Mini Review - Interventional Cardiology (2022) Volume 14, Issue 6
Percutaneous transluminal caval flow regulation PTCR®: A step forward in the evolution of the HFrEF treatment paradigm
- Corresponding Author:
- José E. Herrera
Asociación Cardiológica de Occidente, ASCARDIO,
Universidad Central ‘Lisandro Alvarado’ (UCLA),
Barquisimeto 3001,
Venezuela,
E-mail: jhcardio@live.com
Received date: 20-Oct-2022, Manuscript No. FMIC-22-77844; Editor assigned: 24-Oct-2022, PreQC No. FMIC-22-77844 (PQ); Reviewed date: 07-Nov-2022, QC No. FMIC-22-77844; Revised date: 14-Nov-2022, Manuscript No. FMIC-22-77844 (R); Published date: 21-Nov-2022, DOI: 10.37532/1755- 5310.2022.14(6).581
Abstract
Percutaneous Transluminal Caval flow Regulation (PTCR) is an emerging alternative therapy to treat patients with Acute Heart Failure (AHF). AHF represents the first cause of hospitalization in elderly persons and is the main determinant of the huge healthcare expenditure related to Heart Failure (HF). Despite therapeutic advances, the prognosis of AHF is poor, with in-hospital mortality ranging from 4% to 7%, 60 to 90-day mortality. To reverse this situation, a balloon catheter medical device has been designed to produce cyclic occlusions of the Inferior Vena Cava (IVC) supported by the phases of respiration, thus having subtotal occlusion during expiration and total occlusion during inspiration, producing an intermittent regulation of venous return or preload from the IVC to the right atrium. This PTCR procedure is minimally invasive. It is performed through the insertion of the balloon catheter via the femoral vein. This catheter is advanced to the IVC guided by echocardiogram or fluoroscopy to be placed prior to drainage of the hepatic vein. At this point, the balloon is inflated up to 70% to 80% of the diameter of the IVC in expiration, which has to be previously evaluated by echocardiography. Then inspiratory collapse (20 to 30% average) of the IVC diameter produces total occlusion during inspiration and a partial or subtotal occlusion during expiration, thereby regulating caval flow in an intermittent manner.
This innovative procedure is aimed at regulating the hypervolemia present in the IVC, normalizing venous return, preload, intracardiac pressures, biventricular diastolic and systolic diameters, diastolic and systolic volume, thus, obtaining reduction of Total Cardiac Burden (TCB) and producing a reversal of ventricular remodeling. In this manner the heart returns close to its original design, with improvement in Ejection Fraction (EF) and cardiac output.
Keywords
Percutaneous transluminal caval flow regulation •Inferior vena cava Heart failure • Catheter balloon • Medical devices • Cardiac output • Ejection fraction
Abbrevations
HFrEF: Heart failure with reduced Ejection Fraction; PTCR: Percutaneous Transluminal Caval Flow Regulation; HV: Hypervolemia; TCB: Total Cardiac Burden; ED: Expiration Diameter; ID: Inspiration Diameter; IVC: Inferior Vena Cava, CO: Cardiac Output; AHF: Acute Heart Failure; HF: Heart Failure; EF: Ejection Fraction.
Introduction
According to the American Heart Association there are approximately 6.2 million Heart Failure (HF) patients in the US alone [1], 64.3 worldwide. In 2018, HF was mentioned in 379,800 death certificates (13.4%) [1]. Heart failure projected to increase dramatically, according to new statistics. Heart Failure Projection In Future: The number of people diagnosed with heart failure is increasing and projected to rise by 46 percent by 2030, resulting in more than 8 million people with heart failure, according to the American Heart Association’s 2017 Heart Disease and Stroke Statistics Update (link opens in new window) published Wednesday [1].
HF cost the nation an estimated $30.7 billion in 2012 [2]. This total includes the cost of health care services, medications to treat HF, and lost work days. Nearly 1 in 4 HF patients are readmitted within 30 days of discharge and approximately half are readmitted within 60 days. These patients have to go to the hospital every 90 days for 4–5 day decongestant treatment with the use of potent diuretics. 25% of the 6.2 million HF patients in the US represent 1.7 million patients who are our target patients for use of our procedure Transluminal Caval flow Regulation PTCR and Catheter Medical Device.
This great reality shown with its statistics, creates a rather bleak picture because until now current therapies have not been able to, significantly, reduce hospital readmissions of patients with acute or chronic decompensated HF and treat pulmonary congestion, which endangers patient’s life.
