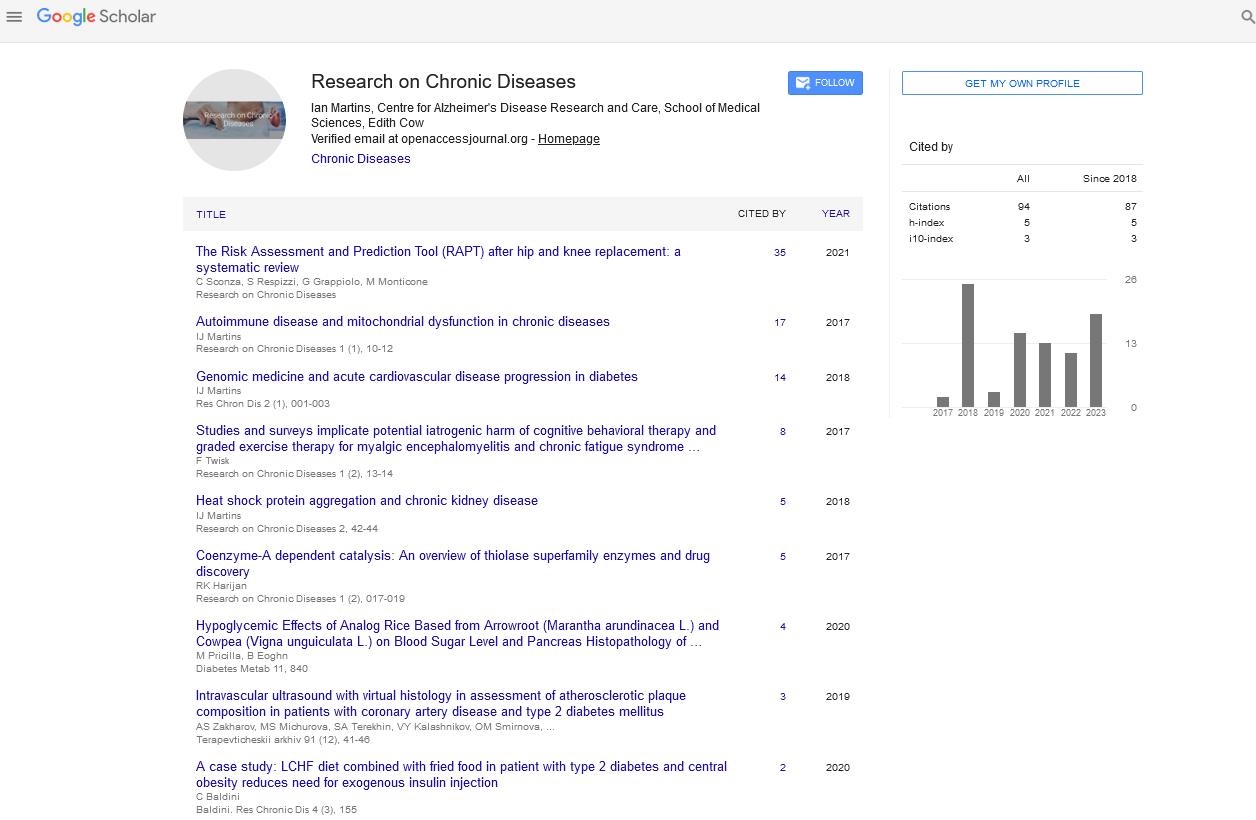
Editorial - Research on Chronic Diseases (2023) Volume 7, Issue 3
Periodontal disease in Adaptive immune response
Dr. Feng Li*
Department of immunology Science, University of Ha’il, Saudi Arabia, College of Engineering science
Department of immunology Science, University of Ha’il, Saudi Arabia, College of Engineering science
E-mail: fengl@gmail.com
Received: 01-5-2023, Manuscript No. oarcd-23-99359; Editor assigned: 03- 5-2023, Pre QC No. oarcd-23-99359.; Reviewed: 17-5-2023, QC No. 99359; Revised: 23-5-2023, Manuscript No. oarcd-23-99359 (R); Published: 30-5-2023; DOI: 10.37532/ rcd.2023.7(3).048-050
Abstract
Periodontal diseases affect between 20 and 50 percent of the world’s population and are common in developed and developing nations alike. Periodontal disease is a public health issue due to its high prevalence in adults, teens, and older people. Periodontal diseases are associated with a number of risk factors, including smoking, poor oral hygiene, diabetes, medication, age, hereditary factors, stress, and others. Periodontal diseases are linked to systemic conditions like diabetes, cardiovascular disease, and poor pregnancy outcomes, according to solid evidence. Periodontal disease is likely to raise the risk of cardiovascular disease by 19%, and this relative risk rises to 44% in people over the age of 65. Type 2 diabetic people with serious type of periodontal illness have 3.2 times more noteworthy mortality risk contrasted and people with no or gentle periodontitis. In patients with type 2 diabetes, it has been demonstrated that periodontal therapy improves glycemic control. Periodontitis is connected with maternal contamination, preterm birth, low birth weight, and toxemia. Oral illness avoidance procedures ought to be consolidated in constant foundational sickness preventive drives to reduce the weight of sickness in populaces. Maturing is related with the improvement of sickness. Periodontal sickness is one of the numerous illnesses and conditions that expansion in commonness with age. Notwithstanding the conventional spotlight on individual age-related conditions, there is currently a more noteworthy acknowledgment that multi-framework conditions, for example, fragility assume a significant part in the soundness of more established populaces. In older adults, frailty is a clinical condition that increases the likelihood of adverse health outcomes. Both delicacy and periodontal sickness are normal ongoing circumstances in more seasoned populaces and offer a few gamble factors. Periodontal disease and frailty likely have a reciprocal relationship. A better understanding of age-related diseases and therapeutic targets for improved management of frailty and periodontal disease may result from investigating age-related changes in immune cells that regulate inflammation.
