
- My Hoang Tai Nguyen
Department of Interventional Cardiology,
Cho Ray Hospital, |
Ho Chi Minh City,
Vietnam,
E-mail: marknguyen.dr@gmail.com
Received date: 29-Jun-2022, Manuscript No. FMIC-22-63704; Editor assigned: 01-Jul-2022, PreQC No. FMIC-22-63704 (PQ); Reviewed date: 18-Jul-2022, QC No. FMIC-22-63704; Revised date: 25-Jul-2022, Manuscript No. FMIC-22-63704 (R); Published date: 01-Aug-2022, DOI: 10.37532/1755-5310.2022.14(4).547
Abstract
Background: Foreign bodies in the heart and major vessels usually occurs from some invasive procedural complications such as internal jugular vein catheterization for feeding or infusion of drugs, or some intervention procedures, etc. It can cause severe complications such as serious infection, hemorrhage and embolism. We review 25 cases of foreign bodies in the heart and major vessel from April 2006 to November 2019 in Cho Ray hospital.
Research design: Retrospective, case series We performed successfully 23/25 cases (92%) of percutaneous retrieval of foreign bodies in the heart and major vessels by goose-neck snares from April 2006 to November 2019 in the interventional cardiology department. The foreign bodies retrieved were a piece of a venous central catheter or a guidewire stuck in the right heart or the central venous, or stent, ASD occluder device, VSD occluder device or PFO occluder device dislodged during or just after interventional procedures.
Results: Percutaneous retrieval was successful in 23/25 patients (92%) with the use of goose-neck snares. No complications occurred during the procedures.
Conclusion: Percutaneous retrievals with goose neck snares is an effective and safe technique that should be the first choice for removing of foreign bodies in the heart and major vessels.
Keywords
Retrieval •Foreign body • Snare • Heart
Abbreviations
ASD: Atrial Septal Defect; ADO: Amplatzer Ductus Occluder; VSD: Ventricular Septal Defect; PFO: Patent Foramen Oval; DSA: Digital Subtraction Angiography
Introduction
Foreign bodies in the heart and major vessel usually occur from some invasive procedural complications such as jugular vein catheterization for feeding or infusion of drugs, it can cause serious complications: infection, hemorrhage or pulmonary embolism. These days, when more and more invasive procedures have been often utilized in clinical practice with children as well as adults, so intravascular/intracardiac foreign bodies are more commonly encountered in the real world [1,2]. Retrieval of foreign bodies in the heart or major vessel by open-heart surgery is more complex and dangerous than by percutaneous transcatheter interventional procedures. Some devices have been used to retrieve them successfully such as: goose neck snare, three-dimensional snare, grasping forcep, etc. [3-5]. The first case of intravascular percutaneous transcatheter retrieval was done more than 40 years ago to remove a foreign body that was a piece of soft guidewire stuck in the superior vena cava and right atrium [6]. Percutaneous retrieval technique of intravascular foreign bodies has now become more popular and a standard method of treatment in interventional cardiology. However, its prevelence is rare so that there have not been so many reports on this topic. In Vietnam, interventional cardiology has been recently developed since 1999, the number of percutaneous foreign body removal case is small.
The common foreign bodies are central venous catheters used in chemotherapy, hemodialysis, parenteral nutrition, long-term antibiotic therapy, or monitoring the central venous pressure in shock. After interventional cardiology is developing in Vietnam, so many interventional procedures were done. Some complications related to procedures. Therefore, some others are stents, broken balloons, ASD occluder devices, VSD occluder devices or PFO occluder devices dislodged during interventional procedures. One common complication is that the wire slips into the vessels or the catheter is broken during procedures. This fragment can move to the right heart and causes arrhythmia, systemic embolism and tricuspid valve regurgitation. In some rare situations, it can go to the pulmonary artery and causes pulmonary embolization.
We review 25 cases of percutaneous foreign bodies’ removal in the heart and major vessels from April 2006 to November 2019 in the interventional cardiology department in Cho Ray hospital.