With this review of our article where we show our experience in humans using our procedure, we want to make it well established that, with the results obtained, our procedure and device represent a new alternative to treat HF patients with great advantages over current therapies. This is due to the fact that it is a safe temporary therapy, without collateral effects, and very effective in achieving hemodynamic and echocardiographic benefits. Thus, meaning a true innovation, capable of changing the paradigm of HF treatment with great benefits for patients and great savings for the state health service (Table 1) [3,4].
| Prevalence | Annual Mortality | Costs |
|---|---|---|
| About 2% total population, 6.2 million adults in the United States have heart failure [3]. | In 2018, heart failure was mentioned on 379,800 death certificates (13.4%) [3]. | Heart failure costs the nation an estimated $30.7 billion in 2012 [4]. This total includes the cost of health care services, medicines to treat heart failure, and missed days of work. |
Table 1: Facts about heart failure in the United States.
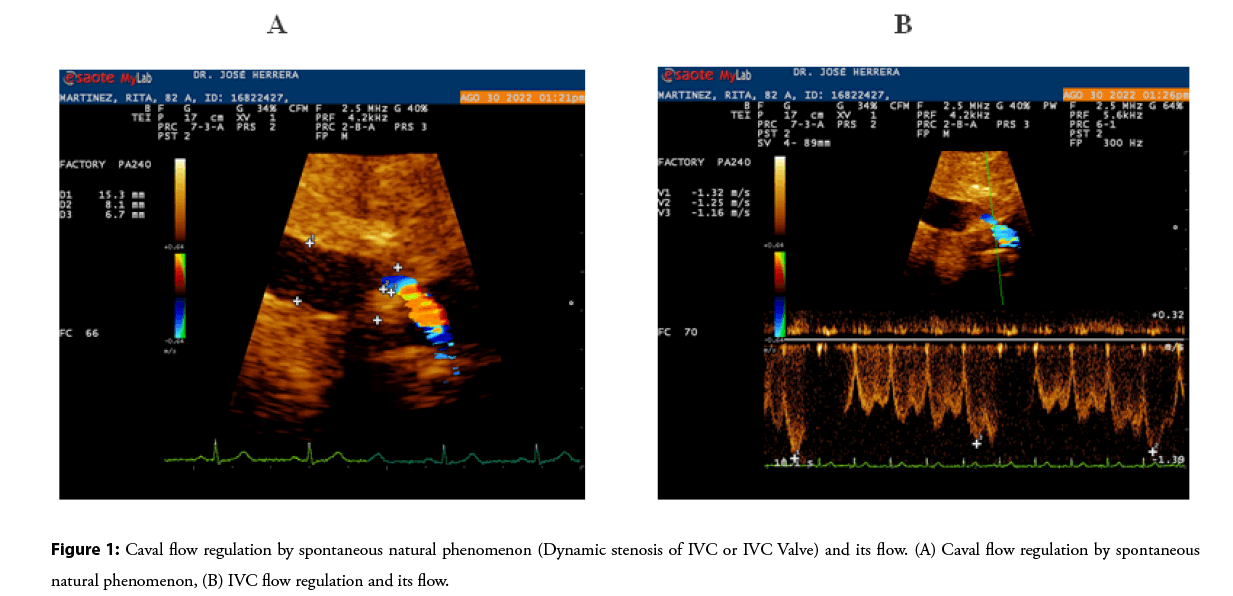
PTCR is mimicking a spontaneous natural phenomenon capable of regulating hypervolemia and cardiac venous return called Inferior Vena Caval Dynamic Stenosis (Figure 1) [5]. This spontaneous natural phenomenon is produced by the development of a fibrocalcic formation in the right Cavodiaphragmatic junction, producing intermittent occlusions of the IVC sustained by the respiratory phases; thus, we have total occlusion of the IVC during inspiration and subtotal during expiration. Inspiratory vena cava collapse plays an important role in producing intermittent inferior vena cava occlusions, resulting in intermittent venous blood flow from the IVC to the right atrium. This spontaneous natural phenomenon produces an effect similar to that of a valve, capable of reducing venous return, therefore preload, total cardiac load resulting in a marked decrease in biventricular diameters and volumes (Video 1).
Video 1: Spontaneous natural phenomenon caval flow regulator (dynamic stenosis of cava or caval valve).
Figure 1: Caval flow regulation by spontaneous natural phenomenon (Dynamic stenosis of IVC or IVC Valve) and its flow. (A) Caval flow regulation by spontaneous natural phenomenon, (B) IVC flow regulation and its flow.
