Review Article - Imaging in Medicine (2016) Volume 8, Issue 3
Peripheral vein locating techniques
- *Corresponding Author:
- Zehava
Ovadia-Blechman
Department of Medical Engineering
Afeka Tel Aviv Academic College of Engineering
Tel Aviv, Israel
Tel: +972-3-7688696
Email: zehava@afeka.ac.il
Abstract
This article summarizes available methods for improving venous prominence and reviews the variety of devices for locating peripheral veins. The technologies underlying these devices, both those in use and under development, are described in terms of the advantages and disadvantages of their physical properties, their success rate in difficult cases and their current market price. The selection of the optimal technology for different conditions is also described. All existing technologies improve the success rate of nurses and paramedics in locating veins, save time and money and increase patient and medical staff satisfaction.
Keywords
peripheral intravenous catheterization, locating peripheral veins, venous locating techniques
Introduction
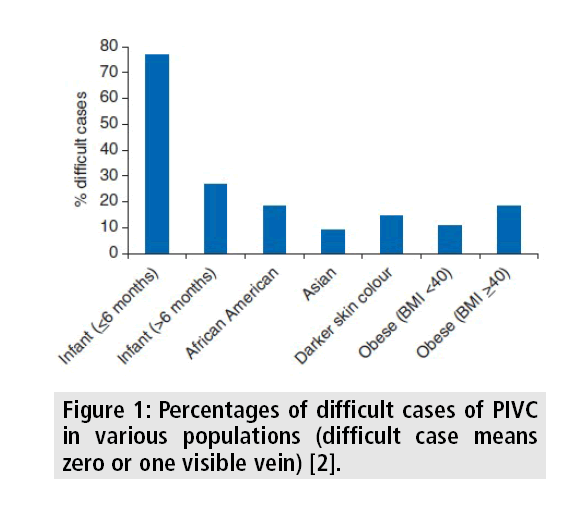
Peripheral intravenous catheterization (PIVC) is one of the most common minimally invasive medical procedures performed in hospitals today. Up to 80% of all patients admitted to hospitals worldwide will have a peripheral intravenous line inserted in the forearm or hand to administer fluids, medications, and blood products. The procedure, which is considered indispensable to human health [1], can be especially difficult in infants and elderly people, as well as in obese patients, dark skinned people, intravenous drug abusers, hypotensive individuals, and those with multiple injuries that limit the number of available limbs and may require several attempts, causing distress. The percentages of difficult cases in populations of interest was already published and are presented in FIGURE 1 [2]. Difficult venous access affects more than one-third of patients at hemophilia treatment centers [2,3].
PIVC is one of the high-risk procedures performed by physicians, nurses and paramedics. Because it is such a common procedure, it is easy to forget the potential for serious complications and safety risks to the patient, as well as to the medical staff. Complications range from bruising to bacterial infection, extravasation, phlebitis, thrombosis, embolism and nerve damage. Unsuccessful PIVC can lead to more invasive procedures resulting in infection and requiring higher operator skills (e.g. central line placement, peripherally inserted central catheters and more) [2]. Lawsuits against nurses involving short peripheral catheter placement resulting in patient injuries are increasing, with a reported average paid indemnity of over $100,000. Reports of increased blood occupational exposure during placement of short peripheral catheters are well-documented [4].
This article reviews the scientific literature on the strategies developed to overcome difficult peripheral intravenous accesses (DPIV) and summarizes the features and applications of devices that have been or are being developed to decrease the difficulty of the procedure. The physical principle for each application is also described. TABLE 1 summarizes the advantages and disadvantages as well as the cost of devices for each technology.