Keywords
Periodontal disease • Epidemiology • Risk factors • Systemic disease • Preventive strategy
Introduction
The primary cause of tooth loss and one of the two greatest threats to oral health is periodontal disease, which is a chronic inflammatory disease of the periodontium.1,2 There are approximately 800 species of bacteria that have been identified in the oral cavity3, and it is hypothesized that periodontal disease can result from the complex interaction of bacterial infection and host response, modified by behavioral factors such as smoking.4 The purpose of this review is twofold: 1) to talk about ways to prevent and treat periodontal disease, as well as risk factors, the prevalence of the disease in various populations, and its connection to other systemic diseases. Chronic diseases and age-related health conditions, which have a negative impact on older people’s health and quality of life3, are also strongly linked to aging. It has been accounted for that more established people 65 years or more have something like one constant condition1. In the United States, 38% of people had 0–1 chronic condition, while 47% had 2–3. Additionally, oral health-related chronic conditions are crucial to the health of older populations. Periodontal disease is one of the most common chronic diseases worldwide and gets more common as people get older4,5. For older people to maintain their quality of life, functional performance, and overall systemic health, proper oral health care is essential. Multi-system conditions like frailty play an important The primary cause of tooth loss and one of the two greatest threats to oral health is periodontal disease, which is a chronic inflammatory disease of the periodontium.1,2 There are approximately 800 species of bacteria that have been identified in the oral cavity3, and it is hypothesized that periodontal disease can result from the complex interaction of bacterial infection and host response, modified by behavioral factors such as smoking.4 The purpose of this review is twofold: 1) to talk about ways to prevent and treat periodontal disease, as well as risk factors, the prevalence of the disease in various populations, and its connection to other systemic diseases. Chronic diseases and age-related health conditions, which have a negative impact on older people’s health and quality of life3, are also strongly linked to aging. It has been accounted for that more established people 65 years or more have something like one constant condition1. In the United States, 38% of people had 0–1 chronic condition, while 47% had 2–3. Additionally, oral health-related chronic conditions are crucial to the health of older populations. Periodontal disease is one of the most common chronic diseases worldwide and gets more common as people get older4,5. For older people to maintain their quality of life, functional performance, and overall systemic health, proper oral health care is essential. Multi-system conditions like frailty play an important role in the health of older populations, which is now more widely recognized than in the past. This is in addition to the traditional focus on single (or related) chronic diseases. “a clinically recognizable state of increased vulnerability, resulting from aging-associated decline in reserve and function across multiple physiologic systems such that the ability to cope with daily or acute stressors is compromised”6 is the definition of frailty. In older adults, frailty is a common clinical syndrome or condition that raises the risk of negative health outcomes like falls, disability, hospitalization, death, and long-term care7. The incidence of frailty rises dramatically with age, much like the prevalence of chronic diseases like periodontal disease [1,2]. Additionally, it has been suggested that oral diseases like periodontal disease may raise the risk of frailty. Unloading this bi-directional relationship among feebleness and periodontal sickness justifies further examination. Improved management and treatment of frail older people’s frailty as well as periodontal disease may result from a deeper comprehension of these associations. In addition, gaining an understanding of the mechanistic biological pathways that lie behind frailty and periodontal disease will provide deeper insights that have the potential to enhance older people’s diagnosis and individualized treatment options. The epidemiology, risk factors, and connections between frailty and periodontal disease are all discussed in this manuscript. In addition, the manuscript will discuss the pathophysiological effects of aging-related molecular and cellular changes that may contribute to both frailty and periodontal disease. In the end, the manuscript will come to a conclusion that has implications for both research and clinical care [3,4]. As has been referenced already, the more drawn out life expectancy implies that the teeth and supporting designs keep on being utilized and presented to microscopic organisms any more. The prevalence of periodontal disease in the elderly, changes in risk factors, particular medical conditions, issues related to periodontal disease management and maintenance, and peri-implant infections are all briefly discussed in this article [5,6].