Materials and Methods
Research design
Retrospective study
Research objects
All cases of foreign bodies stuck in the heart and major vessels have indications for percutaneous removal from April 2006 to November 2019 in the interventional cardiology department of Cho Ray hospital. Patients underwent clinical examination and complete preoperative investigation such as X-ray, CT scan or DSA fluoroscan to determine the location, length and shape of foreign body. After all, the percutaneous retrieval was carried out in the cardiac catheterization room.
The research data will be collected according to the research medical record form. Data entry using Microsoft Excel 2010 software, statistical analysis using SPSS 18.0 software.
Results
From April 2006 to November 2019 in Interventional Cardiology Department, we attempted retrievals of 25 foreign bodies in 25 patients. Retrieval was successful in 23 (92%) of 25 patients with no complications (Tables 1 and 2).
| Characteristics (n=25) | Mean ± SD n (%) |
|---|---|
| Age (*) | 42.2 ± 19.04 |
| Sex | |
| Male | 20 (80%) |
| Female | 5 (20%) |
Note: (*) the youngest patient 16 years old, the oldest 81 years old
Table 1: Characteristics of research population.
| Location of vascular access (n=25) | Mean ± SD n (%) |
|---|---|
| Vascular approach | |
| Right femoral vein | 18 (72%) |
| Left femoral vein | 2 (8%) |
| Right & Left femoral artery | 9 (36%) |
| Right femoral artery | 2 (8%) |
| Others (*) | 1 (4%) |
| Heparin (UI) | 2900 ± 730.5 |
| Preventive Antibiotics | 14 (56%) |
Note: (*) A case small incision at radial access area to take the mini-wire out
Table 2: Vascular access.
The mean dose of heparin in procedure is 2900 UI. More than 50% of patients required prophylactic antibiotics.
Procedures were approached through the right femoral venous route in 18 (72%) cases, left femoral venous route in 2 (8%) cases, both femoral venous routes in 9 (36%) cases. Goose-neck snares were used in 23 (92%) cases. In order to facilitate the full expansion of snares in the vascular space to get foreign bodies, we had to use pigtail catheter (5F) in 4 cases, JR4 catheters (5F) in 3 cases, and MP catheters (5F) in 4 cases (Tables 3 and 4).
| S No. | Location of foreign bodies | Foreign bodies | Devices | Catheter | Sheath |
|---|---|---|---|---|---|
| 1 | Pulmonary artery | ASD occluder device | Snare | Pigtail | 14 |
| 2 | Inferior Vena Cava | Guidewire 0.035 50 cm | Snare | JR 4.0 | 7 |
| 3 | Left common carotid artery-Left Ventricle | Guidewire 0.035 50 cm | Snare | JR 4.0 | 7 |
| 4 | Inferior Vena Cava–Superior Vena Cava | Guidewire 0.035 50 cm | Snare | MP | 9 |
| 5 | Right jugular vein-Inferior Vena Caval | Guidewire 0.035 50 cm | Snare | 9 | |
| 6 | Right atrium | Central vein catheter | Snare | Pigtail | 8 |
| 7 | Superior Vena Cava–Right atrium–Right ventricle | Central vein catheter | Snare | 8 | |
| 8 | Right radial artery | Mini wire | Small incision | - | |
| 9 | Inferior Vena Cava–Right iliac vein | Guidewire 0.035 50 cm | Snare | 8 | |
| 10 | Right jugular vein | Oxygen catheter (non-contrast) | Snare | 10 | |
| 11 | Right jugular vein- Superior Vena Cava | Guidewire 0.035 50 cm | Snare | 9 | |
| 12 | Superior Vena Cava–Right atrium | Hickman catheter | Snare | 10 | |
| 13 | Pulmonary artery | ASD occluder device | Snare | 10 | |
| 14 | Superior Vena Cava–Right femoral vein | Guidewire 0.035 50 cm | Snare | Pigtail | 8 |
| 15 | Inferior Vena Cava–Right atrium | Central vein Catheter | Snare | 10 | |
| 16 | Right ventricle–Pulmonary artery | Pace maker electrode | Snare | Pigtail | 8 |
| 17 | Right jugular vein–Inferior Vena Cava | Guidewire 0.035 50 cm | Snare | MP catheter (5F) | 8 |
| 18 | Right subclavicular vein–Inferior Vena Cava | Guidewire 0.035 50 cm | Snare | MP catheter (5F) | 8 |
| 19 | Superior Vena Cava–Inferior Vena Cava | Guidewire 0.035 50 cm | Snare | 10 | |
| 20 | Left Pulmonary artery | Device ADO I 16/14 | Snare | 12 | |
| 21 | Right Pulmonary artery | Device ADO II 5/4 | Snare | JR 4.0; MP | 10 |
| 22 | Superior Vena Cava–Inferior Vena Cava | Central vein Catheter 10F 40 cm | Snare | 14 | |
| 23 | Superior Vena Cava–Inferior Vena Cava | Central vein Catheter | Snare | 7 | |
| 24 | Superior Vena Cava–Inferior Vena Cava | Guidewire 0.035 50 cm | Snare | 7 | |
| 25 | Abluminal Aorta | Renal stent 5 × 18 mm | Snare | 8 |
Table 3: Characteristics of retrieval procedures.