| Method | Color Visiona | Pressure Sensor | LED | Infrared | Ultrasoundb | Multi-spectralc |
|---|---|---|---|---|---|---|
| Pros | Simple No battery No electricity Suitable for outdoor light Portabale Wearable |
Simple Fast Detection For use in every enviorment |
Simple Portabale Various wavelengths Veins depth and diameter can be evaluated Keep the vein from rolling |
Various wavelengths Vein map shows on the skin Up to 15mm depth No patient contact Works in light or dark |
Large screen Can see the needle inside the body Needle guide device Vein depth and diameter can be estimated Very deep peneterating |
Multispectral camera Ultrasound Real-time sharing Portabale No patient contact Wearable |
| Cons | Will not work in the dark Not for the colorblind |
No image No visability improvment |
Need a dark environment Many kinds of products Requires patient contact |
Vein depth and diameter can be estimated Requires practical training |
Not portable Expensive Complicated Requires practical training |
Heavy (300gr without battery) Requires practical training |
| Price [USD] | ~300 (for glasses or bulb) | 120 | 200-630 | ~27,000 not portable/4,500 portable | ~27,600 | ~10,000 |
| % of Improved PDVA | ~91% | 80% | 93% | 93% |
bThe price is for a specific designated ultrasound machine. The price of an ordinary ultrasound machine starts from 20,000 USD
c The success rates for the multispectral glasses are not presented because they only recently came on the market
Table 1: Advantages, disadvantages and costs for each technology.
■Slapping the skin
Gently slapping the skin, this must not be too firm to avoid pain that can cause a vasoconstriction reflex.
■Tourniquet
Prolonged application of a tourniquet and repeated gripping and relaxing of the hand. Since a tourniquet reduces the number of superficial veins while allowing blood flow through the arteries, the additional blood left in the veins is more prominent. Gripping and relaxing the hand stimulates the blood to pass despite the resistance from the tourniquet.
■Negative pressure
Vacuum around the limb. The device consists of a plastic film-covered cardboard mailing tube that can be placed over the forearm. A rubber sleeve is attached to the distal end and forms a seal after a blood pressure cuff is wrapped around the sleeve and the upper arm. A rubber squeeze bulb attached to the distal end of the device is used to generate a vacuum within the device. Compression must be sufficient to restrict venous outflow and permit arterial inflow in order to maintain control of outflow occlusion. The cuff serves as a tourniquet.
■Warming the area
Warming the area with pads soaked in warm water, or immersing the limb in warm water increases local blood flow that enhances venous distension.
■Application of alcohol
■Application of alcohol Alcohol or betadine swabs, which change the reflection of light on the skin (particularly helpful in dark-skinned patients).
■Vasodilatation pastes
Vasodilatation pastes are smeared on the skin. These pastes contain Magnesium sulphate glycerin paste, magnesium soaked sponge and nitroglycerin paste (not to be used in patients with heart problems).
New techniques and devices for locating veins
■Color vision
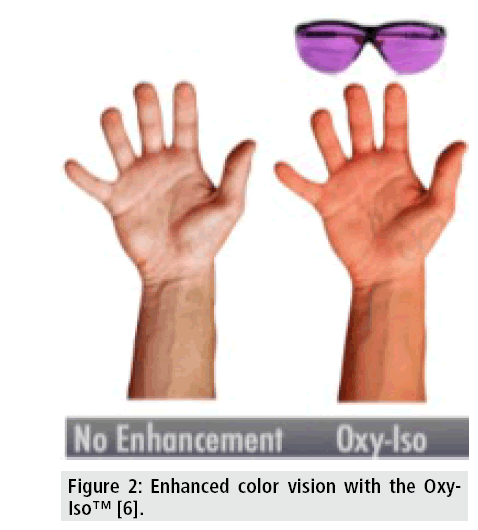
This modality is especially helpful for redgreen colorblindness. Medical staff relies on color vision for diagnosing and vein localization, but red-green colorblindness robs them of the ability to see veins, vasculature, blood in excretions, and other important signs and symptoms. Based on the property of blood to change color with variations in oxygenation, the Oxy-Iso (O2Amp™ Company) filter, which isolates and amplifies the red-green color of the oxygenation signal, was developed (FIGURE 2). Filtered glasses and LED bulbs that fill the workspace with Oxy-Iso light [6] serve this purpose.
■Ultrasound (US)
Two approaches to the use of ultrasonic waves to enhance visualization of the vasculature underlying the skin have been described: USguided PIVC and Doppler US.