The PTCR Procedure
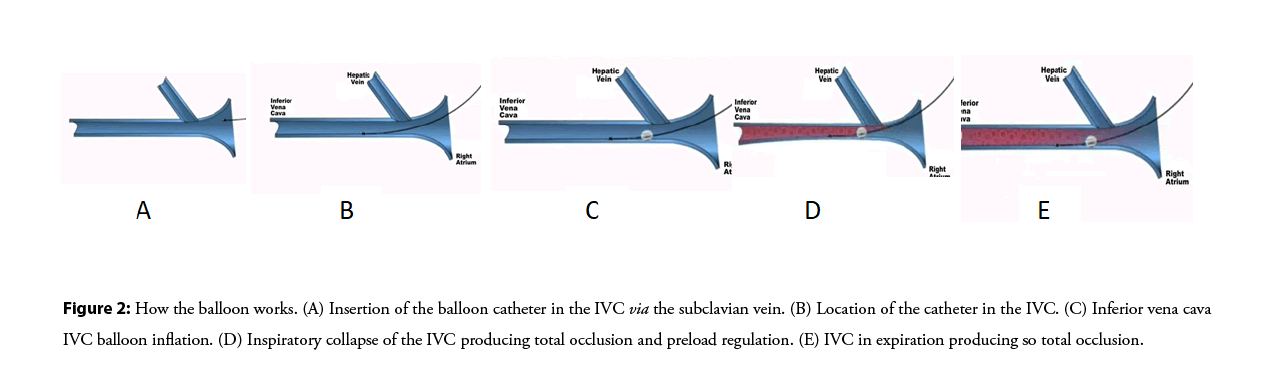
The methodology to implement the PTCR procedure consists of a series of rules that guarantee the function of regulating venous return, preload and therefore the total cardiac burden (Figure 2).
The diameter of the caval balloon is related to the anteroposterior diameter of the IVC at the time of inspiratory collapse. For example, if the expiratory diameter is 18 mm and the collapse is 30% (5,4 mm), it would suffice to subtract 18 mm (diameter in expiration)-5,4 mm (diameter in inspiration)=Balloon size must be inflated until reaching 12,6 mm and so on for any other case (Video 2).
Video 2: How the IVC flow regulator balloon works.
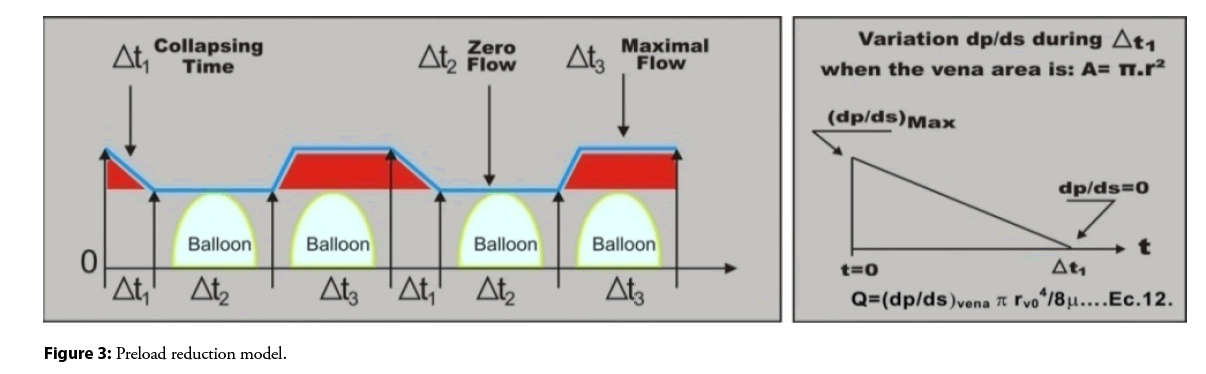
Mathematical Model to Explain the Operation of the PTCR
Cyclic variation of the radius r of a section of the vena cava near the balloon. The maximum radius is r0 vena cava. At time of collapse Δ t1, the radius decreases from r0 to the balloon radius rb. During the time Δ t2, the vein remains radius r=rb no flow. During the time Δ t3, the vein returns to its normal radius and blood flows into the atrium. The balloon acts as a regulator of preload (flow to the heart) (Figures 2 and 3). We are annexing supplementary material with the mathematical support through the equations carried out that allowed us to reach the final equation that governs and validates this procedure to be applied in humans.
Figure 2: How the balloon works. (A) Insertion of the balloon catheter in the IVC via the subclavian vein. (B) Location of the catheter in the IVC. (C) Inferior vena cava IVC balloon inflation. (D) Inspiratory collapse of the IVC producing total occlusion and preload regulation. (E) IVC in expiration producing so total occlusion.