| Results | Frequency (%) n (%) |
|---|---|
| Technical success | 23 (92%) |
| Procedural success | 22 (88%) |
| Procedural duration (minute) | 57,0 ± 15,3 (Mean ± SD) |
| Complications | 0 |
Table 4: Results of taking foreign bodies.
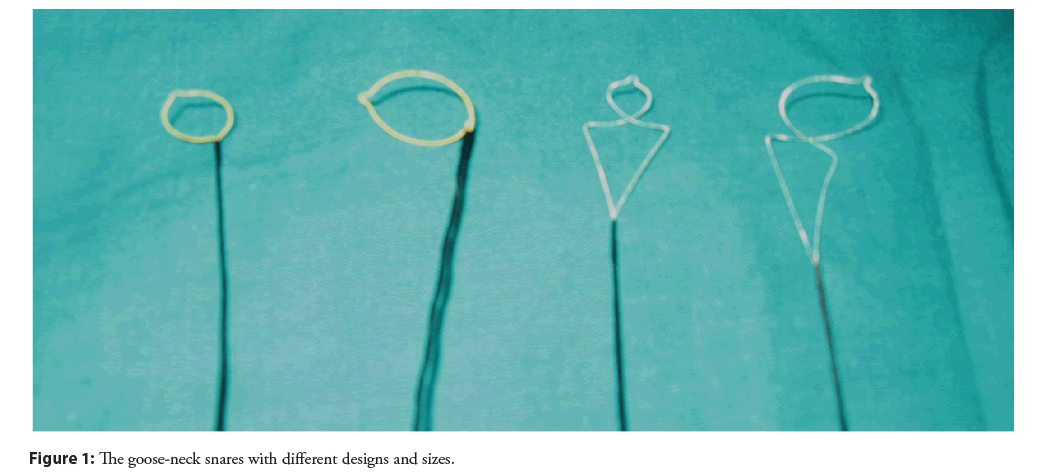
Twenty-five cases of foreign bodies were complications from vascular procedures in other hospitals or specialties (not interventional cardiology). Four cases were complications from congenital heart transcatheter closure procedures in our cath lab including two ASD occluder devices migration after half of a month and two months of deployment, one ADO I (Amplatzer Ductus Occluder) migration after six months of deployment and one ADO II (Amplatzer Ductus Occluder) dislodge during VSD closure procedure. All the occluder devices were stuck in the pulmonary artery. One ASD occluder device was retrieved successfully by goose-neck snare. Other ASD occluder devices were failed for percutaenous retrieval so that patients were sent to open heart surgeries. Two Amplatzer Ductus Occluder (ADO) devices were taken out of the pulmonary artery successfully by different goose-neck snares (Figure 1).