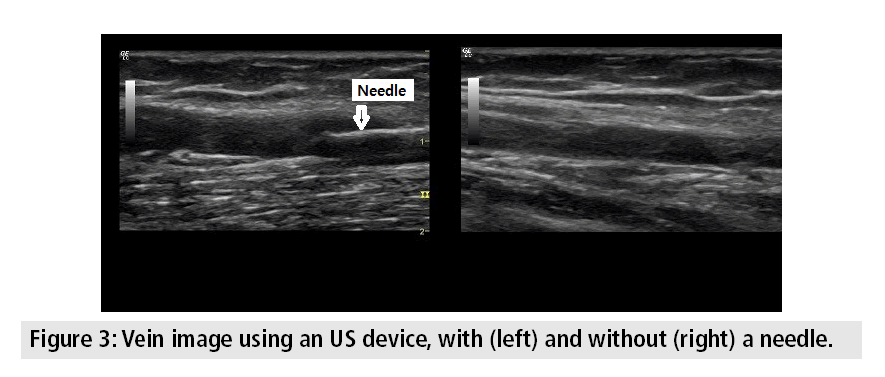
US-guided PIVC can be very effective when performed by an experienced individual, but the small size and depth of the vessels make the procedure quite challenging. Success rate of this method depends on the preferences of the technician. US guidance is done using longitudinal view of the vein. A transversely oriented 7.5 MHz linear transducer is helpful in locating superficial veins. In a dedicated instrument, a guide directs the needle to the target vessel by pointing it toward the US beam. The medical staff performing the procedure looks at the picture presented on the screen instead of the patient [7]. Insertion under US guidance has been reported to increase success by as much as 97% in adults, while its use in children achieves successful insertions and complication rates of infusion therapy that are statistically similar to those achieved with the standard method [8]. A practical picture as shown on the US screen is presented in FIGURE 3.
The second approach, Doppler US, is based on the principle that ultrasonic waves reflected from blood vessels have different frequencies than those transmitted, according to the Doppler Effect (blood is a moving substance while skin and tissue are static), and therefore provide critical 3D information about a vein’s location. As the Doppler US device moves along the patient’s arm, the transducer emits a thin acoustical beam into the skin and to the reflector, which directs the US waves into the patient’s skin at a slight angle. The device can determine the direction of blood flow (to or from the heart) to distinguish arteries from veins. When the device detects a vein, an alarm is triggered and the needle is inserted [9]. This technique, which is still in development stage by a team of Georgia Institute of Technology researchers [9], addresses a number of challenges. Unlike large US systems employed by hospitals for general blood flow studies, the vein finder based on Doppler US targets a very small area of the body. Because the acoustical beam has to be small, in accordance with the small body area being targeted, only a small amount of energy, about 1/10,000 of transmitted waves, is scattered off the vein, limiting how much energy can be put in and how much can be picked up. These considerations, plus the high cost and small size of the instrument, restrict the company to a single sensor, which limits the type of signal processing that can be implemented in order to eliminate the scattering effects.
■Near infrared (NIR) spectroscopy
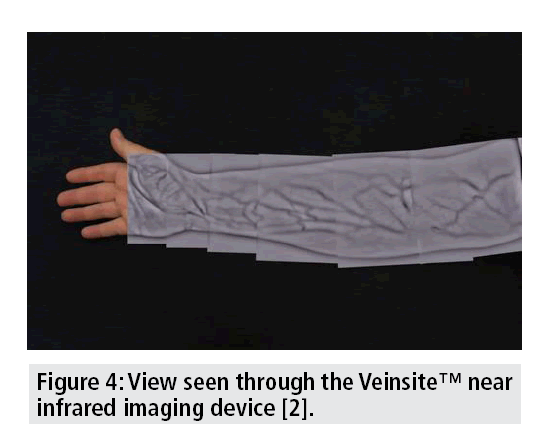
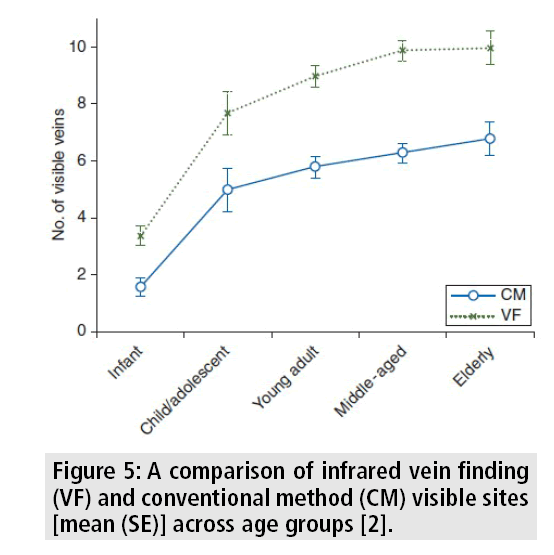
A NIR technology device emits radiation (range 700-900 nm) that penetrates human anatomy deeper than visible light (400-700 nm). Since hemoglobin and other vascular fluids are highly absorptive, electro-optical technology can detect the absorption difference between vascular structures and surrounding tissue. The processed image of the patient's superficial vein pattern can be projected back onto the skin surface in real time (FIGURE 4), providing the user with a near real time, enhanced video of the vascular system. A 97% increase in the detection of possible intravenous catheterization sites in difficult cases has been reported with NIR technology [2]. The mean number of visible sites that were found across all age groups without any vision assistance increased with the infrared vein finding (VF) device (FIGURE 5) [2]. A vision system providing multispectral images in the NIR and visible spectrum, associated with 3-dimensional information of the arm topography, yield reliable results for automatic vein detection [10].
■Visible light transilluminator
This simple technology is based on LED (light emitted diode) light waves that penetrate tissue, are absorbable by hemoglobin, and are visible to the human eye. The skin reflects the short-wavelength light (blue and green) and absorbs the long-wavelength light (orange and red). The intensity of the light reflected from the surface of the skin overpowers the transmitted light, limiting the naked eye's visualization of superficial veins. Reflected light is reduced and deeper veins visualization is increased by applying LED light waves, which are easily absorbed by deoxygenated hemoglobin in venous blood and show up as dark areas on the skin. An improvement to this method, sidetransillumination, uniformly transilluminates a small region of the skin to obtain better imaging of veins without shadows, and enables penetration of light into tissue for vein imaging up to 6 mm in depth, depending on the size of the vein [11].
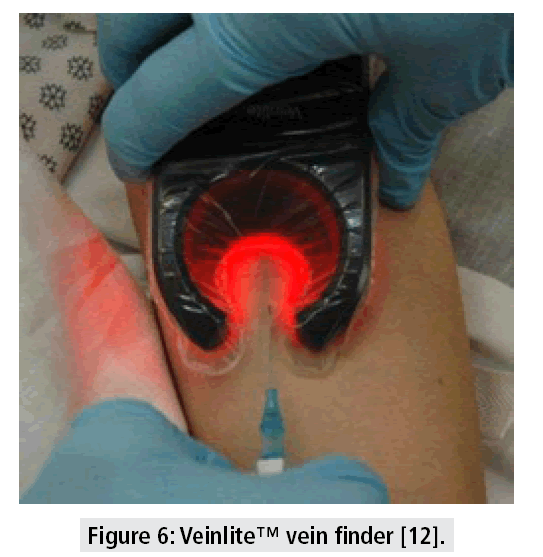
Some devices, like the one shown in FIGURE 6, use side-transillumination to transmit a circular array of bright LED light inclined inwards at an angle, such that the light is focused towards the center of the circle and below the surface of the skin, creating a virtual light source under the skin. This technique achieves uniform transillumination of a small region of tissue and enables visualization of peripheral veins. Most devices are portable and work on batteries and are operable only in a dark room. A clinical study with one such a device, the Veinlite™ vein finder, reported an accuracy of 85% compared to 74% with the standard method [12]. This technology is particularly effective in children, and models have been developed for specific applications, including emergency, oncology and radiology purposes.
■Pressure sensor
The Vein Entry Indicator Device (VEID™, Vascular Technologies Ltd.) designed to assist PIVC consists of a plastic box weighing 8.5 g containing a pressure sensor, a signal indicator and a processing unit. The pressure sensor, which has operating pressures of 5-100 cm H2O, detects pressure changes when the vein is entered, emitting a beep within 0.1 sec to alert the operator to stop advancing in order not to puncture the back wall of the vein. The VEID alerts the operator when there is doubt about the location of the needle tip. This small device, approved by the FDA, attaches to any female Luer Lock IV catheter. VEID increased the success rate in children from 70% to 90% and in adults with difficult veins from 26% to 90% [13]. The method does not improve vein visibility, but insertion is faster and more accurate.