Adaptive immune response
The activity of T cells and B cells, as well as the production of antibodies and cellular immunity that goes along with it, typically characterize activation of the adaptive immune response105. Innocent lymphocytes can perceive antigens and mount a reaction during disease and memory lymphocytes are prepared to take into consideration a more fast reaction to recently experienced antigens. Low numbers of T and B cells in the periodontium indicate a varied immunoglobulin repertoire in response to the oral micro biota in the crevicular fluid106. Periodontal disease causes an increased adaptive immune response and a shift in the immunoglobulin repertoire toward a more uniform response to pathogens. The senescentassociated secretory phenotype (SASP)126, senescent cells’ characteristic pro-inflammatory phenotype, appears to be the cause of their detrimental effects on tissue [7,8]. Numerous pro-inflammatory cytokines, chemokines, and other proteins and molecules are secreted by the SASP. In an additional effort to prevent malignancy127, it appears that the SASP’s function is to maintain the cell cycle arrest in an autocrine manner and to induce senescence in nearby cells. Nonetheless, the collection and proceeded with creation of SASP compounds is unfavorable to the encompassing tissues and cells bringing about hindered tissue capability and the improvement of a persistent provocative environment128. Hence, cell senescence is thought to be an essential jumper of inflammaging129. Senescent cell accumulation has also been linked to a wide range of chronic inflammatory conditions that get worse with age, just as inflammation-aging is linked to diseases that come with getting older. In human and creature studies, aggregation of senescent cells has been related with macular degeneration130, ongoing deterrent aspiratory disease131, dementia132, Parkinson disease133, osteoarthritis134, and atherosclerosis [9,10].
Conclusion
Despite the fact that periodontal disease is the most common infectious oral condition, it can be treated and avoided. Periodontal disease’s associated systemic diseases and complications may also decrease as its incidence and prevalence decrease. Reduced prevalence of periodontal disease has the potential to reduce the need for treatment and the financial burden on healthcare systems. High pervasiveness of periodontal illness additionally requires the foundation of observation framework for oral sicknesses locally. In order to lessen the severity of other chronic diseases, prevention programs for periodontal disease ought to make use of common risk strategies. Practical procedures would likewise improve interdisciplinary joint efforts among medical services suppliers. The relationship of maturing, fragility, and periodontal illness is upheld by the epidemiological and fundamental cell and atomic exploration introduced here (Figure 1). Periodontal disease and frailty in older people must be addressed urgently in light of the worldwide population’s rapid aging. Based on our current knowledge, it is clear that agingrelated pathophysiological changes contribute to periodontal disease. This could partially explain the higher prevalence of periodontal disease in older, frailer populations. An appreciation for the age-related changes that add to periodontal infection will prompt extended translational work creating novel ways to deal with finding and treatment of periodontal sickness.
References
- Savage A, Eaton KA, Moles DR et al. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J. Periodontol.36, 458-467(2009).
- Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol.71, 743-751 (2000).
- Hirschfeld L, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 49, 225-237(1978).
- Ryder MI. The influence of smoking on host responses in periodontal infections. Periodontology. 43, 267-277(2007).
- Bergström J, Boström L. Tobacco smoking and periodontal hemorrhagic responsiveness. J Clin Periodontol. 28: 680-685(2001).
- Listl S, Galloway J, Mossey PA et al. Global Economic Impact of Dental Diseases. J. Dent. Res. 94, 1355-61(2015).
- Forshaw RJ. Dental health and disease in ancient Egypt. British Dental Journal. 206, 421-424(2009).
- Loos, Bruno G. Systemic markers of inflammation in periodontitis. J Periodontol. 76, 2106-2115(2005).
- Ekanayaka A. Tooth mortality in plantation workers and residents in Sri Lanka. Community Dent. Oral Epidemiol. 12, 128-135(1984).
- Michaud, Dominique S Izard, Jacques. Microbiota, Oral Microbiome, and Pancreatic Cancer. Int J Cancer.20, 203-206(2014).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref