News and Views - Imaging in Medicine (2013) Volume 5, Issue 5
PET/CT proves more accurate than marrow biopsy in diagnosis and prognosis of lymphoma patients Growing use of MRI in breast cancer correlates with increased use of invasive surgery
Abstract
PET/CT proves more accurate than
marrow biopsy in diagnosis and
prognosis of lymphoma patients
Source: Berthet L, Cochet A, Kanoun S et al. In newly diagnosed diffuse large b-cell lymphoma, determination of bone marrow involvement with 18F-FDG PET/CT provides better diagnostic performance and prognostic stratification than does biopsy. J. Nucl. Med. 54(8), 1244–1250 (2013).
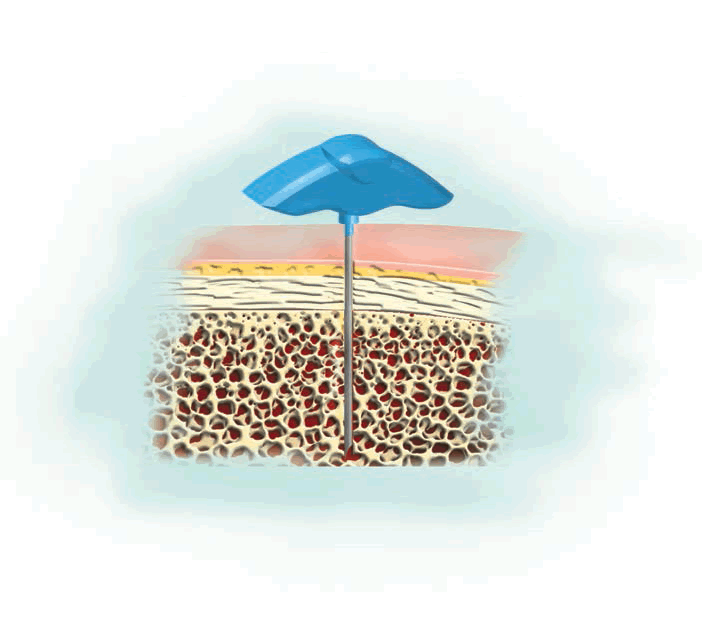
A recent study published in the Journal of Nuclear Medicine reported that imaging with 18F-fluorodeoxyglucose (FDG) PET/CT was more accurate, demonstrated a higher negative predictive value and was more sensitive than bone marrow biopsy, the current gold standard, for determining bone marrow involvement in sufferers of diffuse large B-cell lymphoma, a key factor in determining treatment strategy.
The retrospective study, carried out at the Center Georges-François Leclerc (Dijon, France), included 133 patients referred to the center between June 2006 and October 2011. All patients received both a whole-body PET/CT scan and a bone marrow biopsy to determine marrow involvement. A final diagnosis of bone marrow involvement was made if the biopsy was positive, or if a positive PET/CT result was subsequently confirmed by guided biopsy, targeted MRI or the concomitant disappearance of focal bone marrow uptake with that of uptake in other lymphoma lesions on PET/CT monitoring. Progression-free survival and overall survival were then analyzed.
A total of 33 patients exhibited bone marrow involvement; of these, eight were identified by biopsy and 32 were identified by 18F-FDG PET/CT. PET/ CT was more sensitive (94 vs 24%; p < 0.001), demonstrated a higher negative predictive value (98 vs 80%) and was more accurate (98 vs 81%) than the biopsy procedure. Of 24 patients with a positive PET/CT but negative biopsy for bone marrow involvement, 11 were re-evaluated as stage IV, which resulted in a revision of their treatment plans. Furthermore, PET/CT was also determined to be an independent predictor of progression-free, although not overall, survival.