■Multispectral camera
Multispectral imaging involves collecting data from two or more ranges of frequencies along the spectrum. Eyes-on™ glasses use multispectral light-based technology for imaging most peripheral veins [14]. A builtin computer integrates the images generated using four different wavelengths, including the near infrared part of the spectrum. While the computer projects a 3D view of the vasculature onto the clear lenses of the glasses, wearers can still look past the transparent vein map before their eyes to see what is going on in the room. The glasses include 3D imaging, wireless connections, digital storage and interfaces with hospital electronic medical records systems for seamless documentation. An accessory to the device uses US to reveal veins located farther beneath the skin surface. The same technology with an exceptionally strong lens system and convenient adaptations to field conditions is used in the military. Critical patient information is obtainable with eye movement downward [14-16].
■Robotics systems
Efforts have been made recently to develop robotic systems for PIVC and drawing blood but none have reached the market. The system, as described in one such study [17], operates as follows: The patient slides his or her arm into an inflatable cuff, which acts as a tourniquet. An infrared light illuminates the inner elbow for a camera that searches for a suitable vein using software that compares the camera’s view with a model of the veins of the arm. Once sufficient blood flow in the chosen vein is confirmed by US wave, the robotic arm aligns itself with the chosen vein and inserts the needle.
Another innovative system, in development phase, SAGIV™, is a semi-automatic guided intravenous device (FIGURE 7). Using infrared technology and an online LCD monitor, the SAGIV enables operators to identify appropriate veins for cannulation, and on demand automatically inserts the needle and cannula. Using an electrical feedback, the device precisely penetrates the vein and ensures appropriate catheter positioning. Once the catheter is in place, the SAGIV removes the needle to an easily discarded sealed housing [18,19].
Discussion
The wide variety of devices designed for locating veins reflects the great challenges of this procedure. Unfortunately, they are rarely seen in clinics, probably because of economic constraints, hospital politics, conservative medical staff, or simply a lack of awareness of both their existence and advantages. Despite their availability, valuable time and money continue to be wasted and people continue to suffer multiple needle stickings. Clinicians face difficulties in locating peripheral veins on a regular everyday basis. They usually start with the basic simple techniques of milking, slapping, and tourniquet. Recurrent failures are helpful in identifying persons who need additional extra help to be cannulated. Based on our experience with some of the new vein locating techniques, we believed that these technologies would lead to better performance during the first attempt.
All existing methods, without exception, increased success rates for locating veins for PIVC, particularly in difficult cases. Adoption of these advanced technologies may lead to improved medical treatment, as well as prevent clinical complications such as hematomas. All methods save critical time and improve both medical staff and patient satisfaction. The mobile devices offer solutions to overcome obstacles, drive down costs, redesign care-paths and processes, augment the level of patient safety and significantly improve the quality of care in diverse care settings, including hospital wards, emergency rooms, field hospitals, the military and homes [20]. It could also be very useful and effective for patients that inject their medicine straight into the veins themselves (such as hemophiliacs).
Many of the technologies have different versions of their product tailored to the specific needs of the users. Devices are chosen according to specific working environments. Emergency medicine requires devices that are portable, easy and fast to operate, and can work in any lighting conditions. The most suitable ones are the pressure sensor, which is light in weight, and easy to operate; NIR devices, which can be portable and can work in any lighting condition; and a multispectral device whose military version is portable, can work in any lighting condition, and has strong lenses to accommodate extreme weather. Less suitable devices for emergency medicine are the color vision glasses and LED technology, both which require controllable lighting conditions. The same holds for the common US machines, which in addition are large and heavy. In hospitals, where lighting conditions are controllable and mobility is unnecessary in most departments, each of the technologies described above is suitable, including the innovative robotics devices under development. The eventual availability of these devices will enable practitioners to obtain a more accurate picture and better understanding of the region of interest, automate the detection and cannula insertion process so as to avoid complications, and enable even the novice to perform the procedure [21]. Combining digital data storage with vein view technologies will enable the medical staff to share and consult with colleagues, and build a database of the associated successes, difficulties and complications.