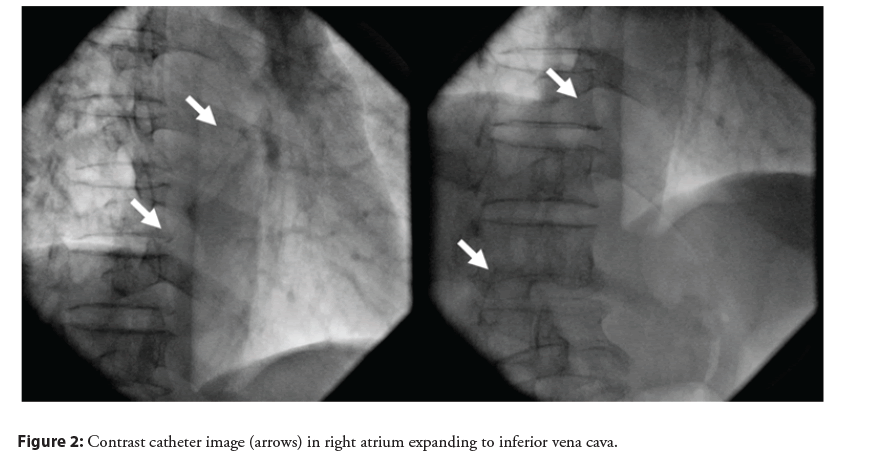
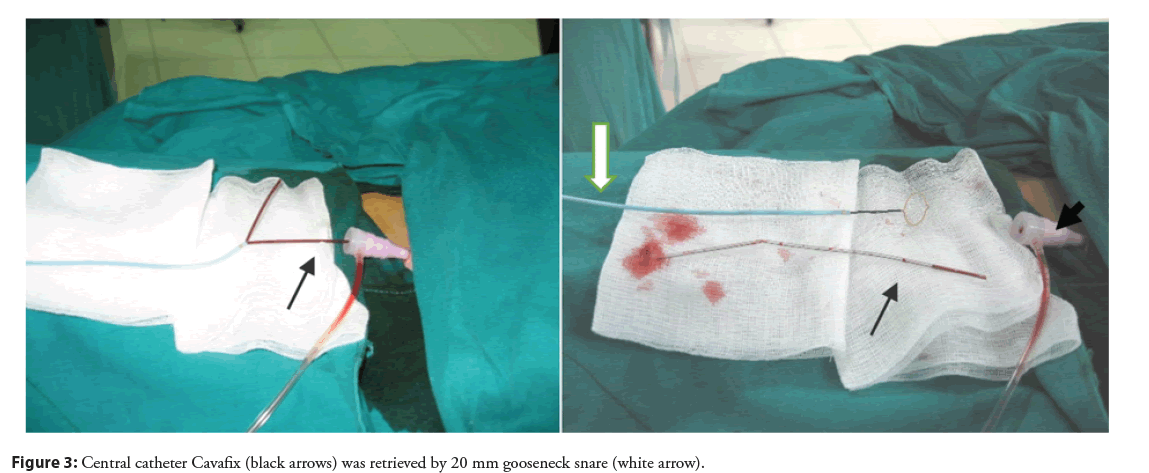
The other foreign bodies include 12 guidewires, 5 central vein catheters, 1 Hickman catheter, 1 oxygen catheter and 1 broken electrode wire. All the guidewires and central catheters were contrast during the fluoroscan (Figure 2). Therefore, they were retrieved successfully (Figure 3). Except from one 50 cm oxygen catheter, we could not take it out under the fluoroscan. Because it was attached to the central vein and too difficult to remove.
One old and frail patient (82 years old) died during hospitalization because of a severe pulmonary infection, not involved retrieval procedure.
Discussion
Although percutaneous retrieval of foreign bodies in the heart and major blood vessels is not a new concept in the world, in Cho Ray hospital as well as in many medical centers in southern provinces of Vietnam, these are the first cases to perform retrieval of foreign bodies in the heart and major vessels by percutaneous transcatheter procedures. We do not have much experience and almost the cases were done by expert tutorials. The foreign bodies in the heart and large blood vessels were broken catheter fragments or guidewires, stents, and some occluder devices that dislodged in interventional procedures. All of them had one free head in the vascular space so that it was able to catch by a goose-neck snare. According to Cekirge, et al. the goose-neck snare is the first device used when removing foreign bodies in the heart and major blood vessels [5,7]. The diameter of the snare ring is usually chosen equal to the vessel’s one where the foreign body is located. We used the snare with the 20 mm ring diameter for all the cases. According to some reports, the snare can successfully remove most of the foreign bodies in the heart and major blood vessels [3,4]. Even though there were many other retrieval devices such as forceps, baskets, etc., the goose-neck snare has still been the most simple and effective tool (Figure 1).