Louis Berthet, the lead author, commented: “In our study, we showed that in diffuse large B-cell lymphoma, 18F-FDG PET/CT has better diagnostic performance than bone marrow biopsy to detect bone marrow involvement and provides a better prognostic stratification. While bone marrow biopsy is considered to be the gold standard to evaluate bone marrow involvement in high-grade lymphomas, 18F-FDG PET/CT is in fact the best method to evaluate extension of the disease, as well as avoid invasive procedures.” He added, “Our findings add to the literature to prove the significance of 18F-FDG PET/CT in cancer evaluation and to democratize this imaging method. Molecular imaging is the best method to adapt targeted therapies to each patient. The emergence of PET/MRI and novel radiotracers predicts an exciting new future for our field.”
Growing use of MRI in breast cancer correlates with increased use of invasive surgery
“…undergoing preoperative MRI significantly increases the likelihood of subsequent mastectomy rather than breast-conserving surgery…”
Yale School of Medicine researchers have reported that increased use of preoperative MRI in older women is correlated with an increased use of mastectomy versus breastconserving surgeries, describing the data as ‘concerning’.
The study, published in Breast Cancer Research and Treatment, collected data on 72,461 women between the ages of 67 and 94 years who underwent surgery for breast cancer between 2000 and 2009. Only 10.1% of the total cohort underwent MRI, but in the period investigated preoperative MRI usage rose from 0.8% in 2000–2001 to 25.2% in 2008–2009. After controlling for clinical and demographic factors, the authors report that undergoing preoperative MRI significantly increases the likelihood of subsequent mastectomy rather than breastconserving surgery (adjusted odds ratio: 1.21; 95% CI: 1.14–1.28). Among those women who underwent mastectomy, preoperative MRI is significantly associated with an increased likelihood of bilateral cancer diagnosis and undergoing bilateral mastectomy than non-MRI counterparts (9.7 vs 3.7% and 12.5 vs 4.1%, respectively; p < 0.001 for both).
“These data are concerning because the long-term benefits associated with bilateral mastectomy for older women with breast cancer are unclear,” commented the study’s lead author Dr Cary Gross. “Patient concern about recurrence and survival must be balanced with the increased risk for complications associated with more aggressive cancer surgery, particularly when there is no proven benefit of the more aggressive option.”
“There has been no randomized controlled clinical trial demonstrating improved outcomes for women who undergo preoperative breast MRI at any age,” said Dr Brigid Killelea, first author on the study. “Breast conserving therapy, when feasible, remains the preferred approach for women with early stage breast cancer.”
Source: Killelea BK, Long JB, Chagpar AB et al. Trends and clinical implications of preoperative breast MRI in Medicare beneficiaries with breast cancer. Breast Cancer Res. Treat. doi:10.1007/ s10549-013-2656-1 (2013) (Epub ahead of print).
New MRI technique reveals brain tumor vascular response to chemotherapy
“…vessel architectural imaging may also help to further current understanding of how antiangiogenesis treatments exert their effects.”
A new method for analyzing MRI data has demonstrated promise in identifying tumor response to antiangiogenesis therapy, providing a potential novel source of information for physicians deciding upon treatment strategies. The study, published in Nature Medicine by researchers from the Massachusetts General Hospital (MA, USA), reports that changes in the vascular architecture of brain tumors could be discerned just days after the initiation of anti-angiogenesis treatments using the technique, termed vessel architectural imaging (VAI).
“Until now the only ways of obtaining similar data on the blood vessels in patients’ tumors were either taking a biopsy, which is a surgical procedure that can harm the patients and often cannot be repeated, or PET scanning, which provides limited information and exposes patients to a dose of radiation,” commented Kyrre Emblem of the Martinos Center (MA, USA), lead author of the report. “VAI can acquire all of this information in a single MR examination that takes less than 2 min and can be safely repeated many times.”
As well as holding promise for less invasive diagnostic techniques of therapeutic efficacy VAI may also help to further current understanding of how antiangiogenesis treatments exert their effects and which patients will benefit from them. Previously, trials in animals and humans have demonstrated that antiangiogenesis treatments work by normalizing compromised blood vessels in the tumor, stabilizing leaky vessels to allow increased blood perfusion throughout the tumor and thus improving the efficiency of chemotherapy or radiation treatment. In glioblastoma, the tumor type imaged in this study, investigators from the Massachusetts General Hospital found that antiangiogenesis treatment alone significantly extended the lifespan of some patients. In the current report the team used VAI to investigate the changes that occur as a result of antiangiogenesis treatment and which patients benefit.