It is also important to adopt the technology suitable to the population of patients. LED technology is better for small children, while US is more suitable for obese people. Finally, price must be taken into account, with devices ranging from 120 USD to over 27,000 USD (TABLE 1).
Conclusion
The use of the advanced technologies in future medical treatments replace subjective with objective measurements, can improve PIVC success rates and minimize the impact of medical staff's expertise level on the procedure result. Embracing these technologies for routine use can save critical treatment time in emergency rooms as well as on the battlefield, and reduce expenses. It can also lead to greater satisfaction of both medical staff and patients in the clinic as well as in homecare.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- RiveraA, StraussK, ZundertAet al. Matching the peripheral intravenous catheter to the individual patient. Acta. Anaesth. Belg. 58, 19-25 (2011).
- ChiaoF, Resta-FlarerF, LesserJet al. Vein visualization: Patient characteristic factors and efficacy of a new infrared vein finder technology Br. J. Anaesth.110, 966–971 (2013).
- GuillonP, MakhloufiM, Baillie S et al. Prospective evaluation of venous access difficulty and a near-infrared vein visualizer at four French haemophilia treatment centres. Haemophilia. 2,121–126 (2015).
- VizcarraC, CassuttC, CorbittN et al. Recommendations for improving safety practices with short peripheral catheters. J. Infus. Nurs. 37, 121-124 (2010).
- MbamaluD, BanerjeeA. Methods of obtaining peripheral venous access in difficult situations. Postgrad. Med. J. 75, 459-462 (1999).
- ChangiziB. The first eyewear and light-filtering technology designed for seeing people. (2012).
- American Institute of Ultrasound in Medicine, AIUM Practice Guideline for Use of Ultrasound to Guide Vascular Access Procedures, White Paper 2012 (2013).
- AvelarA, PeterliniM, PedreiraM. Ultrasonography-guided peripheral intravenous access in children: A randomized controlled trial. J. Infus. Nurs. 38, 320-327 (2015).
- BeckerTJ. Moving the needle.Res. Horizons. 23, 28-29 (2005).
- PaquitV, TobinK, Price J et al. 3D and multispectral imaging for subcutaneous veins detection.Opt. Express. 17, 11360-11365 (2009).
- LindseyJ. No More Stab-in-the-Dark IV Sticks!JEMS. 90 (2005).
- KatsogridakisY, SeshadriR, SullivanCet al. Veinlitetransillumination in the pediatric emergency department: A therapeutic interventional trial Pediatric.Emerg. Care. 24, 83-88 (2008).
- SimhiE, KachkoL, BruckheimerEet al. A vein entry indicator device for facilitating peripheral intravenous cannulation in children: A prospective, randomized, controlled trial.Anesthesia and Analgesia. 107, 1531-1535 (2008).
- PedulliL. Move over Google glass: Evenaunveils eyes-on imaging system.(2013).
- ShahzadA, SaadM, Walter N et al. Hyperspectral venous image quality assessment for optimum illumination range selection based on skin tone characteristics. Biomedical. Engineering. Online. 13, 109 (2014).
- MearianL. Smart glasses let nurses see veins through skin (2013).
- ZivanovicA, DaviesB. A robotic system for blood sampling, IEEE transactions on information technology in biomedicine: A publication of the IEEE Engineering in Medicine and Biology Society. 4, 8-14 (2000).
- Yissum. The Hebrew University of Jerusalem, SAGIV (Automated IV), Summary of the technology. (2013).
- The Hebrew University of Jerusalem, SAGIV (Automated IV), Executive summary.(2013).
- JuricS, FlisV, DebevcMet al. Towards a low-cost mobile subcutaneous vein detection solution using near-infrared spectroscopy.Scientific. World. J. (2014).
- ScalesK. Vascular access: A guide to peripheral venous cannulation. Nursing standard: Official newspaper of the Royal College of Nursing.19, 48-52 (2005).