A 3-year, single-center experience of Bonvini, et al. [1] reported most foreign bodies in the heart and major vessels were fragments of feeding or infusion intravenous catheters and were successfully removed by transcatheter with no complications. Cantarelli, et al. In San Paulo between 1985 and 1991 reported that broken catheters were the common foreign bodies in the heart (14 of 15 cases) and all of them were successfully removed by a goose-neck snare [2].
In our series cases, the retrieval was successful in 23 (92%) of 25 cases without immediate complications. The result is comparable with some studies [3,8].
As interventional cardiology develops, the nature of foreign bodies also changes. Nowadays, foreign bodies are usually interventional equipment. Many authors summarized that the foreign bodies almost include electrode wire, stent, inferior vena cava filter, valve balloon, coils, ASD occluder, VSD occluder [3,4,8]. However, the removal procedure can still succeed with a goose-neck snare. We fail to retrieve one ASD occluder migration into the pulmonary artery case. This occluder, after that, was removed by open-heart surgery without complication.
The mean time of our retrieval procedure is 57 minutes. It is longer than the procedure time of Egglin, et al. which is just 15 to 30 minutes. We have not had so much experience in retrieving foreign bodies, therefore it might take us longer compared with other authors [3,4].
Illustrated case
A male patient, 82-year-old, was on the third day of postoperative due to gastric perforation complications of septic shock. When a right jugular catheter procedure was done, the patient was agitation. A piece of Cavafix catheter was broken and moved to the venous system. The X-ray film and echocardiography revealed that a fragment of the catheter was in the right atrial. Observation under a luminous fluorescent screen showed this fragment from the right atrial to the inferior vena cava (Figure 2). The 13 cm Cavafix catheter fragment was successfully removed by percutaneous retrieval technique without any complications (Figure 3). The total time of this procedure was 30 minutes.
Conclusion
Percutaneous retrieval of foreign bodies in the heart and large blood vessels is not a new concept in the world but these were the first cases in Vietnam. This procedure is simple and proven to be safe, effective, and has a high success rate (92%) without any complications. This procedure saves and prevents the patient from having to undergo open-heart surgery and shortens the hospital stay. In our opinion, the percutaneous retrieval technique of foreign bodies should be the first choice for removing foreign bodies in the heart and major vessels.
References
- Bonvini RF, Rastan A, Sixt S, et al. Percutaneous retrieval of intravascular and intracardiac foreign bodies with a dedicated three-dimensional snare: A 3-year single center experience. Catheter Cardiovasc Interv. 74(6): 939-45 (2009).
[CrossRef] [Google Scholar] [PubMed]
- Cantarelli MJ, de Paola Ade A, Alves CM, et al. Percutaneous retrieval of intravascular foreign bodies. Arq Bras Cardiol. 60(3): 171-5 (1993).
[PubMed]
- Egglin TK, Dickey KW, Rosenblatt M, et al. Retrieval of intravascular foreign bodies: Experience in 32 cases. AJR Am J Roentgenol. 164(5): 1259-12643 (1995).
[CrossRef] [Google Scholar] [PubMed]
- Erdmann E. Percutaneous transfemoral foreign body removal from the heart or great vessels. Dtsch Med Wochenschr. 113(41): 1594-7 (1988).
[CrossRef] [Google Scholar] [PubMed]
- Woodhouse JB, Uberoi R. Techniques for intravascular foreign body retrieval. Cardiovasc Intervent Radiol. 36(4): 888-9 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Thomas J, Sinclair SB, Bloomfield D, et al. Nonsurgical retrieval of a broken segment of steel spring guide from right atrium and inferior vena cava. Circulation. 30: 106-108 (1964).
[CrossRef] [Google Scholar] [PubMed]
- Cekirge S, Foster A, Weiss J, et al. Percutaneous removal of an embolized Wallstent during a tmansjugular intrahepatic portosystemic shunt procedure. J Vasc Lnteiv Radiol. 4(4): 559-560 (1993).
[CrossRef] [Google Scholar] [PubMed]
- Carroll M, Ahanchi SS, Kim JH, et al. Endovascular foreign body retrieval. J Vasc Surg. 57(2): 459-63 (2013).
[CrossRef] [Google Scholar] (All versions) [PubMed]