PTCR is a minimally invasive percutaneous therapy, supported by the patient’s physiology, designed to fulfill two important functions. The first is to reduce hypervolemia present in 90% of cases with HF [5]; thereby reducing total cardiac burden. The second function is to prevent the increased blood pressure in the right atrium in patients with HF from being transmitted to the IVC during inspiration, thereby reducing the pressure in the IVC and favoring renal venous return. The higher the breathing frequency, the greater the preload regulation [5].
Acute hemodynamic and echocardiographic effects experience in 6 patients with HF treated using PTCR [5,6], showed a cyclic occlusion of the IVC and an intermittent reduction in caval flow (cardiac preload) as reported by the authors. PTCR resulted in a significant reduction in mean right atrium pressure, systolic right ventricular pressure, mean pulmonary artery pressure, and mean pulmonary capillary wedge pressure with no significant increase in cardiac output.
It is worth saying that this reduction of the average intracardiac pressures, approximately 30% [5], with respect to their initial measurements during the use of the PTCR, means a pseudo normalization of the intracardiac pressures and a very close return to the original cardiac design, significantly reducing pulmonary congestion.
The size of the balloon was calculated with the help of a mathematical equation using an example and the diameter of the ideal balloon to produce preload regulation is related to the diameter of the IVC, during the inspiratory collapse produced by the inspiratory phase of respiration.
This study was designed to evaluate 10 patients, but only 6 met the inclusion criteria in the study, so this number of patients is our greatest limitation. It is recommended to carry out a further study involving a greater number of patients.
No procedure-related complications were observed in this study and there was no liver or kidney function impairment in the short or long 2-year follow-up.
Discussion
After observing these results, we are convinced that the PTCR procedure leads to great hemodynamic, echocardiographic, and clinical benefits for the patient by achieving a reduction in total cardiac burden, producing a significant reduction in biventricular volumes and diameters when used alone: 30 minutes in each evaluated patient. It is becoming an emerging therapy to treat patients with both acute and chronic HF, evolving the chronic heart failure treatment paradigm in cardiology, given the versatility of the catheter that allows the IVC to be accessed either through the subclavian vein or the femoral vein. This emerging therapeutic strategy could be very useful as well, to effectively and safely treat pregnant patients where traditional treatment cannot be used due to side effects and stillbirth, and also this therapy can be used in patients with HF postpartum, in this way avoid the passage of drugs through breastfeeding.
Future Directions
The PTCR is a procedure to reduce the total cardiac burden without side effects and very low complications. In an effective way, constitutes an innovation in the management of HF, demonstrated in recently published results [5,6]. This procedure can be used to treat patients with acute and chronic HF and given the versatility of the balloon catheter medical device, it can be inserted via the femoral vein to treat cases of patients with acute HF or via the subclavian vein to treat patients with chronic HF so that they can go home with their total cardiac load-regulating balloon for more than 3 months. Thus markedly decrease readmissions at 90 days, 160 days and annual mortality due to HF. In this way quality of life is given to the patient, prompt incorporation into family and working activities and a large reduction in health spending for the state. Based on these statements, the PTCR will have the potential to reduce the total cardiac burden and heart Failure progression.
PTCR is a new alternative to reduce total cardiac burden and treat patients with heart failure, reducing intracardiac pressures, biventricular volumes, ventricular diameters, ventricular filling pressure and ventricular wall stress, resulting in clinical benefits such as reduced pulmonary congestion and improving cardiac output, without side effects. It has demonstrated to date to be a safe and effective procedure. More studies are needed with a larger number of patients to confirm our initial observation in our study.
References
- Heart failure projected to increase dramatically, according to new statistics
- Constanzo MR, Guglin ME, Saltzberg MT, et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 49(6): 675-683 (2007).
[CrossRef] [Google Scholar] [PubMed]
- Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 Update: A report from the American Heart Association. Circulation. 141(9): e139-596 (2020).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: A report from the American Heart Association. Circulation. 139(10): e56-528 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Herrera JE, Herrera JA, Finizola B, et al. First-in-human experience of preload regulation with percutaneous transluminal caval flow regulation in heart failure with reduced ejection fraction patients. ESC Heart Fail. 9(2): 1118-1126 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Herrera JE, Cubeddu R, Torres W, et al. TCT-733 acute hemodynamic effects percutaneous transluminal caval flow intermittent restriction with balloon in ischemic and non-ischemic heart failure patients. J Am Coll Cardiol. 66(S15): B299 (2015).