Of 30 patients who received cediranib and whose data were analyzed, ten were true responders, exhibiting significant positive alterations in vascular architecture, 12 displayed worsening of their condition and were classed as nonresponders and the remaining eight patients’ data suggested only stabilization of the tumor. Patients who responded to the treatment survived 6 months longer than their nonresponding counterparts. Emblem notes that “quickly identifying those whose tumors don’t respond would allow discontinuation of the ineffective therapy and exploration of other options.”
Senior author Gregory Sorensen explains: “One of the biggest problems in cancer today is that we do not know who will benefit from a particular drug. Since only approximately half the patients who receive a typical anticancer drug benefit and the others just suffer side effects, knowing whether or not a patient’s tumor is responding to a drug can bring us one step closer to truly personalized medicine – tailoring therapies to the patients who will benefit and not wasting time and resources on treatments that will be ineffective.”
Looking to the future, Emblem and colleagues are now exploring whether VAI can be used to determine patients who will, or will not, respond to a drug before therapy is begun, potentially eliminating futile treatment regimens.
Source: Emblem KE, Mouridsen K, Bjornerud A et al. Vessel architectural imaging identifies cancer patient responders to anti-angiogenic therapy. Nature Med. doi:10.1038/nm.3289 (2013) (Epub ahead of print).
“…knowing whether or not a patient’s tumor is responding to a drug can bring us one step closer to truly personalized medicine…”
About the News and Views
The News and Views highlights some of the most important events and research in the field of imaging in medicine. If you have newsworthy information, please contact: Jonathon Wilkinson, Commissioning Editor, Imaging in Medicine, j.wilkinson@futuremedicine. com
Next-generation PillCam® receives US FDA clearance
Given Imaging (Yoqneam, Israel) has announced that the US FDA has approved the PillCam® SB3 (Given Imaging) for the detection and monitoring of small bowel problems, such as Crohn’s disease. The device, which should be available in the USA at the beginning of October, weighs less than 4 g and measures 11 × 26 mm, building on the success of its predecessor, PillCam SB. According to the company, the SB3 boasts a 30% improvement in image quality and a 40% increase in video processing.
CEO and President of Given Imaging, Homi Shamir, explained: “With more than 2 million procedures conducted since the first generation of the product was introduced, PillCam SB has had a significant impact on patient care in the US and across the globe. We believe PillCam SB3 will both enhance the clinical experience for our large base of existing US customers and expand the market for this product among new physicians who have not been performing PillCam procedures.”
“Our goal as we set out to reimagine and improve the PillCam platform was not just to provide physicians with more information, but to provide them with better and more actionable information. By delivering more detail, more coverage and improving the overall efficiency of our technology platform, we have achieved this with PillCam SB3.”
However, while the benefit for physicians is undoubted, there is also an advantage to using this technology for patients, as Felice H Schnoll-Sussman, Director of the Jay Monahan Center for Gastrointestinal Health (NY, USA) explains: “Patients with complicated diseases involving the small bowel, such as Crohn’s disease, often struggle to comprehend what is happening inside their bodies and how it can be better managed. The improved image resolution and overall efficiency of the PillCam SB3 system in capturing and analyzing images of the small bowel has potential to have a meaningful impact on patient care.”
Overall, the wider availability of this technology has the potential to improve diagnosis and patient understanding in a range of small bowel abnormalities, including Crohn’s disease, gastrointestinal bleeding and anemia.
Source: Improved PillCam® SB technology provides a more detailed and efficient small bowel examination for patients with conditions such as Crohn’s disease and obscure GI bleeding. Given Imaging press release: http://phx.corporate-ir. net /phoeni x .zhtml?c=130061&p = irol - newsArticle&ID=1847080&highlight
– All stories written by Adam Born


